Gopal Addresses Differences Between Real-World and Clinical Trial Data for DLBCL
During a Targeted Oncology case-based roundtable event, Ajay K. Gopal, MD, discussed the options for second-line and subsequent treatment of a patient with relapsed/refractory diffuse large B-cell lymphoma who refuses CAR T-cell therapy.
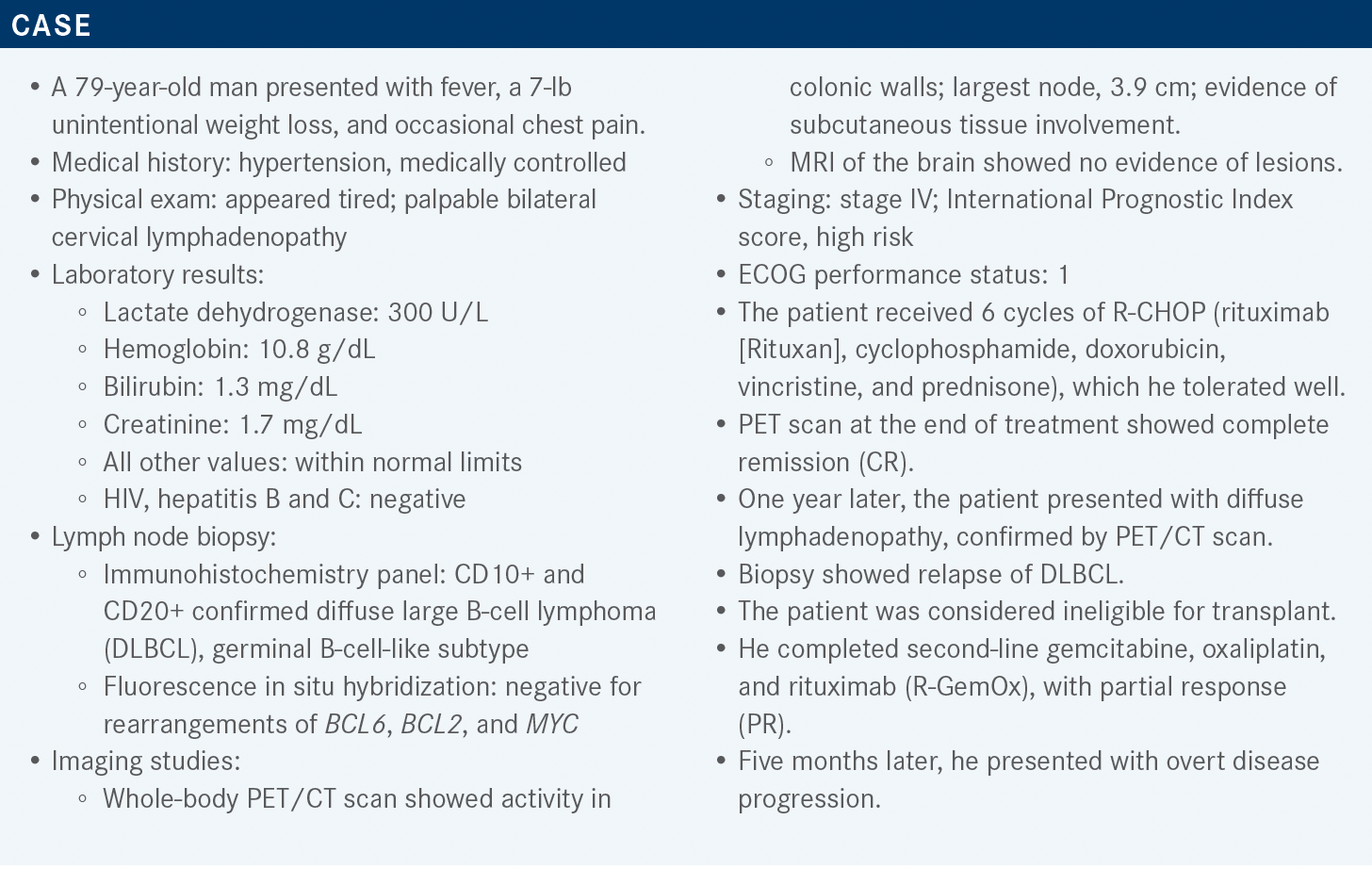
Ajay K. Gopal, MD
Medical Director of Clinical Research, Hematology, Malignancies/ Hematology
Seattle Cancer Care Alliance
Professor, Division of Medical Oncology, University of Washington School of Medicine
Professor, Clinical Research Division, Fred Hutchinson Cancer Research Center

Targeted OncologyTM: What are the recommended approaches for relapsed/refractory DLBCL in the second-line and subsequent therapies settings?
GOPAL: What the NCCN [National Comprehensive Cancer Network] guidelines have for second-line therapy in nontransplant candidates is basically a dealer’s choice.1 This patient was on R-GemOx. Polatuzumab vedotin [Polivy] with bendamustine [Treanda] and rituximab [pola-BR] is also FDA approved. Others on the list are historical lymphoma regimens, many containing platinum, and then more recently, tafasitamab [Monjuvi] plus lenalidomide [Revlimid], which is approved to treat adults who are not eligible for transplant. Other regimens used in certain circumstances include brentuximab vedotin [Adcetris], a CD30-targeted agent, and bendamustine plus rituximab, ibrutinib [Imbruvica], and lenalidomide plus rituximab. For CAR [chimeric antigen receptor] T-cell therapy, we now have 3 agents approved in the third-line space.
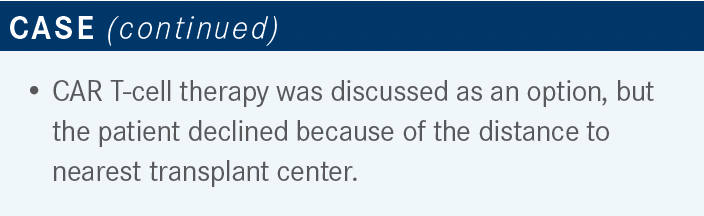
What do you think about the currently approved CAR T-cell therapies for DLBCL?
The 3 proven CAR T-cell agents for third-line therapy all have single-arm studies, but I think we all know from our practices that study data never match what we see in the clinic. My thoughts in general are that there’s more discordance between the real-world and clinical trial data because the histology in real-world data tumors is more aggressive. The studies put all these little things like you have to do X, Y, and Z, but then you’re weeding out all the patients with explosive disease and you end up getting a better-risk population, so the single-arm trials are probably not the same [as clinical practice]. For axi-cel [axicabtagene ciloleucel (Yescarta)] for example, I was part of a group that put together some real-world data, and the CR rate, which was 58% in the trial, was 42% for our study-ineligible patients.2
The median progression-free survival [PFS] was only 3 months if you were fit enough to get axi-cel, but you wouldn’t have met the eligibility criteria.2 Stephen D. Smith, MD, from the Seattle Cancer Care Alliance looked at the eligibility criteria for patients who had 2 prior lines of therapy, and none of them got CAR T-cell therapy, but just meeting the eligibility to ZUMA-1 trial [NCT02348216] gave a statistically significant improved survival advantage. We never get the same results of the trial for off-trial patients, and they are probably not quite as good as what these studies tell us.
How many patients were included who had transformed follicular lymphoma (FL)?
[Sixteen patients had transformed FL]. Axi-cel has a label for transformed FL and liso-cel [lisocabtagene maraleucel (Breyanzi)] has a label for any transformed, including DLBCL arising from indolent lymphoma. But my sense is that these patients don’t do worse. Sometimes, they’ve had more lines of therapy, which might impact their tolerability, or they’ve had many lines through their FL, then they transform and get CAR T-cell therapy. For straight-up FL, there are also published data supporting a label for 2 prior lines for axi-cel as well, but we’re not using it for many of those cases.
What are the toxicity profiles of CAR T-cell agents?
Generally, we think that axi-cel probably has a little more toxicity, both for cytokine release syndrome [CRS] and neurotoxicity.2 We don’t have much real-world data for the other constructs yet, but at least the studies suggest they’re a little better tolerated for neurotoxicity and CRS.3,4
What data led to the approval of pola-BR for third-line therapy for relapsed/refractory (RR) DLBCL?
The study that got pola-BR approved [NCT02257567] was designed as a randomized phase 2 trial, so it does give you a sense of the relative benefit of adding BR, which may not have been the first thing we pull off the shelf anyway for RR DLBCL. The eligibility criteria were adults with a confirmed biopsy, at least 1 prior line of therapy, ECOG performance status of 0 to 2, and grade 1 or less peripheral neuropathy, and either transplant ineligible or failed prior autologous stem cell transplant [ASCT].5
[For the exclusion criteria], the patients did not have an allogeneic transplant or ASCT within 100 days, did not have transformed disease, and were transplant ineligible. The 2 arms were BR vs pola-BR with 2 patient groups with FL and DLBCL. The patients with DLBCL were given the regimen on a 21-day cycle vs a 28-day cycle for FL. The polatuzumab dose was 1.8 mg/kg intravenously.
The median for the prior lines of [therapy for both arms] was 2. Most patients had a duration of response to last prior therapy of less than 1 year or refractoriness to last prior therapy, which by definition in this trial, was less than a PR or relapsed within 6 months. It’s not a huge surprise that this is the case with DLBCL, but the majority had refractory disease to the last therapy and minority had prior stem cell transplant.
The primary end point was objective response, and one may argue that maybe that’s not the most important end point in DLBCL, but for this trial, they showed that the pola-BR improved the overall response rate [ORR] and CR rate. The ORR was 45%. Dr Smith put together a group looking at some of the real-world data, and the ORR was pretty similar.6 The CR rate was lower in the real-world pola-BR data at 24% [compared with 40% in the trial].5,6
The median PFS in the pola-BR arm from the study was 9.5 months, but the median PFS was only 2 months in the real-world data, so it’s not quite the same, but I think that’s not a surprise because of the selection criteria. I think people are probably aware of these data. So not a home run, probably, but as a stand-alone, even in the pola-BR arm, a median survival of 1 year is not fabulous.
I think this is what happens in aggressive malignancies when you don’t have study selection criteria, so what I take away from these studies is that I can’t always apply it to my patients. There is probably more benefit for pola-BR than BR, but you probably aren’t going to get on the pola-BR curve unless you have a fit patient who might have met the eligibility criteria.
The main point for adverse events [AEs] is that there was more discontinuation on the pola-BR arm of about one-third. The main AE monitored was peripheral neuropathy.5
What data led to the approval of tafasitamab plus lenalidomide?
Tafasitamab is an Fc-enhanced anti-CD19 monoclonal antibody [mAb] and is probably more similar to the way obinutuzumab [Gazyva] is optimized, so more of the Fc receptor and less of the complement fixation. We don’t exactly know how lenalidomide works, but there’s some hypothesized mechanisms. The single-arm L-MIND study [NCT02399085] led to the approval of tafasitamab plus lenalidomide.7
I would just be cautious about any single-arm studies, particularly in aggressive malignancies like DLBCL in terms of the real-world results, which we have not seen yet. The study was for patients with 1 to 3 prior regimens who were transplant ineligible. Those who were primary refractory were excluded, so they took out the highest of the high-risk group.8 I’m not being particularly critical of any agent or trial, but there is a theme of certain high-risk subsets getting excluded, but these are the ones who are the most in need.
Tafasitamab, for those who have given it, has an induction dosing at day 1, 8, 15, and 22 for the first 3 cycles, then every other week for cycle 4 through 12. It’s 25 mg per day for lenalidomide from day 1 through 21. In my experience, lenalidomide gets tougher as patients get older, and I also think it’s tougher in patients with lymphoma for some reason, than in patients with myeloma. I don’t have any myeloma cases, but it just seems that way to me. The tafasitamab continues after 12 cycles indefinitely, but the lenalidomide stops. The primary end point was ORR.
Reading the fine print of all these trials, they don’t always tell you the whole story of the patient population and who was not included. The median prior lines of therapy for the L-MIND trial were 2, so like the pola-BR trial from that perspective. A minority of patients had had a prior stem cell transplant, again like the pola-BR trial. A lower number compared with the pola-BR trial were refractory to their last prior therapy by 6 months, but it is not appropriate to compare across studies.
The CR rate was 40%, PR was 17.5%, and the median duration of response [was 43.9 months], though I’m itching to see real-world data to see if the patients were chosen in a way to get a long duration of response. I’m always skeptical of study data, my own data included.
The median PFS was about 1 year in this population, and interestingly, the overall survival [OS] was eye popping at 33.5 months.9 Again, taking care of a lot of patients with DLBCL, I just wonder who those patients were and if they are the ones we see in our clinic with explosive refractory disease. These are the data, but I think we need to see more real-world information.
What study data led to the approval of loncastuximab tesirine?
Loncastuximab tesirine [Zynlonta] is another antibody-drug conjugate. It has a different PBD [pyrrolobenzodiazepine] payload and AE profile. Polatuzumab and brentuximab have the MMAE [monomethyl auristatin E] vedotin for example, and the same general principle [applies to loncastuximab] that binds to CD19 and is internalized and causes PBD to be released, which causes DNA cross-links and eventual cell death.
The LOTIS-2 trial [NCT03589469] was, again, a single-arm trial that led to the approval of loncastuximab.10 I read the protocol before as published. So there were some little exclusions in there; for example, you couldn’t have any mass that was 10 cm or larger, so that’s a big lymphoma mass, but it still took out some patients. There were the usual things of getting 10 unstained slides and for patients that have rapidly progressive disease in whom you can’t get another biopsy, those could not go on the study. All the studies do this, so I’m just saying, it’s not real-world scenarios where you must treat people quickly.
Every 3 weeks, the patients got a dose of 150 μg/kg for the first 2 cycles, then after 2 cycles, the dose is dropped to 75 μg/kg, and they get it for up to a year. They found that by dropping this dose after the first 2 cycles, you get less AEs.11
I will give credit that this was a bit of a larger study, so 145 patients, and there were some who had double, triple, and transformed disease. They might have been a more indolent because it’s hard to get on a trial with a relapsed double-hit lymphoma that’s exploding. They had 3 prior regimens, so more lines of therapy than the other studies.
How did patients do on the LOTIS-2 trial?
The ORR came quickly and was at 48%; half of those were PRs and half were CRs. There was a little less follow-up on this study, but the CRs, not surprisingly, were maintained. The median number of cycles to response was relatively short, at 4.5 cycles.
We always have to be cautious in interpreting subgroup analyses because these studies are not powered to show differences in these subgroups. It is not clear that any one particular group did worse, but perhaps refractory disease, not surprisingly, did worse than relapsed disease.
The most recent reported median duration of response was 13.4 months, and for those with CR it was not reached; whether this is drug related or tumor related is hard to know. A longer follow-up had similar data for the median PFS, [which was 4.9 months (95% CI, 2.9-8.3)] and median OS [was 9.9 months (95% CI, 6.7-11.5)].
For subsequent therapy, I think we don’t know the answers. My 84-year-old patient got CAR T-cell therapy after tafasitamab plus lenalidomide, and was not a transplant candidate, had basically stable disease that lasted for a few months. Then he went on a clinical trial with a bispecific antibody, which gave him stable disease, and then I referred him to get CAR T-cell therapy. He got biopsied, he still had CD19, so he got a CAR T-cell agent and got about 9 months of remission out of that.
Unfortunately, he relapsed, got re-biopsied, still had CD19, and now I’m treating him with loncastuximab. I’ve reimaged him and he has about a 40% reduction in his adenopathy, but he’s not at PR yet. A patient can get 3 lines of anti-CD19 therapy and I guess none of them completely did the trick so far, but I’m hoping we’re going to have more data in the future on this.
For loncastuximab, the protein dose is small and it’s probably related to the potency or toxicity of the payload, so you’re not getting a lot of antibody dose there, for what it’s worth. Peripheral edema is the main thing to watch for, and it tends to kick in later, after about cycle 3. I’ve talked to folks from the company to try to find what’s the mechanism.
I don’t think anybody completely understands it. It’s related to the payload, presumably, but patients get peripheral edema, and pre-treatment with steroids seems to help some.10 My patient is not having any issues with edema, but he’s getting a little bit of borderline neutropenia and the absolute neutrophil count is around 1100.
If you use this drug, it’s important to be aware of the peripheral edema and the dexamethasone premedication for a few days prior, but that’s sometimes tougher than the chemotherapy, especially in older patients.
REFERENCES
1. NCCN. Clinical Practice Guidelines in Oncology. B-cell lymphomas, version 5.2021. Accessed February 15, 2022. https://bit.ly/3geoS5N
2. Locke FL, Ghobadi A, Jacobson CA, et al. Long-term safety and activity of axicabtagene ciloleucel in refractory large B-cell lymphoma (ZUMA-1): a single-arm, multicentre, phase 1-2 trial. Lancet Oncol. 2019;20(1):31-42. doi:10.1016/S1470-2045(18)30864-7
3. Schuster SJ; JULIET Investigators. Tisagenlecleucel in diffuse large B-cell lymphoma. N Engl J Med. 2019;380(16):1585-1586. doi:10.1056/ NEJMc1901464
4. Abramson JS, Palomba ML, Gordon LI, et al. Lisocabtagene maraleucel for patients with relapsed or refractory large B-cell lymphomas (TRANSCEND NHL 001): a multicentre seamless design study. Lancet. 2020;396(10254):839-852. doi:10.1016/S0140-6736(20)31366-0
5. Sehn LH, Herrera AF, Flowers CR, et al. Polatuzumab vedotin in relapsed or refractory diffuse large B-cell lymphoma. J Clin Oncol. 2020;38(2):155-165. doi:10.1200/JCO.19.00172
6. Smith SD, Lopedote P, Samara Y, et al. Polatuzumab vedotin for relapsed/ refractory aggressive B-cell lymphoma: a multicenter post-marketing analysis. Clin Lymphoma Myeloma Leuk. 2021;21(3):170-175. doi:10.1016/j. clml.2020.12.013
7. FDA grants accelerated approval to tafasitamab-cxix for diffuse large B-cell lymphoma. FDA. Updated August 3, 2020. Accessed February 15, 2022. https://bit.ly/3bodb9v
8. Salles G, Duell J, González Barca E, et al. Tafasitamab plus lenalidomide in relapsed or refractory diffuse large B-cell lymphoma (L-MIND): a multicentre, prospective, single-arm, phase 2 study. Lancet Oncol. 2020;21(7):978-988. doi:10.1016/S1470-2045(20)30225-4
9. Duell J, Maddocks KJ, González-Barca E, et al. Long-term outcomes from the phase II L-MIND study of tafasitamab (MOR208) plus lenalidomide in patients with relapsed or refractory diffuse large B-cell lymphoma. Haematologica. 2021;106(9):2417-2426. doi:10.3324/haematol.2020.275958
10. FDA grants accelerated approval to loncastuximab tesirine-lpyl for large B-cell lymphoma. FDA. Updated April 23, 2021. Accessed February 15, 2022. https://bit.ly/36j4ca3
11. Caimi PF, Ai W, Alderuccio JP, et al. Loncastuximab tesirine in relapsed or refractory diffuse large B-cell lymphoma (LOTIS-2): a multicentre, open-label, single-arm, phase 2 trial. Lancet Oncol. 2021;22(6):790-800. doi:10.1016/ S1470-2045(21)00139-X




















