Roundtable Discussion: Hamilton Compares Therapy Options and Sequencing for Recurrent TNBC
During a Targeted Oncology case-based roundtable event, Erika P. Hamilton, MD, discussed the choice of first- and second-line therapy for a patient with triple-negative breast cancer following adjuvant chemotherapy.
Erika P. Hamilton, MD (Moderator)
Director, Breast Cancer and Gynecologic Cancer Research
Sarah Cannon Research Institute
Nashville, TN

HAMILTON: Does anyone want to tell me what they picked and why?
KHASAWNEH: There is no wrong answer here, [in my opinion]. TNBC is definitely an orphan disease; survival is lowest among all breast cancer categories. She progressed 8 months after adjuvant dose-dense AC followed by paclitaxel. She’s definitely in trouble, and most likely she’ll succumb to her disease, given her young age.
The best option for her, in my opinion, would be to enroll in a clinical trial because all other options can be given through standard of care, but a clinical trial would be the best option to try to explore any novel agents, or a novel combination of the approved agents on the market.
HAMILTON: Yes. Anybody else want to weigh in?
CARR: I was going to say the same thing that Dr Khasawneh said. This is a young woman with recent adjuvant therapy who relapsed early—a clinical trial is what we would do.
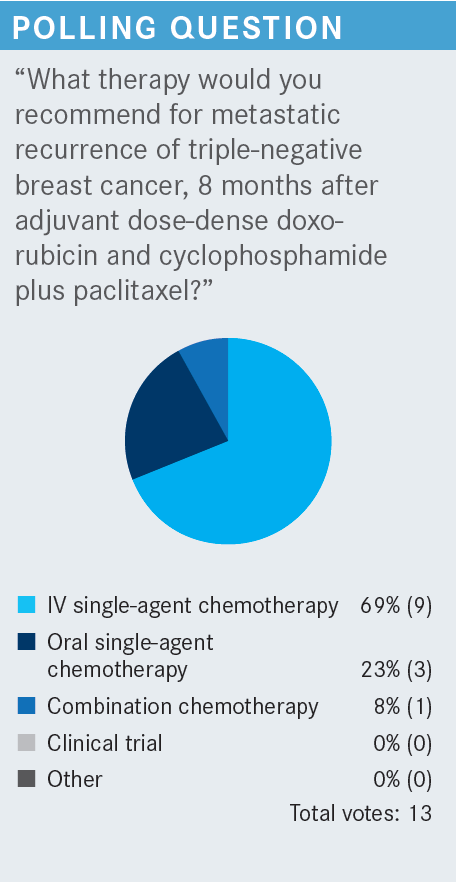
HAMILTON: Yes, exactly. I would definitely do a clinical trial too. I don’t tend to use a lot of combination chemotherapy, but this patient relapsed pretty quickly, 8 months after her AC to paclitaxel. So I think I may be leaning toward a combination, gemcitabine [Gemzar] and carboplatin or something like that. But then, at the same time, she has pretty low burden of disease. She has only 2 small lung lesions and 1 liver lesion. I think an IV single agent would be appropriate. But I agree, especially for our patients with TNBC, where iterative care is just not ideal, I’m thinking of a clinical trial.
MAHESHWARI: Yes, I think in a case like this, whatever we do, survival for the next year is very limited. If somebody failed AC followed by paclitaxel, [her chance of survival is poor].
HAMILTON: Right. I agree. She got 3 great chemotherapy agents, and she’s progressing afterward. You don’t have much hope that the fourth is the miracle one.
MAHESHWARI: Yes. Thank you.
HAMILTON: With a bit more indolent disease, I’d probably think about single-agent chemotherapy and not pulling out combination chemotherapy at this time. What regimen would you pick? What chemotherapy, single agent, would you give her if you had to pick at this point? Would you recycle a taxane? Would you do something else?
NIDHIRY: I would probably do a single-agent taxane, like paclitaxel with albumin [Abraxane], or probably carboplatin.
HAMILTON: Does anyone else want to weigh in on what they might pick if it weren’t a clinical trial?
KUZUR: Eribulin [Halaven].
GIAN: Yes. That’s what I was going to say, eribulin.
KUZUR: There’s also the new drug, sacituzumab [Trodelvy], as well?
HAMILTON: Yes, with sacituzumab govitecan we often have trouble getting it reimbursed for the first line because it’s approved for the second line and beyond. Same with eribulin, actually. Sometimes if patients have had neoadjuvant [or] adjuvant chemotherapy, you can [give sacituzumab] if they relapse quickly, but I don’t know that we’d get it through insurance here with the 24-month gap.
KUZUR: These patients [with TNBC] always make me nervous. They are young, and they’re going to [have potentially poorer results], regardless of anything we do. That’s why I believe in a clinical trial.
HAMILTON: Yes, absolutely.
HAMILTON: [For] the patient with recurrence 8 months after receiving adjuvant dose-dense AC-paclitaxel, what do we recommend as second-line therapy for this patient with metastatic [TNBC]? She got dose-dense AC to paclitaxel, [her disease] relapsed in 8 months, and she got gemcitabine and carboplatin. What’s your next choice?
GIAN: I would go ahead with the eribulin at that point, if she couldn’t get on a clinical trial.
HAMILTON: A lot of you picked sacituzumab. What’s your experience there?
CARR: I haven’t given it yet, but I know it’s an antibody-drug conjugate, and that’s kind of a hot topic. The alternative options are not that appealing; other than eribulin, which we probably won’t get too much out of either in this scenario. I think that’s by default where I was headed.
HAMILTON: Has anybody else used sacituzumab?
GHANEM: I have used it a couple of times and have had a good experience with it. It is a well-tolerated treatment. The problem with these patients [with recurrent TNBC] is [they have] very aggressive disease. Both of them did well, actually. I don’t recall the response rate that I got in these 2 cases. One of them responded well; the other one had very aggressive disease. She progressed clinically even before I did scans, and then I had to switch again.
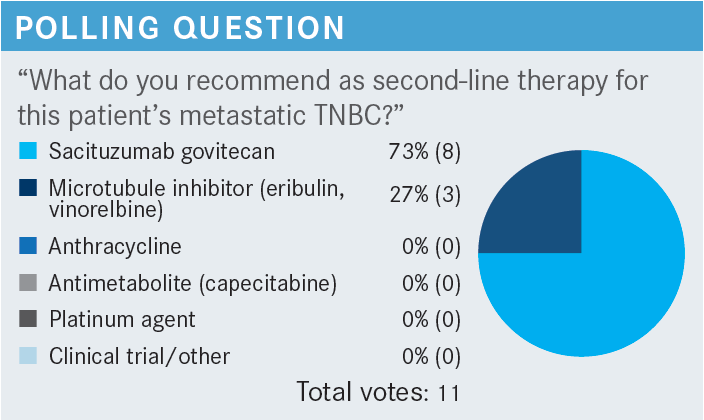
HAMILTON: Yes, I think maybe the most striking thing about the sacituzumab trial [ASCENT; NCT02574455] was that the other arm was a treatment of the physician’s choice, and you could pick [therapies] like capecitabine [Xeloda], vinorelbine [Navelbine], or eribulin, etc.1,2
But for the standard-of-care arm in that third-line setting and beyond, the median progression-free survival [PFS] was 2 months. So what we consider [to be] good chemotherapy for TNBC is giving us only a 2-month benefit. And obviously, sacituzumab clearly beat that, with significant improvement.
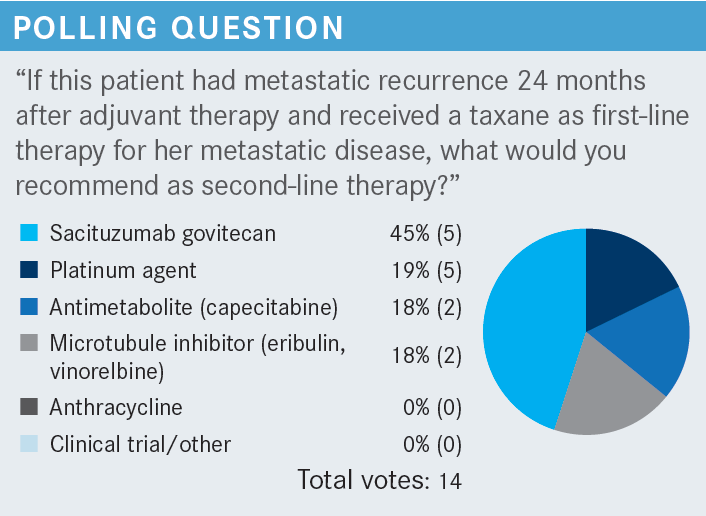
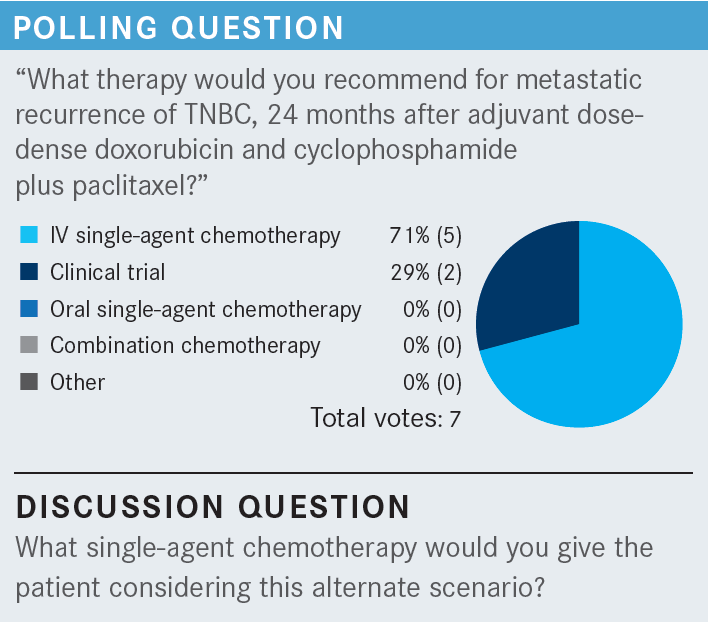
HAMILTON: About half [of the participants] chose sacituzumab, and then [some chose] a platinum agent, eribulin, or capecitabine. Any comments about what drove you to change your answer there?
CARR: I chose a platinum agent. If I recall, this patient has pretty low-volume disease, and this would be second line, and she’s triple negative; so I thought maybe some platinum agent might be useful here to drag things along a little bit, and save the sacituzumab for later on.
NIDHIRY: I chose platinum as well, for similar reasons. Because the patient seemed to be responding to chemotherapy, I thought it was reasonable to use that. I thought sacituzumab was approved as a third-line agent, if I’m not mistaken.
HAMILTON: You’re right, the clinical trial was third line. What about those of you who picked sacituzumab?
WILLIS: I probably would have thought about sacituzumab. Isn’t it second line now?
HAMILTON: It is, yes. They expanded the indication; it now has approval for second line.3,4
KONALA: She received different agents with chemotherapy; she had AC and dose-dense paclitaxel. It could be good to use a different mechanism of action. It has been proven in the second- and third-line settings, so I chose sacituzumab. We can use carboplatin anytime.
HAMILTON: That’s a good point.
HAMILTON: [We are discussing] the patient with metastatic recurrence 8 months after the dose-dense AC to paclitaxel, who got first-line gemcitabine and carboplatin, had the partial response lasting 6 months, and now has new liver metastases.
What do you think when you’re trying to sequence agents? What goes into your thinking there? Are you thinking about the long haul and tolerability, or are you thinking about what is different that the patient hasn’t seen? How are you choosing what agents you give, and what sequence? I think it’s an important question.
WILLIS: I think a lot of it depends on what your molecular studies show you. At some point in the metastatic setting, we probably would have done a panel and found something that we hope we can target. So if BRCA1 or BRCA2 are positive, or PALB2, then we might consider looking at a PARP inhibitor.
If they’re PD-L1 positive or high, you’d maybe think about some type of agent with a PD-L1 inhibitor somewhere in there. And outside that, if you haven’t used sacituzumab, that might be the point [to use it]. And of course, always, you consider clinical trials that might be in the area too.
HAMILTON: Yes, I think that’s great. So, Dr Willis, let’s assume that this patient [has] BRCA wild-type and PD-L1– negative [disease]. How would you sequence? Let’s say she gets gemcitabine and carboplatin first. What are you thinking about for the second [and third lines]?
WILLIS: If she gets gemcitabine and carboplatin first, I’m thinking about sacituzumab if I haven’t used it already. Then after that, a lot of it depends on the patient’s performance status, and I’d be looking at possibly capecitabine. That’s about all I have left.
ZAYDAN: [The first thought that comes to mind] is to consider something that has a different mechanism of action….And second, her current situation, her previous toxicity, and the toxicity of the drug I’m going to use. For example, sacituzumab [can cause] severe neutropenia. Now, if she had a history of neutropenia, or if she has a history of diarrhea, I would be very concerned.
HAMILTON: If she were getting gemcitabine and carboplatin first, what would be your second-and third-line picks?
ZAYDAN: At this point, I would choose eribulin or vinorelbine. I have used vinorelbine and had some success with it.
KONALA: This patient has [had recurrence] after 8 months off chemotherapy. We discussed a clinical trial as a good option. There are some trials combining sacituzumab with immunotherapy. If I can get her on that trial, I would consider that.
HAMILTON: So that’s second line?
KONALA: Yes.
HAMILTON: What would you give third line, after sacituzumab?
KONALA: I would probably go back to chemotherapy.
HAMILTON: What’s your chemotherapy of choice?
KONALA: She already received gemcitabine and carboplatin. We have to try a different mechanism; I’m thinking capecitabine or eribulin after that. I’m hoping we’ll get a different antibody-drug conjugate as we are getting in other cancers.
NIDHIRY: I’d probably go with sacituzumab as a second-line therapy because the patient is progressing on the chemotherapy treatments. And if they progress further, probably a clinical trial or maybe something like eribulin.
GAIN: At every stage, I would try to put them on a clinical trial first because I don’t think it matters what you use. For second-line therapy, I think you have to look up at how [frail] the patient is as well. If the patient is [frail] and their performance status is down, then you probably want your most active drug second; that would be the sacituzumab. Then you could save other agents such as vinorelbine or eribulin or capecitabine after that. Because they may not get to it, and you want to go with whatever you have that has the best chance of working.
If they have great performance status, feel great, and are doing well, you could try [an agent like sacituzumab]. If it’s been a longer remission, [such as] 24 months, you could try something milder, such as eribulin, and then save sacituzumab for third-line therapy.
KHASAWNEH: I agree with all my colleagues. There aren’t set-in-stone guidelines for which one to use. I think it’s a clinical decision, a joint discussion with the patient. But something I always look at is whether there are any residual adverse events [AEs] from previous regimens, like neuropathy.
There is the performance status, the fatigue, the degree of myelosuppression, and the current blood counts. If their blood counts are low, I try not to use a very myelosuppressive regimen, or I start at 75% of the original dose, especially for microtubule inhibitors. And neuropathy is tough to deal with, especially if you’re starting sacituzumab or microtubule inhibitors.
I at least have a discussion with the patient that these things can get worse with the agents I’m going to use, subsequently. But I agree with all my colleagues. I don’t think there are set guidelines for which agent you can use. It’s a shared decision.
HAMILTON: Yes, you’re absolutely right; compared with HER2-positive disease, where we have things pretty well scripted, in TNBC, there’s not even 1 standard of care in the first-line space. We cycle through regimens.
KUZUR: Sometimes I recycle the paclitaxel, especially if it’s been 2 years or more, and I find the weekly paclitaxel single agent can still give some benefit after you’ve run through the other agents.
HAMILTON: What is your experience in terms of tolerability? Do you find the diarrhea hard to manage, easier than with the TKIs [tyrosine kinase inhibitors]? How are you counseling your patients about this drug?
KHASAWNEH: I thought the diarrhea is easier to control compared with [what] larotinib [causes], for example; just loperamide [Imodium], maximum 8 pills per day, and diphenoxylate and atropine [Lomotil] were sufficient to get the patient through. Fatigue and neutropenic fever were bothersome and disturbing in one patient I had. But she was able to get about 8 months before progressing.
HAMILTON: You mentioned neutropenia. How did you manage that neutropenia? Did you try to use growth factor? It’s a little bit trickier on day 1, day 8, with day 15 off. You can’t give pegfilgrastim [Neulasta] after the first dose, etc. How did you manage the counts?
KHASAWNEH: As you mentioned, it’s hard to add pegfilgrastim in a regimen that has day 1, 8, and 15 of a 21-day cycle. For those patients, you’ve got to keep your fingers crossed that they do not develop neutropenic fever. She had pneumonia requiring admission to the hospital. After that, we were able to add filgrastim [Neupogen] for a couple of days after day 15, to bring up the counts to a satisfactory level before each cycle, we hope. But I could not get pegfilgrastim approved.
WILLIS: Yes, I did get a chance to get pegfilgrastim approved, but I gave it after day 8, and she did just fine. In other cases, I did a dose modification and decreased the dose level by 1 step, and I was able to continue it without any problems.
GHANEM: For the diarrhea, it’s usually well managed with antidiarrhea medications; it’s not an issue, not like [what we see with] everolimus [Afinitor] or other chemotherapeutics that we use. So, to me, both patients [I treated with sacituzumab] did well.
[Regarding] the neutropenia, both of these patients were third line and already [had] pancytopenia on starting this treatment. I used to bring them early in the week and do the complete blood count. If the patient [had pancytopenia], I gave filgrastim. For most of these patients, by the end of the week, I was able to give the chemotherapy. It’s more of an issue if it’s given later vs in the second line. My experience was good, and [sacituzumab] was very well tolerated.
HAMILTON: Good to hear. I do something similar. I don’t necessarily have a one-size-fits-all [approach]. I’ve been successful with some patients with mildly low counts, getting away with the “day 1 goes fine, get to day 8, give day 8, and then give pegfilgrastim.” And then patients’ counts are OK by day 21 and the start of the new cycle.
And then, for other patients who have struggled, it’s tough. Because with filgrastim, most often, we can’t get coverage for patients to do that at home, and nobody wants to drive back to the clinic for multiple days of filgrastim. So sometimes I’ve used a dose reduction there with some success.
I think you can pair things. I agree about the diarrhea. I’ve had one patient who had bad diarrhea and a handful of others who have had very minimal to not much diarrhea. I’ve got some patients who have no diarrhea at all. Other patients take 1 loperamide in the morning and they’re good, which is not that much of a crimp on their lifestyle.
CARR: The data look great, of course [From the Data2]. Median overall survival doubled, and PFS [tripled].1,2 When you see a PFS of about 6 months, it’s not impressive to most physicians; but in this case, it is. That gets you through maybe 2 scans, where you can give a patient some good news and a bit of benefit where they may have not had that result with the previous scans. So it gives them something to celebrate in this situation. Overall it looks good. I think everybody would agree with that, compared with the physician’s choice or other chemotherapies we use in this space.
HAMILTON: Yes, I agree. Normally, we don’t [celebrate] over several months [of PFS], but several months, when it’s a tripling of what we have, isn’t so bad. At least, it gets patients through 1 scan without bad news.
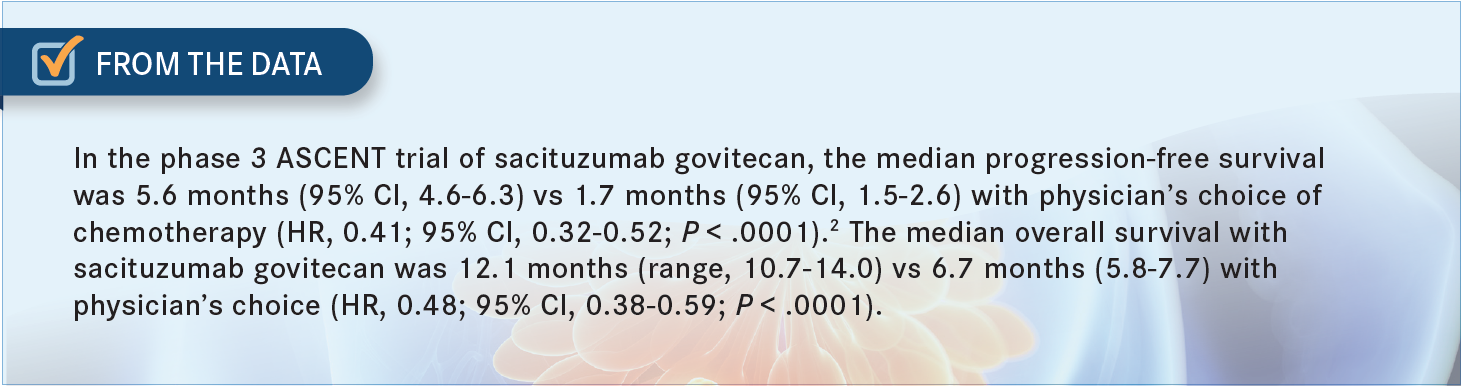
NIDHIRY: I agree. This is a disease with minimal treatment options, and I think it’s reasonable to consider using it in the second-line setting, once [patients] progress on the first-line chemotherapy treatments, because there’s a modest improvement in benefit compared with what we have now. So I would definitely consider using it in the second line.
HAMILTON: What about molecular testing? What are you doing, and do any of those results factor into what you think about sacituzumab or whether you would use it?
GIAN: Oh, absolutely. I think that should be done up front anyway in this scenario. Because if you have a good clinical trial that’s limited to 1 prior therapy, or it has to be given second line, in this situation, you’re going to want to go ahead and use that clinical trial while you can. And then, [sacituzumab] would fall to the third line.
So I think everybody gets tested, at least my patients, and I think you have to look at clinical trials. Even with this breakthrough, and this drug is impressive, it’s not going to be a curative drug. So whatever else you can offer them is still very important here, and that’s going to be based on next-generation sequencing.
HAMILTON: Yes, I think you bring up a good point. That information helps you with what line you are using regimens and whether there is a certain time that you need to use something else. Certainly, that’s the case for PD-L1 testing; we’ve got to [test] that right out of the gate. We’ve got to be doing it first line, or we lose the opportunity.
GHANEM: Yes, I don’t start anyone before I do BRCA1, BRCA2, and PD-L1 [testing] at least. It helps you even with choosing the chemotherapy. If the patient is BRCA positive, you would lean toward a carboplatin regimen, and [also] if the patient is PD-L1. So I don’t start treatment before I do the molecular and genetic testing.
WILLIS: I also always try to make sure I do the molecular panels and the genetic testing as early as I can, so I can direct them toward a particular clinical trial or give them the most appropriate agent. In those molecular panels, one of the new targets—and I know that with the sacituzumab, they are looking at Trop-2 as a possible target, especially—I think it’s more than 80% of patients with TNBC also have Trop-2, so I don’t know how that correlates with the response rate, but I think it’s something that I would look at in terms of moving it to second line vs third line.
HAMILTON: Yes, you’re right. We don’t have any data right now about needing to use Trop-2 to pick who is or is not eligible or who might respond to sacituzumab. So what are you going to use most often as the next therapy after sacituzumab? Are you picking that based on ease of administration, based on what AEs the patient may have, and what you think they might tolerate best?
HEMPHILL: At that point, this is all palliative. It’s the AE profile. [I might choose] capecitabine, potentially, just to keep them out of the clinic, so they can enjoy their families as much as they can, because we know it’s inevitably going to [progress eventually].
But for sacituzumab, is there any clinical benefit whatsoever in the low ER/PR [estrogen receptor/progesterone receptor] level, like the old WHO [World Health Organization] definition, less than 10%? Would you still think about it, given the significant improvement for the patients with TNBC?
HAMILTON: I definitely would. Those patients were not included in the clinical trial. We enrolled another clinical trial for the ER-positive patients. [According to data presented at the 2022 American Society of Clinical Oncology Annual Meeting,] sacituzumab did beat standard chemotherapy in the third-line setting for hormone receptor–positive patients.5 I anticipate an approval for ER-positive patients by the end of the year.
I think that brings up a good point between clinical trials and real-world settings. Clinical trials often require an ER of 0, but what about our patient [who has an] ER expression of 10%? You’re not going to rely on endocrine therapy in that patient, yet they’re not strictly triple negative. And many patients, unfortunately, fall into that gray window. But yes, I think very soon you will be able to use sacituzumab for patients with HER2-negative disease, triple negative, or hormone receptor positive. That was a good question.
HAMILTON: If you aren’t using sacituzumab in the second line, what are you using, and why? Are you thinking, “It’s a new drug, and I just don’t feel as comfortable with it for my patients yet”? Is there something about it you don’t like? Or had you not yet heard the good news that you could be using it in the second line?
ZAYDAN: I’m reserving it as third or fourth line after I try my other options. I am concerned about the AEs. And psychologically, if I use sacituzumab, and it fails, what do I do next?
WILLIS: I’m thinking that second line makes the most sense, in terms of using your best drug that you have. Because when you look at quality of life—honestly, when I see folks getting other regimens, you see that the response rate isn’t that good, and also, every time you give a regimen, it’s just that quality of life is going to take a hit every time.
The AE profile is good. Honestly, I have a hard time giving eribulin, in terms of the neutropenia, in terms of the frequency of dosing. So I don’t see that much difference because you give it on the same [schedule] as you do the sacituzumab.
HAMILTON: Yes, on days 1 and 8?
WILLIS: Yes, so I think it’s a very good agent. One of the big issues that some physicians may have is that initially everybody thought it was going to be approved, and suddenly it got niched and pretty much put off for about a year. I think that’s what makes some people uncomfortable.
But I couldn’t wait for it to come out. I was disappointed when it didn’t come out initially. I like the agent, and I honestly think it should be second line, in terms of that healthy patient or that young patient who’s out there. Some of the patients I’ve treated with it, we talk about that 1 year [median OS]; I’ve not seen that with any other agent. I’m always having to change the agent. So I’d want to give them the best agent up front, especially if the toxicity profile is pretty good.
HEMPHILL: I agree with Dr Willis. From the efficacy and pretty minimal toxicity standpoint, I think it [should be] definitely [used in the] second line.
HAMILTON: Do you care about the survival, the PFS, the response rate, time to response? What do you think is most important for you and your patient?
WILLIS: I am a huge fan of the clinical benefit ratio. I know that at this stage, most patients may not respond. They may have stable disease [SD]. And I like clinical benefit as the best measure when I’m dealing with someone with metastatic disease who I know I may not be able to cure, but I may be able to help them.
HAMILTON: Yes, so you’re looking for [no progressive disease]?
WILLIS: Correct.
GIAN: I concur with that.
ZAYDAN: They are all important. The patient is thinking of survival, but as a physician I think PFS includes everything, practically; like how long it will take for progression, even if [their response] is SD. I think PFS is the best measure I look at.
REFERENCES
1. Bardia A, Tolaney SM, Loirat D, et al. LBA17 - ASCENT: a randomized phase III study of sacituzumab govitecan (SG) vs treatment of physician’s choice (TPC) in patients (pts) with previously treated metastatic triple-negative breast cancer (mTNBC). Ann Oncol. 2020;31(suppl 4):S1149-S1150. doi:10.1016/annonc/annonc325
2. Bardia A, Hurvitz SA, Tolaney SM, et al; ASCENT Clinical Trial Investigators. Sacituzumab govitecan in metastatic triple-negative breast cancer. N Engl J Med. 2021;384(16):1529-1541. doi:10.1056/NEJMoa2028485
3. FDA grants regular approval to sacituzumab govitecan for triple-negative breast cancer. FDA. April 7, 2021. Updated April 8, 2021. Accessed November 23, 2021. https://bit.ly/3fOWhUD
4. Gilead statement on new NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines) recommendation for sacituzumab govitecan-hziy (Trodelvy) in second-line and later metastatic triple-negative breast cancer. Gilead Sciences. September 27, 2021. Accessed August 11, 2022. https://bit.ly/3BV7hLb
5. Rugo HS, Bardia A, Marmé F, et al. Primary results from TROPiCS-02: a randomized phase 3 study of sacituzumab govitecan (SG) versus treatment of physician’s choice (TPC) in patients (Pts) with hormone receptor–positive/HER2-negative (HR+/HER2-) advanced breast cancer. J Clin Oncol. 2022;40(suppl 17):LBA1001. doi:10.1200/JCO.2022.40.17_suppl.LBA1001
Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More