TMB-VH, Potential Biomarker, Is Tied to Anti–PD-L1 Response Across Tumor Types
Very high tumor burden is a potential biomarker that may predict response to anti–PD-L1 therapy in patients of Asian descent across cancer types.
A potential new biomarker, very high tumor burden (TMB-VH), has emerged that could predict response to anti–PD-L1 therapy in patients of Asian descent across cancer types, according to a study published in the Journal for ImmunoTherapy of Cancer.
Between 2019 and 2021, investigators at Samsung Medical Center in Seoul, South Korea, used anti–PD-1/PD-L1 therapy to treat 426 patients with cancer. A total of 1744 patient samples were measured using the TruSight Oncology 500 (TSO500) assay.
Researchers reported that the incidence of TMB-high (TMB-H), defined as 10 or more mutations (mt)/megabase (Mb), was 14.7% (n = 257). Further stratification determined TMB low (TMB-L), defined as 10 or less mt/Mb (n = 1487), was 85.3% ; TMB intermediate high (TMB-IH), defined as between 11 and 16 mt/Mb (n = 186), was 10.7%; and TMB very high (TMB-VH), defined as 16 or higher mt/Mb, was 4.1% (n = 71).
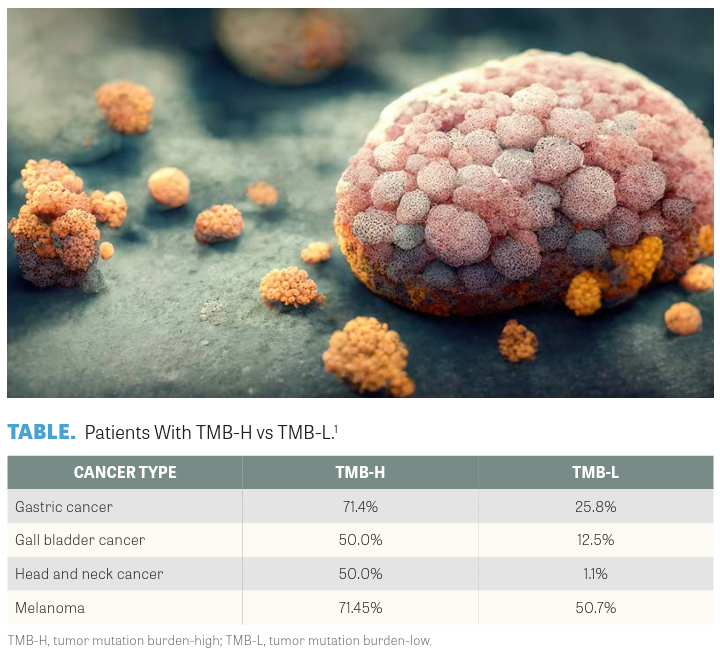
The most common cancers observed in the TMB-H population were colorectal (n = 108, 42.0%), gastric (n = 49, 19.1%), bladder (n = 21, 8.2%), cholangiocarcinoma (n = 21, 8.2%), non–small cell lung cancer (n = 17, 6.6%), melanoma (n = 8, 3.1%), gallbladder (n = 7, 2.7%), and others (n = 26, 10.1%). The response rate to anti–PD-1/PD-L1 therapy for gastric, gallbladder, head and neck cancer, and melanoma (TABLE1) was higher among patients who were TMB-H than patients who were TMB-L.
In the survival analysis, all patients with TMB-VH demonstrated longer overall survival (OS) and progression-free survival (PFS) following anti–PD-L1 therapy compared with patients with TMB-L. No statistically significant difference in OS or PFS was observed after anti–PD-1/ PD-L1 treatment between TMB-IH and TMB-L cohorts or between TMB-H and TMB-L cohorts.
Investigators also reported that the median TMB score of patients who responded to anti–PD-1/PD-L1 therapy was higher in gallbladder (P = .036) than in head and neck cancer (P = .038).
Although TMB-VH, TMB-H, and microsatellite instability high (MSI-H) were significant for predicting response to anti–PD-1/PD-L1 therapy, according to researchers, a multivariate analysis demonstrated that only TMB-VH and MSI-H were significant independent predictors of response to anti–PD-1/PD-L1 therapy.
The investigators wrote that the TMB-VH subgroup, which used a 16 mg/Mb cutoff, demonstrated a benefit from anti–PD-1/ PD-L1 therapy. They attributed the fact that the 10 mt/Mb cutoff for the TMB-H group was not a significant predictive factor for all cancer types for the under-reflected germline single nucleotide polymorphism of Asian ethnicity in the TSO500 assay.
The authors noted that the study limitations included its retrospective analysis and the continuing debate about the predictive value of TMB for PD-1/PD-L1 therapy.
REFERENCE
1. Jung J, Heo YJ, Park S. High tumor mutational burden predicts favorable response to anti-PD-(L)1 therapy in patients with solid tumor: a real-world pan-tumor analysis. J Immunother Cancer. 2023;11(4):e006454. doi:10.1136/jitc-2022-006454

Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More