Dosing and Toxicity: Management of Tyrosine Kinase Inhibitors for Third-Line RCC Therapy
During a live, virtual event, Thomas Hutson, DO, PharmD, discussed the case of a 54-year-old man with a history of metastatic renal cell carcinoma.
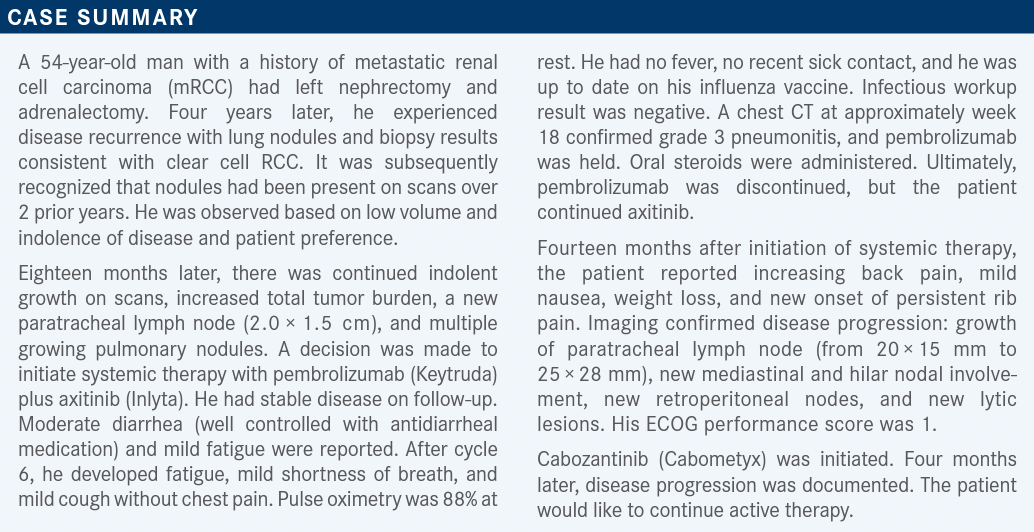
Targeted OncologyTM: How does the mechanism of action of VEGF receptor tyrosine kinase inhibitors (TKIs) relate to their efficacy in patients with RCC?
HUTSON: I’ve always spoken to these therapies as generational, where we had our first-generation drugs, sunitinib [Sutent] and sorafenib [Nexavar]. We moved into our second and third generations, and with the higher-generation drugs, it has resulted in, in some regards, new receptors.
In the case of cabozantinib and lenvatinib [Lenvima], we know that they target other factors that are important in angiogenesis: FGF, c-MET, and AXL as well as those that are upregulated at times of progression.1 They work on what’s called angiogenic escape, and they work in resistance pathways, so that’s why we think they have unique benefit. Also, [efficacy is based] on the potency of inhibiting the VEGF receptor, and we know axitinib and tivozanib [Fotivda] are the most potent VEGF inhibitors, and so they are more selective.
How do pharmacokinetics influence the toxicities associated with the TKIs?
We used to think of kinome trees, where we would look at all the off-target effects of the TKIs and talk about toxicity. Axitinib and tivozanib are the most narrowly focused. They have the least off-target effects. The thought was that would result in greater potency as well as less toxicity, and if you had to choose and were asked, “What is the most potent VEGF receptor inhibitor?”, it’s going to be tivozanib. It’s a third-generation drug, [and] it’s at nanomolar concentrations.
All these drugs have their own unique pharmacokinetic properties, and they have their own unique off-target effects, and that is why there doesn’t appear to be complete crossresistance among the agents and why we’ve been able to sequence them in patients. They all seem to inhibit VEGF, but they do other things, and on the pharmacokinetic side, there are a lot of basic science data on theories [about] why a shorter half-life is better or a longer half-life is better, etc. For tivozanib, its half-life is 80.9 hours.1 This results in its dosing as a 3-week-on, 1-week-off regimen, and the thought is that you get constant exposure of the VEGF receptor and that having the receptor constantly exposed and occupied is beneficial in contrast to a drug like axitinib, where the halflife is 2 to 5 hours, which lends itself well to adverse event [AE] management. But you wonder what happens during the times that the VEGF receptor is not inhibited. Again, these are all theories with no head-to-head studies, but [these are] why [researchers] think one may be superior to the other.
What practical considerations are there for the use of tivozanib as third-line RCC therapy?
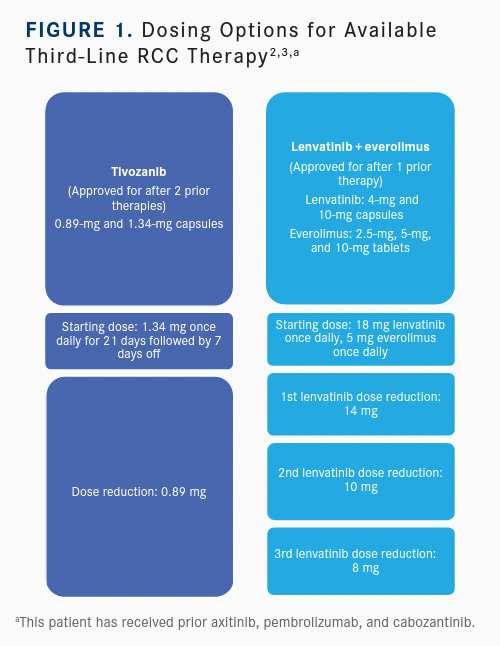
For practical considerations with the management of tivozanib, it seems to be a well-tolerated inhibitor of VEGF with not a lot of off-target effects. We see diarrhea, nausea, and vomiting. [Dosing] starts at 1.34 mg daily, but there is a lower dose at 0.89 mg. [It is given] 3 weeks on, 1 week off. Patients can take the medication with or without food. AE management is [needed] mainly for diarrhea, nausea, and vomiting. You also need to watch for hypertension and manage that, and those modifications would be down to 0.89 mg when you need [them] [Figure2,3].
What have researchers recently learned about the dosage of lenvatinib plus everolimus (Afinitor) as second- or later-line therapy?
[There was] a postmarketing, open-label, randomized trial [NCT03173560] looking at lenvatinib/everolimus. A lot of physicians will…start with 14 mg daily, and there’s been a concern [about] whether you should start at 18 mg daily with lenvatinib/everolimus. The recommendation is that you should start at full dose, which would be 18 mg, and the study was done looking at 14 mg vs 18 mg. The thought was, could you get a better outcome going with a lower dose? You would have fewer dose reductions, and you would have [fewer] discontinuations. The answer was no; it was actually less effective [Table 14].
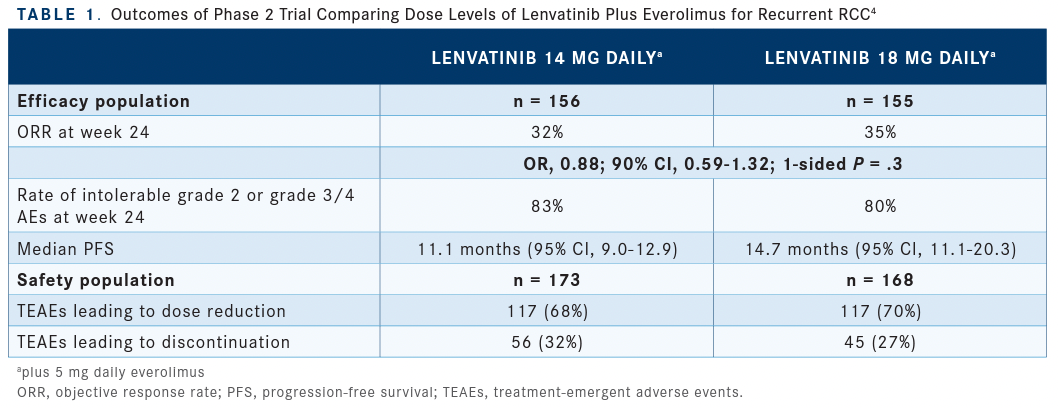
We generally want to start at full dose when you can with TKIs. And with lenvatinib/everolimus, we want to start with 18 mg when we can, let the AEs declare themselves, and try to manage them with best supportive care. We find that [approximately] 25% to 30% of patients stay at full dose and that [ approximately] 70% need to go on a lower dose, and that’s the way I handle it in my practice. This data set would tell you that’s the right way.
I know some [physicians] start at 14 mg, and I think you have to get used to the drug and make your own choices. But if you do start at 14 mg, I would encourage you to go up to 18 mg when you can, because you don’t know [whether] you’re at the right dose for the patient with as much as they can get unless you’re at the full dose.
What toxicities are most significant in later-line TKI-based regimens for RCC?
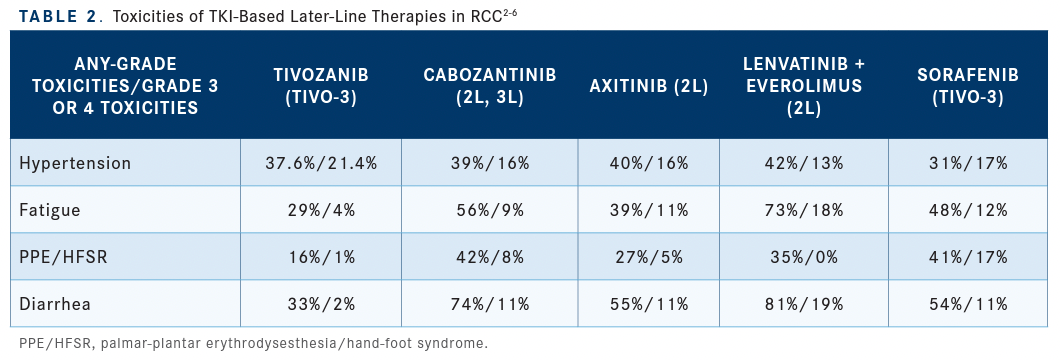
Toxicities that are concerning among these agents are hypertension, fatigue, hand-foot syndrome, [and] diarrhea. [Data from clinical trials] give you some idea about some of the AEs and tolerance. Tivozanib is one of our most tolerable agents. It appears to be more tolerable than axitinib [Table 22-6]. When you look at the published data, if you’re going to have issues with AEs and that’s a concern for you in choosing an agent for your patient, tivozanib is going to give you the least [amount of] issues. Its AE that is an issue is hypertension, and we see that manifest with the potent inhibitors of the VEGF receptor. But as far as fatigue, hand-foot syndrome, and diarrhea, it’s one of the most tolerable of the agents. It’s even more tolerable than what was seen with axitinib. Some of our more toxic agents would be cabozantinib [and] lenvatinib/everolimus, and we recognize they need dose reductions and dose interruptions. Then there is sorafenib, which was our first agent approved for RCC, and [we are familiar with] the AEs it has.
REFERENCES
1. Fogli S, Porta C, Del Re M, et al. Optimizing treatment of renal cell carcinoma with VEGFR-TKIs: a comparison of clinical pharmacology and drug-drug interactions of anti-angiogenic drugs. Cancer Treat Rev. 2020;84:101966. doi:10.1016/j. ctrv.2020.101966
2. Pal SK, Puente J, Heng DYC, et al. Assessing the safety and efficacy of two starting doses of lenvatinib plus everolimus in patients with renal cell carcinoma: a randomized phase 2 trial. Eur Urol. 2022;82(3):283-292. doi:10.1016/j. eururo.2021.12.024
3. Fotivda. Prescribing information. AVEO Pharmaceuticals; 2021. Accessed March 1, 2023. https://bit.ly/3ELQ8Ei
4. Lenvima. Prescribing information. Eisai; 2022. Accessed March 1, 2023. https://bit.ly/3ZsUMz4
5. Cabometyx. Prescribing information. Exelixis; 2021. Accessed March 1, 2023. https://bit.ly/3Z8xpec
6. Inlyta. Prescribing information. Pfizer; 2022. Accessed March 1, 2023. https:// bit.ly/3y6GUyw

Enhancing Precision in Immunotherapy: CD8 PET-Avidity in RCC
March 1st 2024In this episode of Emerging Experts, Peter Zang, MD, highlights research on baseline CD8 lymph node avidity with 89-Zr-crefmirlimab for the treatment of patients with metastatic renal cell carcinoma and response to immunotherapy.
Listen
Beyond the First-Line: Economides on Advancing Therapies in RCC
February 1st 2024In our 4th episode of Emerging Experts, Minas P. Economides, MD, unveils the challenges and opportunities for renal cell carcinoma treatment, focusing on the lack of therapies available in the second-line setting.
Listen