Nivolumab Plus Chemotherapy Demonstrates Superior OS in Esophageal/Gastric Cancer
At 12 months, patients in the experimental arm showed OS rates of 14.4% compared with 11.1% for patients receiving chemotherapy alone in the phase 3, open-label CheckMate649 study.
Geoffrey Y. Ku, MD
Medical Oncologist
Memorial Sloan Kettering Cancer Center
New York, NY
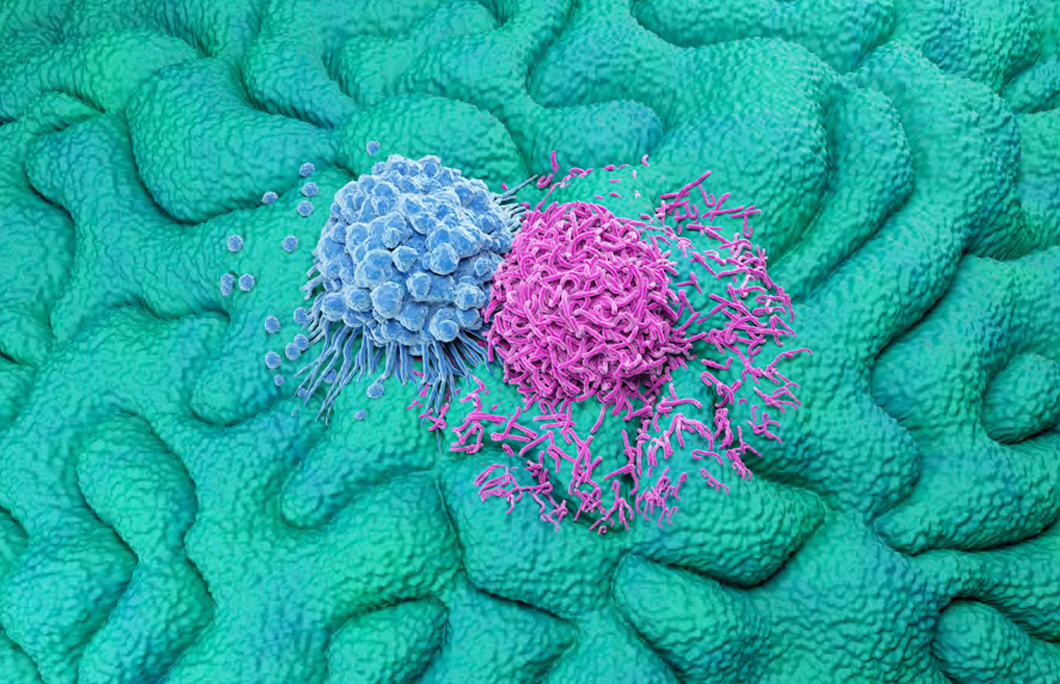
Patients with HER2-negative esophageal/gastric cancer experienced a 29% reduction in risk of death and a 3.3-month improvement in median overall survival (OS) when receiving nivolumab (Opdivo) added to chemotherapy regimens if their tumors expressed a PD-L1 combined positive score (CPS) greater than 5.1 At 12 months, patients in the experimental arm showed OS rates of 14.4% (95% CI, 13.1%16.2%) compared with 11.1% for patients receiving chemotherapy alone (95% CI, 10.0%-12.1%), explained Geoffrey Y. Ku, MD, at the 41st Annual Chemotherapy Foundation Symposium Innovative Cancer Therapy for Tomorrow conference held from November 8 to 10, 2023, in New York.1
“I think we know that this is a positive study. There was an approximate 3-month improvement in median overall survival. The hazard ratio [HR] was 0.71 with a highly significant P value [P = .0001],” Ku said. “Based on the hierarchical testing, if you looked at the CPS of 1 or more patients, and all randomly assigned patients, overall survival was improved across all groups. But as the CPS cutoff goes down, and there are more patients that are treated, you’ll note that the hazard ratio goes up, and there’s less benefit.” Ku is a medical oncologist specializing in gastrointestinal, pancreatic, and esophageal cancer in New York, New York, and is affiliated with Memorial Sloan Kettering Cancer Center.
The phase 3, open-label CheckMate649 study (NCT02872116) determined the primary end points of progression-free survival (PFS) and OS evaluating patients with PD-L1 CPS scores of 5 or more tumors. In this trial, investigators evaluated nivolumab combined with either FOLFOX (oxaliplatin, leucovorin, fluorouracil) or XELOX (oxaliplatin and capecitabine [Xeloda]), nivolumab plus ipilimumab (Yervoy) in the second arm, and chemotherapy alone in the remaining arm. The nivolumab plus ipilimumab arm was closed prematurely due to toxicity and a lack of efficacy. Trial investigators evaluated 3185 patients who were randomly assigned 1:1 across arms with 1581 patients concurrently randomly assigned to the nivolumab plus chemotherapy or chemotherapy-alone arms and 813 patients to the nivolumab plus ipilimumab or chemotherapy-alone arms. Approximately 69% of patients had gastric cancer, 18% had gastroesophageal junction cancer, and 12% had esophageal adenocarcinoma, respectively.2
Ku remarked that, although there was a positive OS reported, the benefit was restricted to patients with a CPS score of 5 or more and patients with lower CPS scores did not benefit as greatly. In the subgroup analysis, Ku highlighted that the HR crossing 1 indicates a neutral or insignificant effect. Specifically, for tumors with a CPS of less than 5, the estimated point for OS and PFS stood at 0.94 and 0.93, suggesting minimal to no significant benefit.
“It’s important to note that the FDA approved the combination of nivolumab plus FOLFOX for all patients with esophageal gastric adenocarcinoma regardless of their PD-L1 status,” Ku explained. “On the other hand, the NCCN [National Comprehensive Cancer Network] guidelines endorsed the combination of nivolumab and FOLFOX for patients where the CPS is 5 or more, and it’s classified as a category 1 recommendation, and therefore very unambiguous. However, in patients with a CPS of 1 to 4, the recommendation is classified as a category 2B, implying that there is significant disagreement on the verdict.”
In addition, NCCN is silent and agnostic on the PD-L1, CPS zero tumors specification, making no mention of how to proceed with treatment for this specific demographic, Ku continued. “It’s interesting that the FDA tends to approve these drugs in a blanket intention-to-treat population, whereas NCCN guidelines tend to be more restrictive. That’s true for KEYNOTE-590 [NCT03189719], but also for the ToGA study [NCT01041404] that led to the approval of trastuzumab [Enhertu] more than a decade ago,” Ku explained.3
Among other studies mentioned, Ku addressed the phase 3 KEYNOTE-062 (NCT02494583),4 KEYNOTE 590 (NCT03189719),5 and KEYNOTE-811 (NCT03615326) trials,6 which evaluated the efficacy of pembrolizumab (Keytruda) with chemotherapy for advanced HER2-positive gastric cancer and esophageal cancer. As with CheckMate649, the FDA approved the pembrolizumab and chemotherapy combination in all patients; however, NCCN guidelines endorse pembrolizumab with chemotherapy only for patients where the tumor PD-L1 CPS is 10 or more as a category 1 recommendation. If the CPS is less than 10, then it’s a category 2B recommendation.
“I hope I’ve managed to convey that the PD-L1 CPS cutoff does identify subgroups that are more likely to benefit, as well as subgroups that are unlikely to benefit. For HER2-positive gastroesophageal junction and gastric adenocarcinoma, pembrolizumab, trastuzumab, and chemotherapy has been a standard of care, although the FDA approval is being amended to exclude PD-L1 CPS zero tumors,” Ku concluded.
REFERENCES
1. Ku G. Current standard of care for first-line therapy in advanced esophageal/gastric cancer. Presented at: CFS Chemotherapy Foundation Symposium Innovative Cancer Therapy for Tomorrow conference; November 8-10, 2023; New York, NY.
2. Shitara K, Ajani JA, Moehler M, et al. Nivolumab plus chemotherapy or ipilimumab in gastro-oesophageal cancer. Nature. 2022;603(7903):942-948. doi:10.1038/s41586-02204508-4
3. FDA approves nivolumab in combination with chemotherapy for metastatic gastric cancer and esophageal adenocarcinoma. FDA. Updated April 16,, 2021. Accessed November 20, 2023. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-nivolumab-combination-chemotherapy-metastatic-gastric-cancer-and-esophageal
4. Shitara K, Van Cutsem E, Bang YJ, et al. Efficacy and safety of pembrolizumab or pembrolizumab plus chemotherapy vs chemotherapy alone for patients with first-line, advanced gastric cancer: the KEYNOTE-062 phase 3 randomized clinical trial. JAMA Oncol. 2020;6(10):1571-1580. doi:10.1001/ jamaoncol.2020.3370
5. Kato K, Shah MA, Enzinger P, et al. KEYNOTE-590: Phase III study of first-line chemotherapy with or without pembrolizumab for advanced esophageal cancer. Future Oncol. 2019;15(10):1057-1066. doi:10.2217/fon-2018-0609
6. Janjigian YY, Kawazoe A, Yañez P, et al. The KEYNOTE-811 trial of dual PD-1 and HER2 blockade in HER2-positive gastric cancer. Nature. 2021;600(7890):727-730. doi:10.1038/s41586-021-04161-3