The End of Conventional Chemotherapy for Urothelial Cancer
According to John M. Burke, MD, it is hard to imagine that results presented at ESMO in the urothelial cancer space will not lead to the complete replacement of conventional chemotherapy as the standard first-line treatment.
John M. Burke, MD
Hematologist and Medical Oncologist
Rocky Mountain Cancer Centers
Associate Chair
US Oncology Hematology
Research Program Aurora, CO

In the last 20 years we have seen targeted therapies and immunotherapies emerge as effective treatments for cancer. In most cases, the rollout of such therapies has been in a relatively orderly fashion, starting with demonstrated benefit in heavily pretreated patients and then slowly moving forward as the therapies are compared with standard chemotherapy. And in some cases, novel therapies have completely replaced chemotherapy, making the latter obsolete.
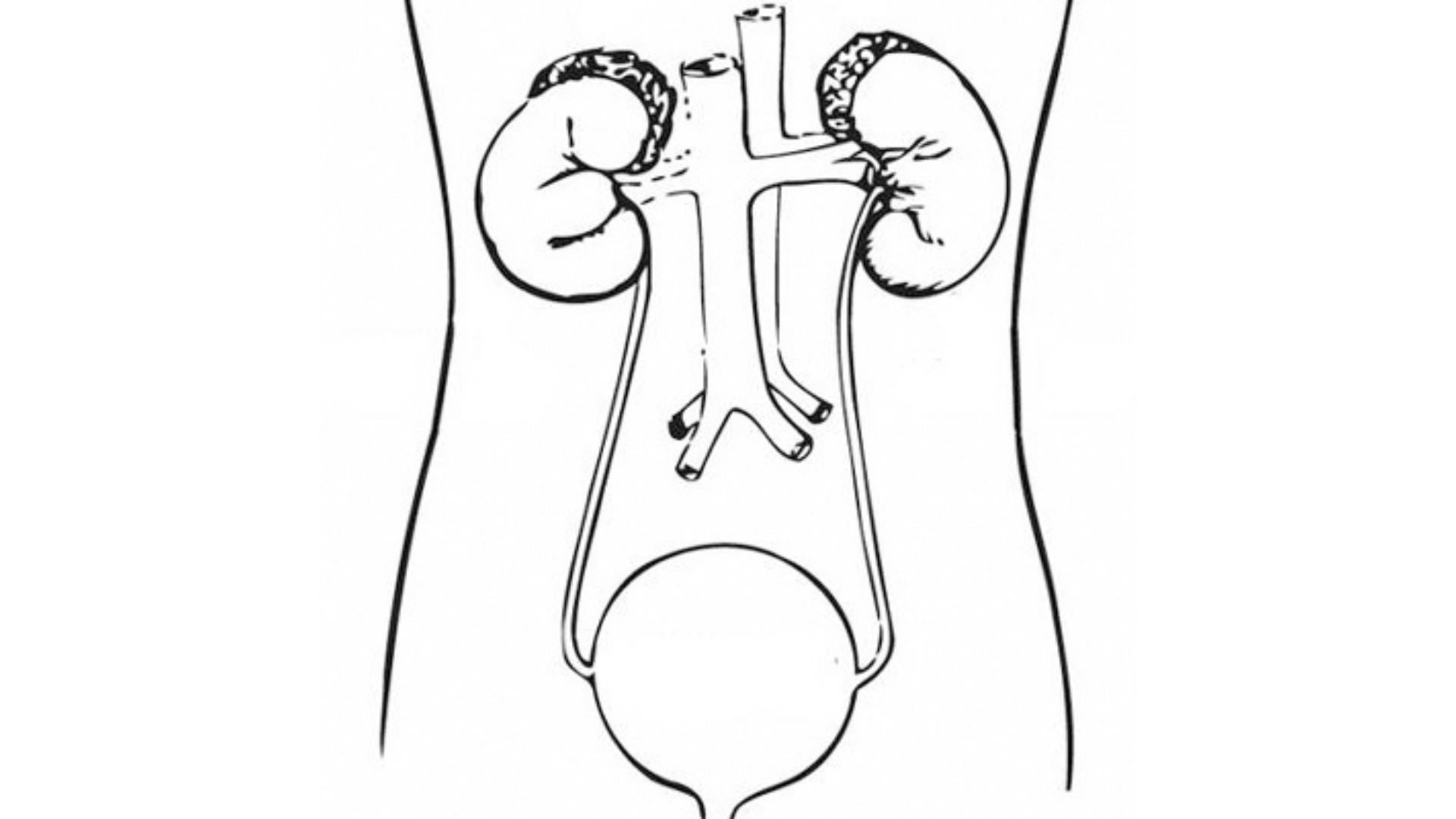
At this year’s European Society for Medical Oncology (ESMO) meeting in Madrid, Spain, we learned that urothelial cancer may be next in line for such a paradigm shift. Many patients with metastatic urothelial cancer have comorbidities, often including renal impairment, which prevent the safe administration of cisplatin or carboplatin. In such patients, use of the PD-1 inhibitor pembrolizumab (Keytruda) had enough of a response rate for the agent to achieve FDA approval and routine use.
Then came data looking at the combination of pembrolizumab plus the nectin-4–targeting antibody–drug conjugate enfortumab vedotin (Padcev) that got everyone’s attention. Findings from phase 1 and 2 studies demonstrated that the combination produced objective response rates in the range of 65% to 73% with median duration of response exceeding 1 year. Based on these data, in early 2023 the FDA granted the combination an accelerated approval for patients not eligible for cisplatin-containing chemotherapy.
Of course, we all know that results of phase 2 trials are often not reproduced in randomized phase 3 trials. Enter EV-302/KEYNOTE KN-A39 (NCT04223856), whose data were presented at the ESMO meeting in October 2023. In the trial, 886 patients with previously untreated locally advanced or metastatic urothelial carcinoma were randomly assigned to receive platinum-based chemotherapy (gemcitabine plus either cisplatin or carboplatin) or enfortumab vedotin plus pembrolizumab (EV-P). Compared with the control arm, EV-P improved progression-free survival (median, 12.5 vs 6.3 months; HR, 0.45; P < .00001), overall survival (median, 31.5 vs 16.1 months; HR, 0.47; P < .00001), and objective response rate (68% vs 44%; P < .00001). It is hard to imagine that these astonishing results will not lead to the complete replacement of conventional chemotherapy as the standard first-line treatment for metastatic urothelial carcinoma.
Score another win for targeted therapies.