Carthon Discusses Testing and Chemotherapy Vs Targeted Therapy in CRPC
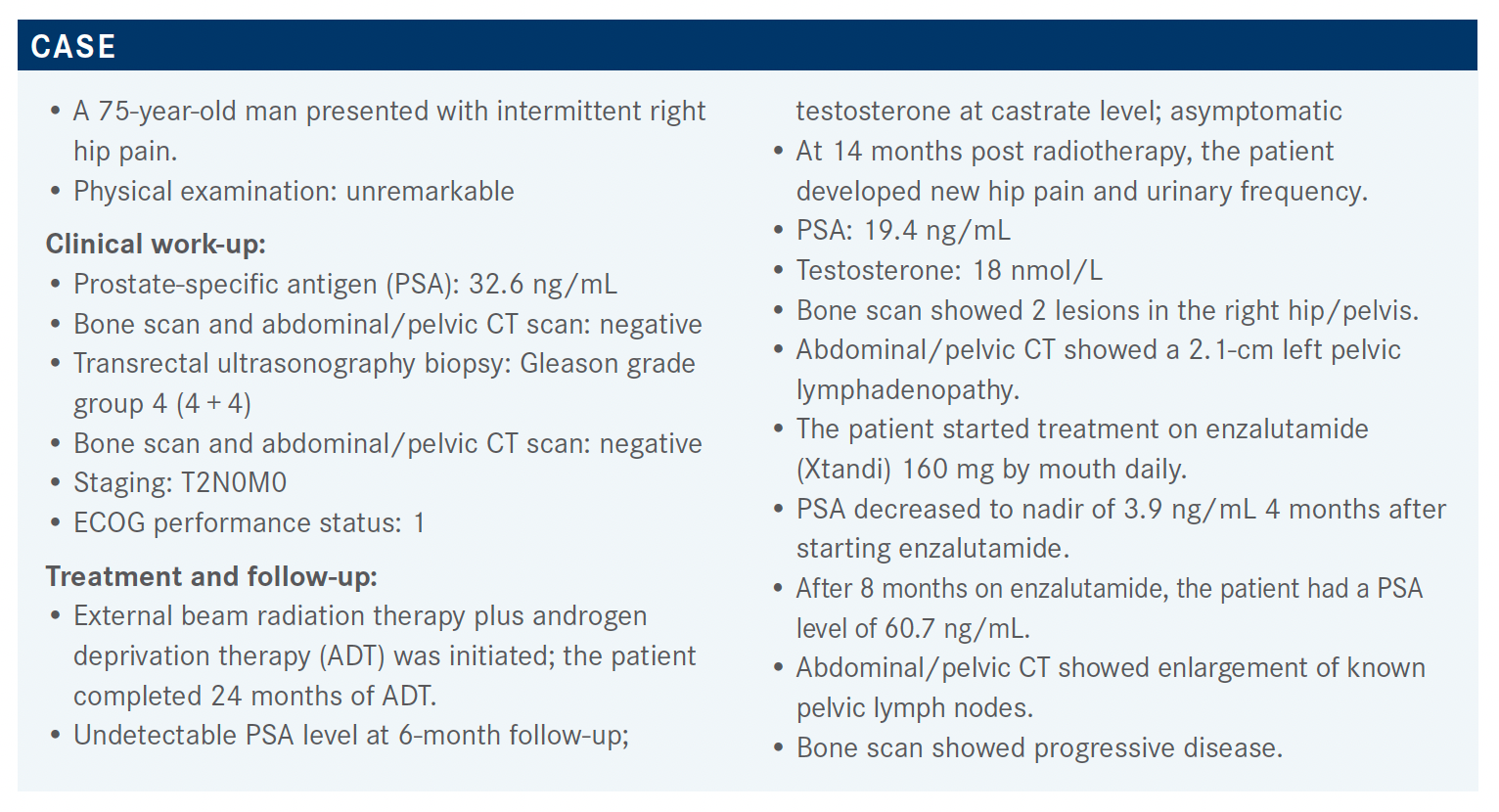
A group of oncologists led by Bradley C. Carthon, MD, PhD, discussed clinical work-up, treatment, and follow-up for a 75-year old patents with castration-resistant prostate cancer.
Bradley C. Carthon, MD, PhD

Bradley C. Carthon, MD, PhD, an associate professor in the Department of Hematology and Medical Oncology at Emory University School of Medicine as well as the section chief of Hematology and Oncology at Emory University Hospital Midtown in Atlanta, GA, discussed the case of a 75-year-old patient with castration-resistant prostate cancer during a Targeted Oncology Case-Based Roundtable event.
Targeted OncologyTM: What are you most likely to recommend now that the patient’s disease is progressing?
CARTHON: Genomic testing was performed, and it showed no actionable mutations. That takes a couple things off the table. [Now] the treatment choices for this patient look at chemotherapy, which is a category 1 recommendation for cabazitaxel [Jevtana], or docetaxel rechallenge.1 We have this patient who has neuropathy and had to stop docetaxel, so we [must] think about that. We have a host of other treatments; some of them dependent on those actionable mutations. Then there are some other things, such as radium 223 [Xofigo], which the patient has not yet had.
Why is the indication so different between olaparib (Lynparza) and rucaparib (Rubraca)? Have you used rucaparib in patients without a BRCA mutation?
A lot of it is the way the trials were set up and the cohorts that were tested. One could argue that, as they have done these studies and screened through the general population, the numbers are smaller and smaller. As you’re looking at each of the specific mutations, the data may not accurately reflect what the efficacy is. [In] the TRITON trial [NCT02952534], when they looked at rucaparib, there were significant numbers of other mutations they were able to see response rates [for].2 Whereas with the studies with olaparib, it was more of a broad-based approach, and some mutations were shepherded in. If you look at the data, you’ll see some of those do not show a great response profile. I think they’re similar. A lot of it is about the cohorts of the study and how they were set up and tested.
What role do chemotherapy and androgen receptor (AR) treatments play in prostate cancer? What are some of the data?
As we talk about chemotherapy vs AR-targeted therapies, we talk a little about patients and tolerating cabazitaxel vs docetaxel. There’s a slightly different profile. [In] some cases, patients tolerate neuropathy much better, but there are also great data looking at those 2 branch points.
If we look at the CARD trial [NCT02485691], this is looking at patients who have had castration-resistant prostate cancer and progress within 12 months on a prior androgen-based therapy before or after docetaxel.3 Because they’ve had those 2 agents, they’re randomized to receive either cabazitaxel vs abiraterone [Zytiga] or enzalutamide— the agent they had not had prior—with end points being primary imaging–based PFS [progression-free survival], secondary OS [overall survival], PSA response, tumor response, and other secondary characteristics.
For the most part, many of these factors were very evenly balanced in the patients that received either cabazitaxel or the AR-targeted therapies. There was some slight difference with age greater than 75 and slight differences with pain— [a little] more in the abiraterone group. With M1 disease, slightly more in the abiraterone-enzalutamide group. But otherwise, pretty well balanced between the 2 categories.
With imaging-based PFS, we see a difference of 8.0 vs 3.7 months between cabazitaxel and the androgen signaling–targeted inhibitors, with a hazard ratio of 0.54 [95% CI, 0.40-0.73; P < .001].3 Looking at the various subgroups, most of the subgroups benefited from cabazitaxel over androgen signaling–targeted inhibitors. Some groups did not show as much of a difference. The confidence intervals were quite wide, but that’s likely from lower numbers. Most of the groups did better with cabazitaxel.
Looking at PFS with other factors, such as symptomatic progression or death from any cause, we see a difference in PFS of 4.4 vs 2.7 months, a hazard ratio of 0.52, and patients benefiting from cabazitaxel [95% CI, 0.40-0.68; P < .0001]. Then with OS, 13.6 months with cabazitaxel, 11.0 months with androgen signaling–targeted inhibitors, with a 0.64 hazard ratio for death [95% CI, 0.46-0.89; P = .008]. With a host of other secondary objectives, whether it be PSA response, tumor response, or pain response—even time to skeletal-related events—cabazitaxel seemed to be superior to the opposite AR inhibitor that the patient received prior.3,4
[Regarding] safety, there seemed to be similar profiles with AEs [adverse events] percentage-wise.3 There was a higher number of AEs leading to treatment discontinuation, but as we’ve used this agent, we know these can be monitored and adjusted for quite readily [cabazitaxel 19.8% vs 8.9% with abiraterone or enzalutamide]. Very reasonable AE profile, I would say. Importantly, quality of life seemed to be preserved for patients on chemotherapy, particularly regarding pain-related well-being, even months after doing their chemotherapy.4
The challenging part is when you have the patient who’s frail and not…willing to do more chemotherapy. That comes back to clinical practice, and the data are there. But if a patient is not of adequate performance status or has some other comorbidity, then it becomes more challenging. We have some new data that might help those patients.
Do the genomic tests help sway your choice of therapy?
Most of the tests will highlight any number of mutations that will clearly suggest these agents are not helpful. In my practice, those are things we know are not likely to work. [First], you have the profile of the patient. For example, if someone runs through the first agent in 3 or 4 months, I have much less confidence in the second or third agent. But if people, for some reason, persisted on an agent for quite a while, I’ll recheck. There does not seem to be a mutation in the AR access. That comes into play when I choose what’s best for that patient or work with them to pick a choice, particularly if they are not interested in chemotherapy or cannot do chemotherapy and they don’t have other options, such as homologous recombination repair mutations or microsatellite instability-high mutations.
A lot of key points have hit on the [questions]: What about the patient? What are the patient’s choices, wishes, and comorbidities to help choose the next best thing for them?
What are some more recent data in this setting?
The VISION study [NCT03511664] is a phase 3, open-label study of protocol standard of care plus or minus lutetium-177–PSMA-617 for PSMA [prostate-specific membrane antigen]–positive castration-resistant prostate cancer.5 This study looked at patients that had treatment with both an AR pathway inhibitor and 1 or 2 taxane regimens, so there has been some notable treatment history. They were allowed to begin standard-of-care treatment before randomization, ECOG performance status 0 to 2, and they had to have a positive PSMA scan on PET/ CT with gallium.
The patients were able to receive up to 6 cycles of lutetium in addition to their standard-of-care regimen vs the standard-of-care regimen alone. They were randomized according to ECOG status, visceral metastases, and AR pathway inhibitors in their [prior] standard-of-care treatment, and they were imaged with CT and MRI bone scans similarly every 8 to 12 weeks.
Alternate primary end points existed, meaning if either of these was met, the study would be deemed positive. That was radiographic PFS or OS with secondary end points, including systematic skeletal events and changes by RECIST response rate and disease control rate.
Screening took place with 1179 patients. They had to have a positive gallium PSMA PET/CT, [which] meant the reading or any spot identified was higher than uptake within the liver. Approximately 86% of those patients met that criteria and 831 were randomized. Patients began enrollment in June 2018. After a couple hundred patients, there was notable dropout in the standard-of-care arm alone. This was because of certain sites pulling out of the study for various reasons, including PSA change or not being part of the intervention arm, so they kind of reset the clock with the blessing of the FDA and continued with the 2:1 randomization, 831 randomized. Of note, there was low enrollment of patients who were Black and African American or Asian.
With OS, patients who receive lutetium-177–PSMA-617 plus their standard of care had an increased median OS 15.3 vs 11.3 months, a difference of 4 months, which was a hazard ratio of 0.62 and statistically significant [95% CI, 0.52-0.74; P < .001].5 This benefit was observed across most prescribed subgroups. The ones that did not show benefit had wide confidence intervals likely related to low numbers. With radiographic PFS, there was a median [PFS of] 8.7 months with lutetium plus standard-of-care arm vs 3.4 months in the standard-of-care arm alone, hazard ratio of 0.40, and the P value was significant [95% CI, 0.29- 0.57; P < .001].
With treatment-emergent AEs, we can imagine with this type of molecule—which is basically radiopharmaceutical— there was notable fatigue and bone marrow suppression with pancytopenia that was more prevalent in the lutetium arm.5 [There was] dry mouth, nausea, and vomiting, but it was reasonably well tolerated [overall].
What has your practical experience been with using PSMA imaging?
This is something where patients hear about it and seek the technology, but we’re behind. Our nuclear medicine colleagues at Emory [University] have [experience with PSMA imaging]. They were leaders with the fluciclovine-based imaging. There are research studies looking at salvage approaches with PSMA-based imaging, but the gallium is unique in where it can be produced [and the] delivery time frames, and having gone through the Axumin PET/CT process, we’ve seen how long it takes. Not so much for it to become approved, not so much for it to be available at a readily accessible site, but trying to get it to the number of institutions and places where these tracers and radioligands are being produced can make it challenging in a timely measure.
The other thing is that once these things are approved, are these going to be in [rural] populations or in inner cities where there may be a very diverse population? Here in the Southeast, are people in rural areas going to be able to have access to these agents? There are going to be some challenging things to overcome. It may be, as with many of the approved agents, that this may not be the site [or space] in which the agent ends up being utilized the most. We’ve seen many approvals in the castrate-resistant setting status post multiple lines of therapy, but they move up. Who knows? It might be that there’s a bigger benefit earlier. I think those are going to remain very active questions for this agent, and accessibility is very much going to be an issue.
Even though we are getting new technology and new radiotracers for therapy, is the insurance barrier an issue?
It’s taken some time to have the insurance companies catch up. Even in those regards, there’s a wide differential on approval. Some insurance companies will deny a patient that may very well benefit someone who has no other site of disease, PSA rising. This is a patient where there may be some way to salvage and disrupt their pathway of pathophysiology. Other places where I’ve had patients want Axumin PET scan, insurance pays for it, and that’s not for monitoring as you go along. I agree that a lot of this is going to have to catch up or even be introduced to the insurance field and some type of experience with approval.
[Going back to our] case, the biology is very complex with notable heterogeneity. Understanding disease biology is going to evolve and influence management in therapeutics, and sequencing is going to become even more important as we think of treatment planning. Androgen deprivation therapy remains a foundational therapy, but many studies are suggesting that switching the mechanism of action, such as with the CARD trial, is associated with improvement of survival.4
REFERENCES:
1. NCCN. Clinical Practice Guidelines in Oncology. Prostate cancer, version 1.2022. Accessed October 23, 2021. https://www.nccn.org/professionals/physician_gls/pdf/prostate.pdf
2. Abida W, Campbell D, Patnaik A, et al. Non-BRCA DNA damage repair gene alterations and response to the PARP inhibitor rucaparib in metastatic castration-resistant prostate cancer: analysis from the phase II TRITON2 study. Clin Cancer Res. 2020;26(11):2487-2496. doi:10.1158/1078-0432.CCR-20-0394
3. de Wit R, de Bono J, Sternberg CN, et al. Cabazitaxel versus abiraterone or enzalutamide in metastatic prostate cancer. N Engl J Med. 2019;381(26):2506-2518. doi:10.1056/NEJMoa1911206
4. Fizazi K, Kramer G, Eymard JC, et al. Quality of life in patients with metastatic prostate cancer following treatment with cabazitaxel versus abiraterone or enzalutamide (CARD): an analysis of a randomised, multicentre, open-label, phase 4 study. Lancet Oncol. 2020;21(11):1513-1525. doi:10.1016/S1470-2045(20)30449-6
5. Morris MJ, De Bono JS, Chi KN, et al. Phase III study of lutetium-177-PSMA-617 in patients with metastatic castration-resistant prostate cancer (VISION). J Clin Oncol.2021;39(suppl 15):LBA4. doi:10.1200/JCO.2021.39.15_suppl.LBA4