Roundtable Discussion: Comparing Triplet vs Quadruplet Regimens as Maintenance for NDMM
A 54-year-old woman received a diagnosis of Revised International Staging System stage II multiple myeloma. Marc J. Braunstein, MD, PhD discussed the case with a group of peers.
Marc J. Braunstein, MD, PhD (Moderator)
Assistant Professor, Department of Medicine
Course Codirector, Hematology- Oncology System
NYU Long Island School of Medicine
Mineola, NY

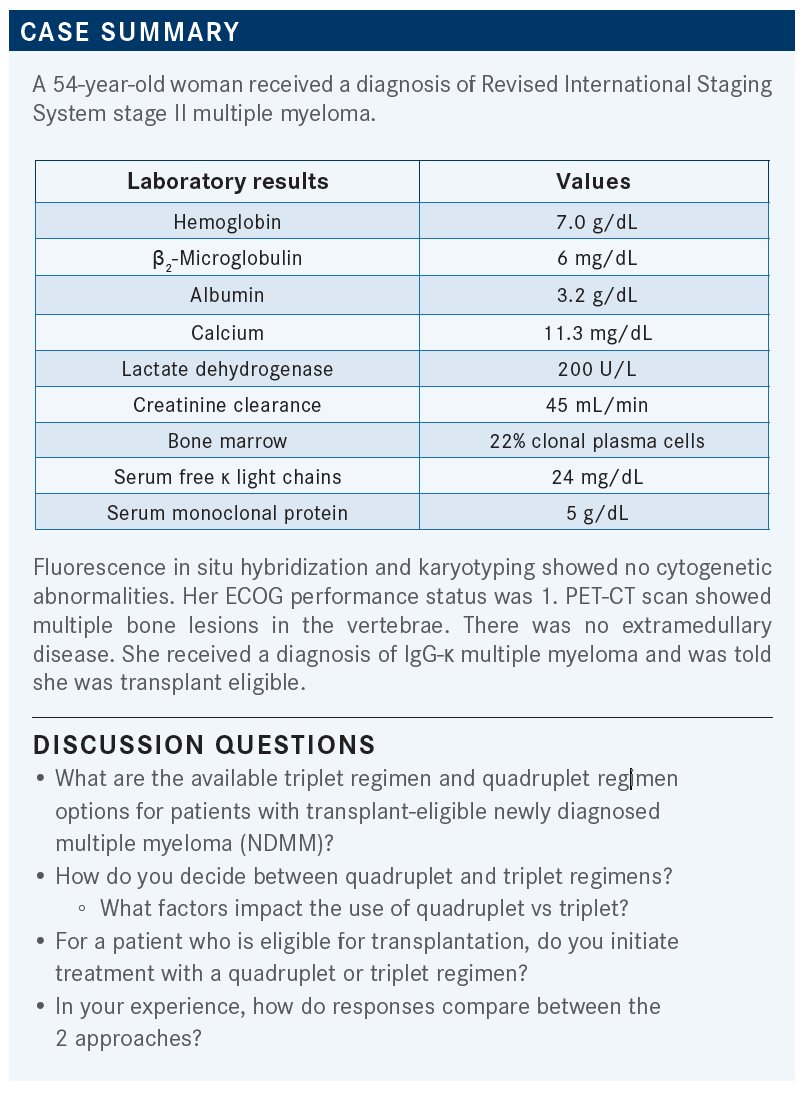
BRAUNSTEIN: In multiple myeloma, if you ask a panel of experts a question, you’ll get 10 different answers. There are various regimens; what are some of the most common ones that you’ve adopted in your practice?
WIEDER: It depends on the age of the patient. It’s not so much age in and of itself, but [more so] transplant eligible vs ineligible. For a younger, healthier person, typically I would use a 4-drug regimen, but let’s say a 3-drug regimen, mostly bortezomib [Velcade], lenalidomide [Revlimid], and dexamethasone [VRd], as opposed to adding daratumumab [Darzalex], just because of comfort and having prescribed [that triplet] over the years. But the daratumumab regimen, D-VRd, is certainly very reasonable and probably just as good as the VRd regimen.
BRAUNSTEIN: I think they’re both highly effective regimens, with perhaps deeper responses [achieved] by adding daratumumab, but still both highly effective. Does anybody else want to share their practice pattern, what they prefer as a triplet or quadruplet regimen up front?
ALI: I agree with VRd or D-VRd. Both are good, I think, for transplant-eligible patients, as you mentioned, and both are very well tolerated.
BRAUNSTEIN: It seems like we’re a fairly homogenous group in terms of favoring VRd. For patients who present with renal failure and who maybe have a creatinine clearance less than 40 mL/min—in this case, it was 45 mL/min—I might consider starting with cyclophosphamide [Cytoxan], bortezomib, and dexamethasone [CyBorD] or daratumumab plus CyBorD and then switching to lenalidomide after 1 cycle if their creatinine clearance improves.
Dr Wieder, you spoke about the fitness or transplant eligibility of the patient. Are there any particular comorbidities that would lead you more toward a quadruplet regimen with a monoclonal antibody [vs] a triplet regimen, or does every patient just get a quad up front because it’s the most intensive regimen we have?
WIEDER: Typically, I haven’t been using much of the quadruplet regimens, because I haven’t had a lot of experience with it, I think that the toxicity is definitely higher, and I’m not sure how much more [advantage] you’re going to get from it. You definitely get a better response. The question is, is it so much better that it’s worth it, to get the patients to transplant? So I’ve been doing mostly triplets, but I think in a very young patient who has bulky disease, if they could tolerate it, the main option that I would consider would be a 4-drug vs a 3-drug regimen.
BRAUNSTEIN: If you had a patient you felt would benefit from a 4-drug regimen, are there any particular comorbidities that would make you a little more hesitant to give a 4-drug regimen?
WIEDER: Not in particular. I think that lenalidomide should probably be used with caution in kidney disease, but the fourth drug that I’d typically be adding would be daratumumab. I think daratumumab, in and of itself, doesn’t have any specific contraindications to using it, so to me, patients who have a good performance status and few comorbidities can tolerate a 4-drug regimen.
BRAUNSTEIN: How about the fact that this patient was anemic to start, which we assume is related to her disease burden? Do you have any hesitation there to use the 4-drug regimen that’s likely to be more myelosuppressive?
ALI: No, I would [be more inclined to] use a 4-drug regimen because she’s a young patient, and you are absolutely right, her anemia is secondary to her disease, so we need to control her disease, so we can send her for a possible autologous stem cell transplant [ASCT].
BRAUNSTEIN: I completely agree. I think we’re likely to see that anemia improve fairly quickly as you treat her. Another way of phrasing the question: If you have a patient who’s not transplant eligible, do you use a 4-drug regimen or do you give triplets or doublets?
WIEDER: I think [I would avoid using a] 4-drug regimen on those patients for 2 reasons. First of all, the things that are making them transplant ineligible [ie, age or comorbidities] are the same things that would make it very difficult for them to tolerate a 4-drug regimen. [Second,] with a transplant-ineligible patient I don’t want to use up all my weapons at the same time, and I’m not sure how much more [benefit] you’re getting with the 4-drug regimen. I’d rather use the drugs sequentially, rather than together, because I think there might be some added benefit. There’s definitely [greater] toxicity [with a 4-drug regimen]. [When] sequencing the drugs, one after the other or alternating triplets, I’m not sure the patient is losing out on much.
BRAUNSTEIN: Exactly, and I agree. What makes a patient transplant ineligible may also make them less fit—if we’re talking about fitness.
BRAUNSTEIN: Our new oncology fellows just started this past week, and they’re learning the art of how to manage AEs, and we tell them about the different things you can do. You can pause [treatment], you can try to suppress [the AEs], or you can dose reduce. In your experience, which of those options have you had to do, primarily, for patients getting quadruplets or triplets for induction for multiple myeloma, if at all? Maybe you haven’t had any issues and just plowed through the treatment.
BLOKH: I have had a pretty good experience, in that most of my patients breezed through the triplets and even the quadruplet regimens. [I’ve given] daratumumab in combination with [various] triplets.
[One exception is] a patient that I’m still [treating], who has had persistent leukopenia and even neutropenia. Initially, I gave her a daratumumab-based triplet. [Then] I got rid of the daratumumab and the lenalidomide, and then I tried to observe her, and as soon as I gave lenalidomide again, her white blood cell count dropped again. Now I have her on bare-bones bortezomib and dexamethasone, and she still runs low with her white blood cell count. I’m not going to assess the bone marrow, because she has been dropping her [blood cell] counts from the beginning of her treatment, so I think it’s treatment related. I don’t know what to do with her; I’m just giving her filgrastim [Neupogen] shots.
It’s not myelotoxic chemotherapy, so you can give filgrastim shots throughout the process, unlike the precautions we take with traditional chemotherapy. So I give her bortezomib and dexamethasone, and I give her 3 days’ worth of filgrastim shots after the regimen, but she’s coming to the infusion center almost every day of the week, and I don’t know what to do with her in terms of the neutropenia.
BRAUNSTEIN: Yes, there are patients who tend to be more sensitive to these drugs, and you can’t always predict it, and you run into those problems. I totally agree with you; I would give the patient growth factors to try to get them through therapy and not deprive them of the benefit of one of the drugs in the class. There are certainly patients who will develop thrombocytopenia or neutropenia. You can’t dose reduce the daratumumab, but you can try to dose reduce the lenalidomide or the bortezomib. I don’t think it’s unreasonable to give growth factors just to try to get them through, especially in the beginning when they may have less bone marrow reserve because their disease burden is higher. I agree—in my practice I haven’t had that many patients who needed to be admitted for grade 3 or 4 neutropenic fever, but we always worry about infections in these patients at diagnosis.
WIEDER: The drugs are, in my experience, very well tolerated. Any time you use any drug for a long period of time, it’s potentially going to cause some chronic neuropathy and so on. But usually, when you use an induction regimen [for] 4 to 6 cycles, it’s very uncommon that you get any major AEs. The 1 issue that I’ve run into lately, more often than not, is a lenalidomide[-related] rash. I think that’s relatively common compared with some of the other potential AEs. For that issue, I usually hold [the drug], wait for the rash to resolve, and then I reintroduce the drug at a lower dose. But aside from that, I find that the drugs are tolerated very well.
BRAUNSTEIN: Right, I agree. The lenalidomide rash creeps up on you. It’s hard to predict, and it’s something that patients will always call me about because they notice it early on. I try to give topical hydrocortisone or antihistamines or something to try to suppress it just to get them through. And most of the time that does the trick, but sometimes we have to dose reduce….That can be a challenge sometimes.
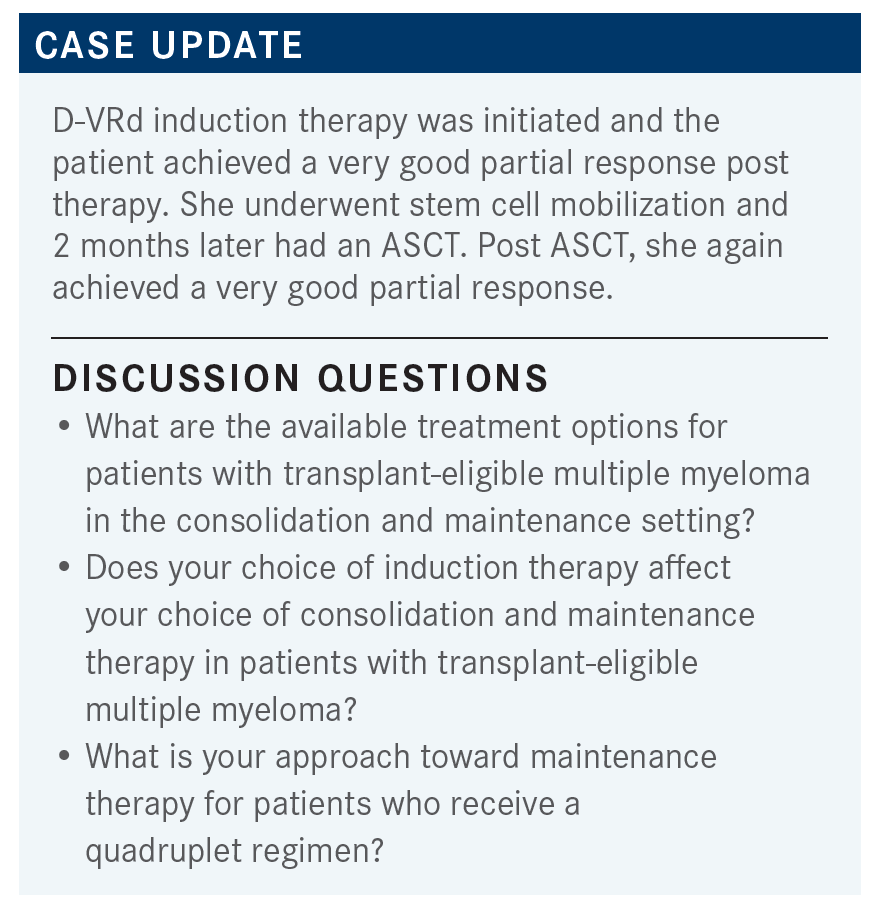
BRAUNSTEIN: If your patient, [who is receiving] a quadruplet regimen, get an ASCT, do you give them 2 cycles of consolidation of D-VRd after the transplant, or do you just move to maintenance? And if you are giving maintenance, are you giving just single-agent lenalidomide, or are you giving the doublet like they did in the GRIFFIN study [NCT02874742] of daratumumab and lenalidomide [From the Data1]?
WIEDER: I typically do approximately 4 cycles [then] send the patient to a transplant consultation. At that point I usually let the transplant team give me direction regarding what to do if the patient is ready for transplant—either to go straight to [transplant] or to continue 1 or 2 drugs for another 1 or 2 cycles, depending upon the scenario. Post transplant, I’ve mostly been going straight to maintenance. I’ve been doing mostly 1 drug, rather than 2, because I think it’s easier for the patient. I give either the lenalidomide as an oral drug regimen [so that they don’t have] to come in as often, or the daratumumab. [With the daratumumab,] they don’t have to worry about taking lenalidomide daily. I haven’t done both, but I’ve done mostly one or the other.
BRAUNSTEIN: Yes, I think that’s perfectly fair. I think if a patient is minimal residual disease [MRD] negative after transplant, you can probably forgo those 2 cycles of consolidation and go right to maintenance. That’s just my practice pattern, but there is an ongoing randomized study [AURIGA; NCT03901963] of patients who are MRD positive after transplant [randomly assigned] to daratumumab plus lenalidomide vs lenalidomide alone. It hasn’t been read out yet.
CHEUNG: Is MRD measured on peripheral blood or on bone marrow? [And is] MRD a useful way to determine [whether] patients [should] go on maintenance or continue maintenance?
BRAUNSTEIN: There’s no peripheral blood assay yet to do MRD testing for multiple myeloma. It is all done with bone marrow samples. The clonoSEQ assay, which is the only FDA-approved assay for looking at MRD status, uses next-generation sequencing of the patient-specific multiple myeloma rearrangement to determine MRD.
The second question is, essentially, how do you practically use MRD? And does it determine your choice about whether a patient should go on maintenance? The MASTER study [NCT03224507] tried to address this question of [using] MRD negativity to de-escalate therapy. I think that’s an evolution in how we make decisions based on MRD.
[Maintenance therapy] remains the standard of care after transplant, regardless of MRD status, but there are newer studies that are looking to see if it’s OK to say, “[If you are] MRD negative, you don’t need to get more maintenance therapy,” which has its own potential AEs. But for now, the convention is still to give maintenance therapy after transplant because it has been shown to improve survival, [although] those survival studies were done before the prevalence of MRD as a clinical tool for multiple myeloma assessment. I would still probably give maintenance therapy, even if the patient were MRD negative.
To anybody else: if you’ve given the quadruplet up front, do you give dual-agent maintenance or single agent?
ALI: [The] transplant specialist usually recommends what to do, how much lenalidomide [to give]. We usually follow that. If a patient becomes MRD negative from induction treatment, will you send them for transplant at that time?
BRAUNSTEIN: To some extent, it depends upon who you’re asking. The transplanters will tell you that MRD is not perfect and that you could still have residual disease. And we know that the patient is likely to relapse at some point eventually, anyway, that they may not be fit enough down the road for a salvage transplant, and that despite the MRD data we have now, [transplant] has still been shown to have progression-free survival [PFS] benefit and, in some studies, overall survival [OS] benefit.
Those who don’t favor transplant up front will point to [results from] the [IFM/DFCI2009] study [NCT01191060] and the DETERMINATION study [NCT01208662], which showed that patients in the nontransplant arm[s] still achieved MRD negativity, and they seemed to do just as well as the transplant group[s].2-5 I think it’s probably practice dependent. Personally, I would probably still pursue the transplant, just because the PFS rates were higher, and in the GRIFFIN study, [treatment] was combined with transplant, and they didn’t use MRD to determine whether patients were going to go for transplant.1,6 But I think we need more data to pin down the answer to that question and determine whether you can use MRD prior to transplant to [determine] if the transplant is critical up front. I think it’s institution dependent.
BLOKH: We used to give bortezomib for patients with high-risk cytogenetics and lenalidomide for everyone else, 10 mg once a day, until disease progression. But now I’m noticing that daratumumab is creeping up in the maintenance setting. In what situations would you use daratumumab vs bortezomib?
BRAUNSTEIN: The National Comprehensive Cancer Network guidelines still recommend maintenance with either bortezomib or lenalidomide plus bortezomib for higher-risk patients.7 To date, I’m not aware of any data showing that daratumumab maintenance impacts the high-risk patients more than single-agent bortezomib or lenalidomide. But there are data [showing] that including proteasome inhibitors, and maybe even dual-agent bortezomib plus lenalidomide, leads to better outcomes for patients with high-risk features.8 The consensus is to treat high-risk patients as intensely as possible, and that probably translates into the maintenance setting as well, but we don’t have the data to answer that yet.
In the FORTE study [NCT02203643], where patients got carfilzomib [Kyprolis] plus lenalidomide maintenance, the high-risk group didn’t necessarily do better in the subgroup analysis,9,10 so I’m not sure we know exactly how to best treat the high-risk patients in the maintenance setting, in terms of using daratumumab or not.
BRAUNSTEIN: I’m interested to know how [the novel induction therapies] influence your choice of transplant. I know you may defer that decision to the transplanter, but do the results of the IFM 2009 study and the DETERMINATION study [NCT01208662], which were fairly similar in their outcomes in showing PFS [benefit] but not necessarily OS [benefit],2-5 impact your decision on whether to give transplants? Do [these results] allow you to stratify patients in terms of who you think might be better suited for transplant?
SIEBEL: For this [decision], I would defer to a transplanter.
BRAUNSTEIN: I think transplanters will likely see [the DETERMINATION study] as being favorable because of the PFS benefit, but I think that it gives you some leverage to discuss with the patient that there are data saying that you could potentially rescue patients with a salvage transplant in subsequent lines of therapy. And, of course, there will be more data with CAR [chimeric antigen receptor] T-cell therapy in earlier lines of therapy, too, and that might impact how we think about transplant. That’s going to take some time.
REFERENCES
1. Voorhees PM, Kaufman JL, Laubach J, et al. Daratumumab, lenalidomide,
bortezomib, and dexamethasone for transplant-eligible newly diagnosed multiple myeloma: the GRIFFIN trial. Blood. 2020;136(8):936-945. doi:10.1182/ blood.2020005288
2. Attal M, Lauwers-Cances V, Hulin C, et al; IFM 2009 Study. Lenalidomide, bortezomib, and dexamethasone with transplantation for myeloma. N Engl J Med. 2017;376(14):1311-1320. doi:10.1056/NEJMoa1611750
3. Perrot A, Lauwers-Cances V, Cazaubiel T, et al. Early versus late autologous stem cell transplant in newly diagnosed multiple myeloma: long-term follow-up analysis of the IFM 2009 Trial. Blood. 2020;136(suppl 1):39. doi:10.1182/ blood-2020-134538
4. Perrot A, Lauwers-Cances V, Corre J, et al. Minimal residual disease negativity using deep sequencing is a major prognostic factor in multiple myeloma. Blood. 2018;132(23):2456-2464. doi:10.1182/blood-2018-06-858613
5. Richardson PG, Jacobus SJ, Weller EA, et al; DETERMINATION Investigators. Triplet therapy, transplantation, and maintenance until progression in myeloma. N Engl J Med. 2022;387(2):132-147. doi:10.1056/ NEJMoa2204925
6. Kaufman JL, Laubach JP, Sborov D, et al. Daratumumab (DARA) plus lenalidomide, bortezomib, and dexamethasone (RVd) in patients with transplant-eligible newly diagnosed multiple myeloma (NDMM): updated analysis of Griffin after 12 months of maintenance therapy. Blood. 2020;136(suppl 1):45-46. doi:10.1182/blood-2020-137109
7. NCCN. Clinical Practice Guidelines in Oncology. Multiple myeloma, version 1.2023. Accessed October 25, 2022. https://bit.ly/2T0mDYS
8. Joseph NS, Kaufman JL, Dhodapkar MV, et al. Long-term follow-up results of lenalidomide, bortezomib, and dexamethasone induction therapy and risk-adapted maintenance approach in newly diagnosed multiple myeloma. J Clin Oncol. 2020;38(17):1928-1937. doi:10.1200/JCO.19.02515
9. Gay F, Cerrato C, Petrucci MT, et al. Efficacy of carfilzomib lenalidomide dexamethasone (KRd) with or without transplantation in newly diagnosed myeloma according to risk status: results from the FORTE trial. J Clin Oncol. 2019;37(suppl 15):8002. doi:10.1200/JCO.2019.37.15_suppl.8002
10. Gay F, Musto P, Scalabrini DR, et al. Survival analysis of newly diagnosed transplant-eligible multiple myeloma patients in the randomized Forte trial. Blood. 2020;136(suppl 1):35-37. doi:10.1182/blood-2020-136907
Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More