Adjuvant Setting in RCC Is Shown to Favor Pembrolizumab
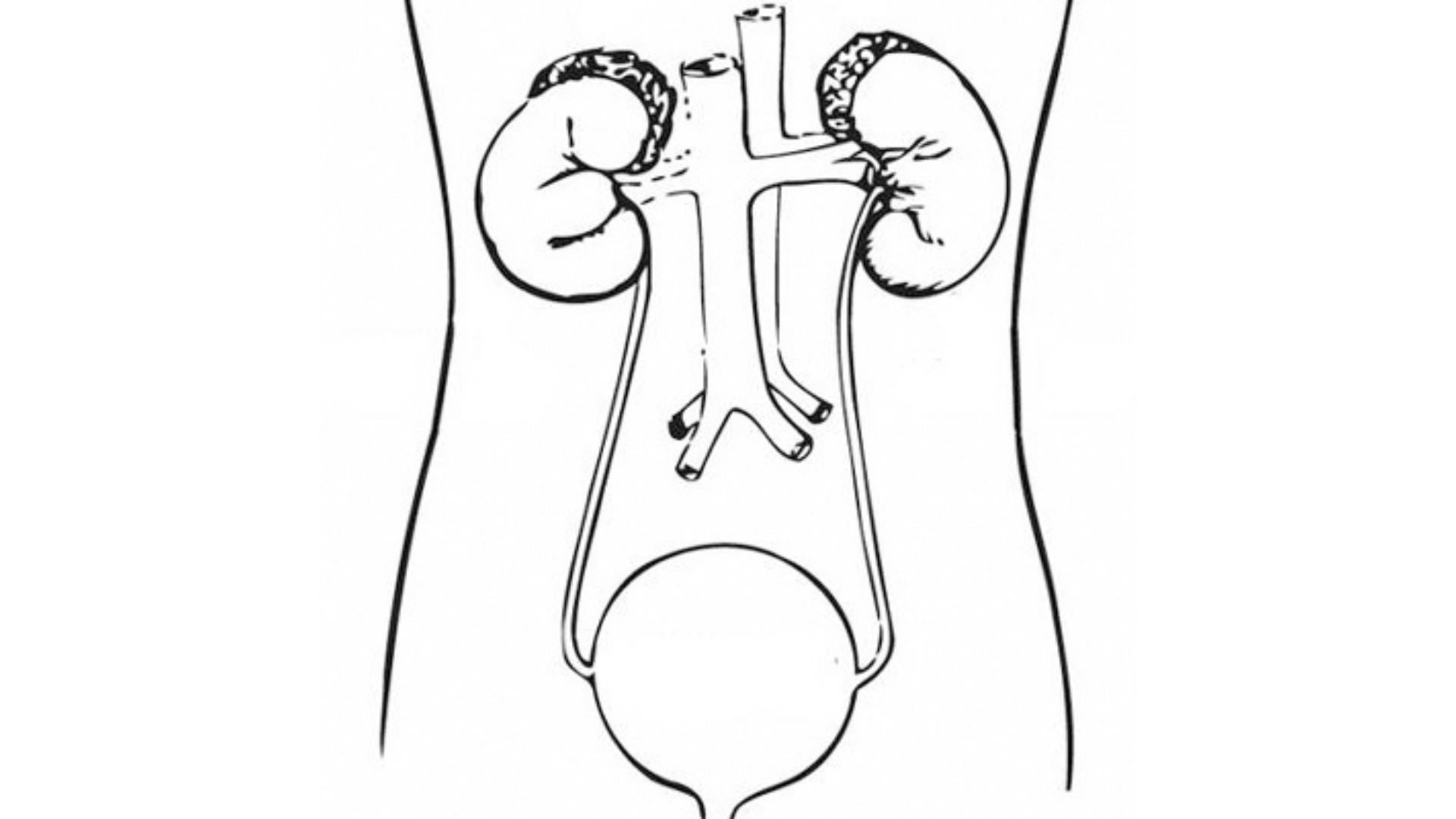
The landmark study, KEYNOTE-564, compared pembrolizumab vs placebo in patients with clear cell renal cell carcinoma who were at high risk for recurrence after nephrectomy.
David A. Braun, MD, PhD

In patients with localized renal cell carcinoma (RCC) in the adjuvant setting, the aim of therapy is to reduce the risk of recurrence and improve outcomes because as much as 50% of patients progress to metastatic disease.1 In the era of immune checkpoint inhibitors, their benefit in the adjuvant setting is unclear. Early data did not deliver an overall survival (OS) benefit, although pembrolizumab (Keytruda) received an approval in this setting.2
“The treatment landscape of adjuvant and metastatic renal cell carcinoma is controversial,” David A. Braun, MD, PhD, an assistant professor of medicine (medical oncology) and the Louis Goodman and Alfred Gilman Yale Scholar at Yale University School of Medicine in New Haven, Connecticut, said during the 41st Annual Chemotherapy Foundation Symposium Innovative Cancer Therapy for Tomorrow conference.3 “We’re going to try to reconcile these [controversies] during my presentation,” Braun continued.
KEYNOTE-564
The landmark study, KEYNOTE-564 (NCT03142334), compared pembrolizumab vs placebo in patients with clear cell RCC who were at high risk for recurrence after nephrectomy.4
The double-blind, phase 3 trial randomly assigned patients to receive pembrolizumab (n = 496) or placebo (n = 498). Investigators reported that the pembrolizumab group had longer disease-free survival (DFS) vs placebo at 24 months (77.3% vs 68.1%; HR, 0.68; 95% CI, 0.53-0.87; P = .002). The estimated percentage of patients who remained alive at 24 months was 96.6% in the pembrolizumab group and 93.5% in the placebo group (HR, 0.54; 95% CI, 0.30-0.96). At 12 months, the corresponding percentages were 85.7% (95% CI, 82.2%-88.5%) and 76.2% (95% CI, 72.2%-79.7%).
“Patients were stratified as either intermediate high risk, high risk, or M1 NED [no evidence of disease]. Intermediate high-risk patients were by far the most common type,” Braun said.
Looking at the 30-month update, pembrolizumab demonstrated an absolute DFS benefit: 78.3% vs 67.3% (HR, 0.63; 95% CI, 0.50%-0.80%; P < .0001). Braun noted that as he interpreted these findings, the benefit scales with the risk, so the benefit is relatively modest when looking at the intermediate high-risk group. Reviewing the high-risk group, the benefit appears to be larger, and it appears to be very large in the last group.
IMmotion010
In the IMmotion010 trial (NCT03024996),5 after undergoing nephrectomy, patients were randomly assigned to receive atezolizumab (Tecentriq; n = 390) at 1200 mg or placebo (n = 388) once every 3 weeks for 16 cycles of 1 year. Patients were stratified according to disease stage, geographical region, and PD-L1 status based on the presence of tumor-infiltrating immune cells (< 1% vs ≥ 1%).
At a median follow-up duration of 44.7 months (interquartile range [IQR], 39.1-51.0), the DFS for patients in the atezolizumab group was 57.2 months (95% CI, 44.6-not evaluable [NE]) compared with 49.5 months for the placebo group (95% CI, 47.4-NE; HR, 0.93; 95% CI, 0.75-1.15; P = .50).5
“I think there is emerging evidence that PD-L1 inhibition is less effective in kidney cancer than PD-1 inhibition,” Braun said. “Many people have had this experience. If we look at regimens that have OS benefit, none of those are with PD-L1 inhibitors.”
CheckMate-914
The double-blind, randomized, phase 3 CheckMate 914 trial (NCT03138512) enrolled patients with localized clear cell RCC who were at high risk of relapse after radical or partial nephrectomy between 4 and 12 weeks before random assignment.6
Overall, adjuvant nivolumab plus ipilimumab did not prolong DFS in clear cell RCC, according to the researchers. However, post hoc analysis suggested that some high-risk subgroups such as patients with sarcomatoid tumor or patients with stage T4 do benefit.6
“One of the key challenges with this regimen is toxicity,” Braun said. “In the adjuvant setting, the use of dual immune checkpoint blockade was very toxic, with [approximately] one-third of patients having had to discontinue therapy.”
PROSPER
The PROSPER trial (NCT03055013)7 randomly assigned 805 patients to receive nivolumab and surgery or surgery and observation. In the treatment arm, patients received 1 dose of nivolumab, then had partial or radical nephrectomy, and then followed up with 9 doses of nivolumab.
“Patients with any histology of RCC were allowed to enroll and there [were] a lot of patients with early-stage disease,” Braun said. “Clinically, almost half the patients had early-risk disease, and on pathologic staging, [approximately] one-third of patients had stage I or II.”
It was found that perioperative nivolumab did not prolong DFS (HR, 0.97; 95% CI, 0.74-1.28; P = .43) and the study was stopped because of futility at the interim analysis. One criticism of the trial was that it enrolled low-risk patients and so they could have been cured by surgery alone.
Clinical Question
At this point, the clinical question becomes should patients treated with a prior immune checkpoint inhibitor (ICI), receive a combination of an ICI and tyrosine kinase inhibitor (TKI) or can a TKI alone be used?
This was explored in a number of studies.8,9 Chung-Han Lee and colleagues9 evaluated intravenous pembrolizumab (200 mg) and lenvatinib (Lenvima; 20 mg) in a phase 1b/2 efficacy and safety study (NCT02501096). The primary end point was objective response rate.
Regarding safety, 57% of patients had a grade 3 treatment-related adverse event (TRAEs) and 7% had grade 4 TRAEs.
In the CONTACT-03 trial (NCT04338269)10 patients whose disease progressed after ICI therapy were randomly assigned to receive atezolizumab plus cabozantinib (Cabometyx) or cabozantinib alone.
In the combination arm, findings showed a median progression-free survival (PFS) of 10.6 months (95% CI, 9.8-12.3) and 10.8 months (95% CI, 10.0-12.5) with the single agent (HR, 1.03; 95% CI, 0.831.28; P = .78).
Median OS was 25.7 months in the combination arm and was not evaluable in the single-agent arm (HR, 0.94; 95% CI, 0.70-1.27; P = .69).
Braun said rechallenging with ICI to improve response showed no difference in response, primary progressive disease rate, disease control, or duration of response. Similarly, rechallenging with ICI did not improve PFS or OS. The combination was also shown to be more toxic than a TKI alone.
Braun also noted that anti-PD-(L)1 should not routinely be used immediately after progression. Furthermore, evidence showing a benefit of delaying re-challenge was not available and treatment for recurrence following adjuvant pembrolizumab was inconclusive.
REFERENCES:
1. Cosso F, Roviello G, Nesi G, et al. adjuvant therapy for renal cell carcinoma: hype or hope?. Int J Mol Sci. 2023;24(4):4243. doi:10.3390/ijms24044243
2. FDA approves pembrolizumab for adjuvant treatment of renal cell carcinoma. News release. FDA. November 17, 2021. Accessed November 20, 2023. https://tinyurl.com/4w2kp2hd
3. Braun DA. Controversies in adjuvant and metastatic treatment settings for renal cell carcinoma. Presented at: Chemotherapy Foundation Symposium; November 8-10, 2023; New York, New York.
4. Choueiri TK, Tomczak P, Park SH, et al. Adjuvant pembrolizumab after nephrectomy in renal-cell carcinoma. N Engl J Med. 2021;385(8):683-694. doi:10.1056/NEJMoa2106391
5. Pal SK, Uzzo R, Karam JA, et al. Adjuvant atezolizumab versus placebo for patients with renal cell carcinoma at increased risk of recurrence following resection (IMmotion010): a multicentre, randomised, double-blind, phase 3 trial. Lancet. 2022;400(10358):1103-1116. doi:10.1016/S01406736(22)01658-0
6. Motzer RJ, Russo P, Grünwald V, et al. Adjuvant nivolumab plus ipilimumab versus placebo for localised renal cell carcinoma after nephrectomy (CheckMate 914): a double-blind, randomised, phase 3 trial. Lancet. 2023;401(10379):821-832. doi:10.1016/S0140-6736(22)02574-0
7. Allaf ME, Kim SE, Master VA, et al. PROSPER: Phase III randomized study comparing perioperative nivolumab versus observation in patients with renal cell carcinoma (RCC) undergoing nephrectomy (ECOG-ACRIN EA8143). J Clin Oncol. 2021;39(suppl 15):TPS4596-TPS4596. doi: 10.1200/ JCO.2021.39.15_suppl.TPS4596
8. Ravi P, Mantia C, Su C, et al. Evaluation of the safety and efficacy of immunotherapy rechallenge in patients with renal cell carcinoma. JAMA Oncol. 2020;6(10):1606-1610. doi:10.1001/jamaoncol.2020.2169
9. Lee CH, Shah AY, Rasco D, et al. Lenvatinib plus pembrolizumab in patients with either treatment-naive or previously treated metastatic renal cell carcinoma (Study 111/KEYNOTE-146): a phase 1b/2 study. Lancet Oncol. 2021;22(7):946958. doi:10.1016/S1470-2045(21)00241-2
10. Pal SK, Albiges L, Tomczak P, et al. Atezolizumab plus cabozantinib versus cabozantinib monotherapy for patients with renal cell carcinoma after progression with previous immune checkpoint inhibitor treatment (CONTACT-03): a multicentre, randomised, open-label, phase 3 trial. Lancet. 2023;402(10397):185-195. doi:10.1016/S01406736(23)00922-4

Enhancing Precision in Immunotherapy: CD8 PET-Avidity in RCC
March 1st 2024In this episode of Emerging Experts, Peter Zang, MD, highlights research on baseline CD8 lymph node avidity with 89-Zr-crefmirlimab for the treatment of patients with metastatic renal cell carcinoma and response to immunotherapy.
Listen
Beyond the First-Line: Economides on Advancing Therapies in RCC
February 1st 2024In our 4th episode of Emerging Experts, Minas P. Economides, MD, unveils the challenges and opportunities for renal cell carcinoma treatment, focusing on the lack of therapies available in the second-line setting.
Listen