Shu Discusses Testing and Targeted Treatment in Patients With Nonmetastatic NSCLC
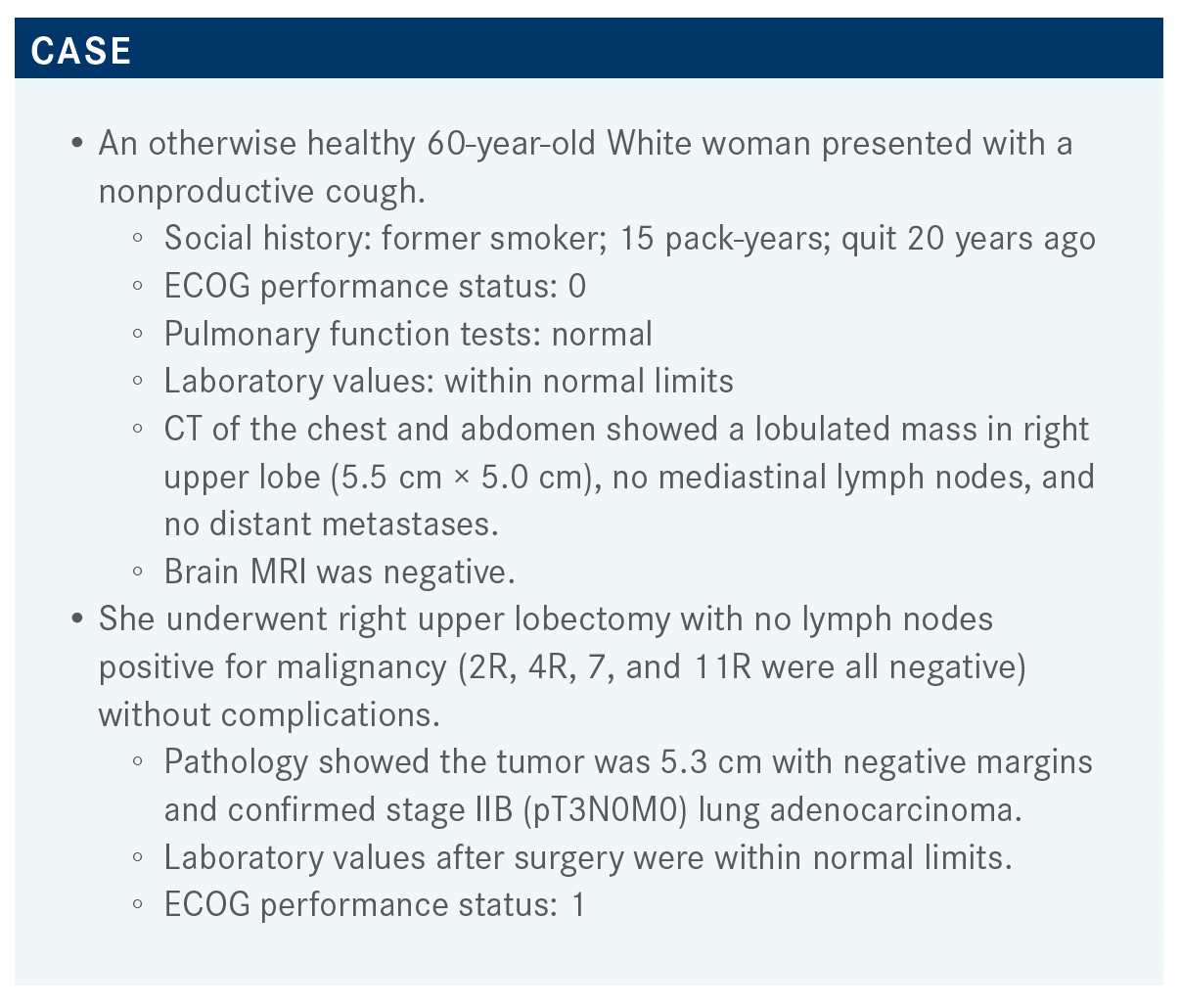
An otherwise healthy 60-year-old White woman presented with a nonproductive cough. The patient's case was the topic of discussion during a recent Case-Based Roundtable event.

During a Targeted Oncology Case-Based Roundtable event, Catherine Ann Shu, MD, assistant professor of Medicine, clinical director, Thoracic Medical Oncology at Herbert Irving Comprehensive Cancer Center of Columbia University in New York, NY, discussed the case of a 60-year-old patient with non–small cell lung cancer.
Targeted OncologyTM: What are the National Comprehensive Cancer Network (NCCN) guidelines for a patient like this?
SHU: According to the NCCN guidelines, this patient is stage IIB [and] margins are negative,1 so we would be talking about chemotherapy and osimertinib [Tagrisso] if indicated. [High-risk features for use of chemotherapy in stages IB and IIA are a tumor greater than 4 cm, vascular invasion, poorly differentiated tumors, visceral pleural involvement, wedge resection, and unknown lymph node status.]
You can make little guidelines in your head that if the tumor is big and has several of these high-risk features, then we’ll want to push the patient toward adjuvant chemotherapy. If there are no high-risk features and it’s a 4-cm toolbar, maybe [we are] less excited to push them, but it’s important to remember these high-risk features are prognostic and not predictive of benefit from therapy.
When do you refer your patients to your radiation oncology colleagues?
DABROWSKI: I mostly refer if this is an R1 resection.
SHU: Positive margin?
DABROWSKI: Yes.
BRAUNSTEIN: If they have no mediastinal disease, N2, or had a resection, we’d probably discuss it in a communal, interdisciplinary tumor board and refer them for radiation if they think it’s case amenable for radiation therapy.
SHU: We also have a multidisciplinary tumor board with radiation oncology always there, and I used to refer a lot more patients to radiation oncology for positive margins, for sure. N2 disease—I used to refer everyone—so even if they had surgery and that [postoperative] N2 disease, [they received] postoperative radiotherapy [PORT].
Recently there was this trial that came out at ESMO [European Society for Medical Oncology] from LUNG ART [NCT00410683],2 and they looked at this idea of PORT. It was a randomized trial looking at patients with completely resected lung cancer, and they had positive N2 disease. These patients were randomized to either control, which is nothing, or they got PORT. We found there was no survival improvement, and the DFS [disease-free survival] hazard ratio was 0.85, but it crossed 1, and the P value was .16 [95% CI, 0.67- 1.07]. Numerically, the DFS was a little better for PORT, but it was not a statistically significant DFS or overall survival [OS] benefit.
Although there was no difference in survival, the secondary end points in this study would be more important. Was it a local failure, or was it metastatic disease?
SHU: Local failure was more common with patients who didn’t get PORT, and the survival benefit was [probably] muted in the PORT arm because they [saw] more cardiac toxicity. I think it will change practice if they publish and show that this continues to hold true, that the toxicity of PORT outweighs the benefit.
What I’m doing now is still sending people for PORT if they have a lot of bulky mediastinal disease, because it prevents local recurrence and it has a part to play. For patients with cardiac disease, or even for patients with small nodal disease, they just have 1 small level VII [node] that was positive, so I’ll hold off on sending them. It’s something that I discuss with the radiation oncologist, that this will be important.
This patient then ended up having 4 cycles of adjuvant chemotherapy with cisplatin and pemetrexed. Her performance status is still 1. The molecular testing revealed the EGFR exon 19 deletion.
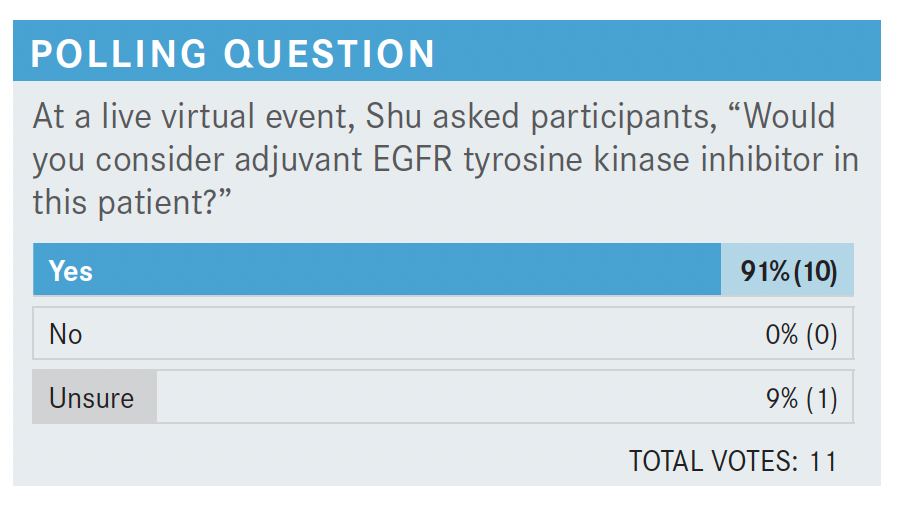
Please discuss the poll results.
BACH: I’m the unsure one, and I’m just going to say [that I’m unsure what to choose] because the patient already had adjuvant therapy. I’m curious to see the data because I’m blanking a little where the TKI [tyrosine kinase inhibitor] comes in. I thought it was post resection in place of chemotherapy.
SHU: It [was] the investigator’s choice on chemotherapy, so a lot of patients did get the chemotherapy, but it’s a good question. I think it’s something we’re all wondering. What do we know about adjuvant EGFR-targeted therapy? This has been debated for a long time. There are a bunch of different trials, such as the RADIANT trial [NCT00373425], [which evaluated] erlotinib [Tarceva] vs placebo, and the [DFS] P value was not significant but certainly looked promising [HR, 0.90; 95% CI, 0.74-1.10; P = .324].3
Then there was the SELECT trial [NCT00462995], which looks very promising but was just your standard 1-arm trial [with erlotinib], so it was not randomized.4 CTONG [NCT01405079] was an adjuvant gefitinib [Iressa] trial, which also didn’t show a benefit for [OS] but showed quite an interesting DFS curve [HR, 0.60; 95% CI, 0.42- 0.87; P = .0054].5 All of these studies show there is some excitement in whether we have the right drug or the right patient population. This is always an important question for us.
What was the design of the ADAURA [NCT02511106] trial?
SHU: ADAURA looked at patients with resected stage IB to IIIA non–small cell lung cancer with or without adjuvant chemotherapy.6 It was interesting because they had the surgery, then it was investigator’s choice to decide whether they wanted to give the adjuvant chemotherapy. Then they were randomized to osimertinib [Tagrisso] vs placebo. Patients would get 3 years of osimertinib, and there was no clear stratification for whether they received chemotherapy.
The baseline characteristics were similar between the 2 [arms].7 It was a heavy female, Asian population, EGFR exon 19 deletion was the most common, and 60% of the patients got adjuvant chemotherapy.
I always thought it was a fairly low number considering these patients were all going on to trial and [were] probably fit enough to get chemotherapy. Remember they’re getting randomized, so they are not guaranteed to get osimertinib.
The [patients with] stage II to IIIA [disease had an] 83% reduction in the risk of disease recurrence, very significant [HR, 0.17; 99.06% CI, 0.11-0.26; P < .001].7 And [in the] overall population, stages IB to IIIA, it was an 80% reduction in the risk of recurrence or death [HR, 0.20; 99.12% CI, 0.14-0.30; P < .001]. This was DFS, and keep in mind the primary end point was DFS in stage II to IIIA, but then they included patients who also had IB to IIIA disease.
What were the results of this trial and your reactions to it?
SHU: It is a very impressive study. On the osimertinib arm, almost everyone did better, regardless of whether they were male, female, smoking, never smoking, [or their stage of disease].7 You can see the [patients with stage] IB did better—again, not the primary end point—and they did better regardless of whether they received adjuvant chemotherapy.
We can’t say patients who got adjuvant chemotherapy and osimertinib did better than patients who did not get adjuvant chemotherapy and osimertinib. We don’t know [that]. We could say everyone who got adjuvant chemotherapy did better, and people who didn’t get adjuvant therapy also did. I think that’s helpful, but maybe doesn’t answer the exact question we’re [sometimes] looking for in practice.
The DFS by stage has a very impressive hazard ratio regardless of whether they had stage IB, II, or III.7 In stage II and III disease, you’re seeing an even greater benefit, and the CNS [central nervous system] benefit was also very impressive. Osimertinib has better blood-brain barrier penetration, so there’s some surprise to us that we see an 82% reduction in the risk of CNS disease recurrence or death.
What we really want to know is: [If you put these patients] on this drug for 3 years, is it tolerable?6 It is. It does cause some issues, like people complain of rash. But I also have a lot of patients who complain about anorexia and they’re losing weight, [are] a little unhappy at the weight loss, and they just have no appetite. So it’s still there. Any adverse event [AE] greater than grade 3 is still higher than placebo, but I would say [it is] tolerated well [overall]. Mostly diarrhea, paronychia, and dry skin [are the common AEs]. It is much better tolerated than erlotinib, and this is also a little easier to tolerate than gefitinib.
Do you use adjuvant osimertinib in your practice?
SHU: I do use adjuvant osimertinib [in my practice].
I use it in stage IB to IIIA, and I still recommend adjuvant chemotherapy in patients with node-positive disease because that’s still the standard of care. Until I have OS data that show we don’t really need the chemotherapy, I’m still giving the chemotherapy.
For the stage IB patients, I am allowing them to just do osimertinib, for example. But I’m curious to hear from the rest of you.
BRAUNSTEIN: These data are very compelling. You showed all the subgroups did very well. Some of the debate seems to be what you do when patients progress on this and whether you’re selecting just for resistance. But you have good data to hang your hat on by giving adjuvant osimertinib.
DALY: The data are very compelling, so at least try it. What is the drawback? Why would you not give it? Seems to be effective overall.
SHU: I guess what Dr Braunstein is saying, does it make the disease more resistant to osimertinib in the future? Those are some of the questions I think we’ll see when we have the OS data, but that makes a lot of sense scientifically and on a practical level. Has anyone had trouble getting it approved by insurance?
DALY: No, I haven’t seen any problems.
VELUSWAMY: I have a question, though. I had an interesting case where the ADAURA data and approval came out about 8 or 9 months after my patient with stage II disease completed adjuvant chemotherapy. She was doing fantastic, but the data came out and we discussed starting her on osimertinib 8 months after. Would you [take this route with the patient]?
SHU: I probably wouldn’t [give osimertinib] 8 months later. I mean, there isn’t a huge downside, but that’s not how the data were collected and written. I tend to be like, if you can’t get adjuvant within 3 months, then now you are 8 months after she’s finished chemotherapy. In that case, I would probably wait. What would you all decide?
VELUSWAMY: Yeah, the same thing, but [the patient] was doing fantastic. Sometime later, 6 to 12 months later, she developed brain metastases, but she’s doing great on osimertinib now.
GERSTEIN: The choices are easy for stage IB disease. You’re just going to use osimertinib. It’s easy for the node-positive patients because you’re going to want to go with chemotherapy up front. Then I would add osimertinib after the chemotherapy because I almost look at it like a patient [with breast cancer]. I’m treating them with chemotherapy, then hormones after.
SHU: I just saw a young woman who came to me for a second opinion at stage IB—well I guess, now it’s IIA. She had a 4 cm tumor, and she [maybe] had 1 or 2 high-risk features.
GERSTEIN: Well, that’s the question, when the patient is in between. It’s easy when it is one extreme or the other.
SHU: [The patient] was IB, and I think she was at 3 cm, but she had 1 or 2 high-risk features. She got her first option, which was chemotherapy followed by osimertinib, and she came to see me. I said I would probably just do osimertinib because that’s a lot of treatment for [someone] with very early-stage disease who wouldn’t even qualify for adjuvant chemotherapy without the osimertinib.
References:
1. NCCN. Clinical Practice Guidelines in Oncology. Non–small cell lung cancer, version 6.2021. Accessed October 17, 2021. https://bit. ly/3GQGtvt
2. Le Pechoux C, Pourel N, Barlesi F, et al. An international randomized trial, comparing post-operative conformal radiotherapy (PORT) to no PORT, in patients with completely resected non-small cell lung cancer (NSCLC) and mediastinal N2 involvement: primary end-point analysis of LungART (IFCT- 0503, UK NCRI, SAKK). Ann Oncol. 2020;31(suppl 4):S1178. doi:10.1016/j. annonc.2020.08.2280
3. Kelly K, Altorki NK, Eberhardt WE, et al. Adjuvant erlotinib versus placebo in patients with stage IB-IIIA non-small-cell lung cancer (RADIANT): a randomized, double-blind, phase III trial. J Clin Oncol. 2015;33(34):4007- 4014. doi:10.1200/JCO.2015.61.8918
4. Pennell NA, Neal JW, Chaft JE, et al. SELECT: a phase II trial of adjuvant erlotinib in patients with resected epidermal growth factor receptor-mutant non-small-cell lung cancer. J Clin Oncol. 2019;37(2):97-104. Published correction appears in J Clin Oncol. 2019;37(7):612.
5. Zhong WZ, Wang Q, Mao WM, et al. Gefitinib versus vinorelbine plus cisplatin as adjuvant treatment for stage II-IIIA (N1-N2) EGFR-mutant NSCLC: final overall survival analysis of CTONG1104 phase III trial. J Clin Oncol. 2021;39(7):713-722. doi:10.1200/JCO.20.01820
6. Herbst RS, Tsuboi M, John T, et al. Osimertinib as adjuvant therapy in patients (pts) with stage IB–IIIA EGFR mutation positive (EGFRm) NSCLC after complete tumor resection: ADAURA. J Clin Oncol. 2020;38(suppl 18):LBA5. doi:10.1200/JCO.2020.38.18_suppl.LBA5
7/ Wu YL, Tsuboi M, He J, et al; ADAURA Investigators. Osimertinib in resected EGFR-mutated non-small-cell lung cancer. N Engl J Med. 2020;383(18):1711-1723. doi:10.1056/NEJMoa2027071