Randall Discusses Testing and Treatment Choices for Ovarian Cancer
Leslie M. Randall, MD, MAS, discussed the treatment regimens available for an African American patient with ovarian cancer.
Leslie M. Randall, MD, MAS

Leslie M. Randall, MD, MAS, professor, Department of Obstetrics and Gynecology Division Director, Division of Gynecologic Oncology, Virginia Commonwealth University, discussed the treatment regimens available for an African American patient with ovarian cancer.
Targeted Oncology™: Are you choosing oral regimens over intravenous regimens because of coronavirus disease 2019? Are you making changes to therapy schedules and dosages or choosing different agents?
RANDALL: I’ve tried to change to oral [treatment] where I could. We don’t have a lot of options for oral gynecologic oncology. It’s why the data I’ll be talking about are exciting. Mostly in my purely palliative-intent chemotherapy, I’ve definitely de-escalated doses and schedules. I’ve used more growth factor support, trying to keep people out of the hospital for things that can be prevented, like neutropenia and sepsis. So I’ve changed my practice in that way.
What testing would you order for this patient? Do you typically test for BRCA and somatic mutations? And, if so, how do you test and when?
We have to test for germline mutations, for the benefit of the family and the patient, to understand their breast cancer risks. I think “Do you have to do somatic testing anymore?” is the debate. If you have a patient with a germline BRCA mutation, you don’t need to somatic test.
I think many of us still believe that we need to test in order to counsel our patients on what the magnitude of benefit would be—maybe to [switch] our patients who are biomarker negative off therapy and onto something else sooner, if we felt like they weren’t receiving benefit from niraparib [Zejula]. If the drug is approved for all-comers, do you have to test? I think you still have to get a germline BRCA test, but if you’re not going to change your management based on the results of a somatic BRCA or a homologous recombination deficiency [HRD] test, it’s a great question.
How do you use HRD testing in this patient population?
The Myriad HRD assay accompanied niraparib with the FDA approval [documentation].1 [The manufacturer] had hoped for a companion diagnostic, but they got a complementary diagnostic. It was because the assay was not discriminatory enough to show that the benefit was isolated to the germline in the HRD [population]. There was still a benefit outside that population. Plus, I don’t feel like the [cutoff] point has been sufficiently defined for the Myriad assay.
Interestingly, the Myriad assay includes the somatic BRCA mutations, but it does not include the other mutations. So the benefit of getting a Foundation Medicine Somatic BRCA test, [for example], is that you get all the other mutations, including the microsatellite instability [MSI]. That would be available on many other assay platforms, such as CARIS. But [if] you’re not going outside MSI, you probably wouldn’t use that information in the frontline setting for treatment anyway. We may want to use that later, and then you may want to retest later, because the tumor could change. So I think that we’re all over the map right now in the testing realm, but I think the 1 thing that remains certain is that you still have to germline-test these patients.
Do you explain to patients what the National Comprehensive Cancer Network (NCCN) guidelines say about HRD?
The NCCN guidelines state that in the absence of BRCA mutations, HRD might provide information on the magnitude of benefit of PARP therapy.2
When I first started [practicing], I thought that it was important to counsel patients about [NCCN guidelines], but in my opinion [now], that doesn’t mean a lot to them. They’re either going to respond to therapy or they are not. What the magnitude of benefit was on the women enrolled on a clinical trial may or may not apply to the patient who is sitting in front of you. Every now and then, you have a patient who’s a scientist or physician, or who understands granularity of data, and they want to know those things. But I would say my average patient is not informed by those data.
What are the different molecular testing assays available for this patient?
The Myriad myChoice HRD test is a tissue-based test.3 This measures 3 different phenotypic changes that denote HRD. One of those is loss of heterozygosity [LOH], [and the others are] telomeric allelic imbalance and large-scale state transitions. This gives you a myChoice score. The PRIMA trial used 42 as a cutoff for the score.4 The VELIA trial used the same assay and used 33 as a cutoff.5 The thought is that the lower you set the cutoff, the more sensitive the assay is to pick up HRD; however, those [cutoff] points have never been rigorously tested or rigorously determined by Myriad.
Foundation Medicine has a similar assay called the BRCA LOH assay.6 It’s a complementary diagnostic to rucaparib [Rubraca] that was approved when rucaparib got its platinum-sensitive recurrent maintenance indication, and it reads out a similar score, but, unlike the Myriad myChoice HRD test, it does not include telomeric allelic imbalance and large-scale state transitions. The idea of these assays is to detect BRCA-like changes in the cell for reasons other than a BRCA mutation. This would pick up your RAD51C/D mutations. It would not explicitly diagnose them, but it would pick up that dysfunction. So I call these the phenotypic versus the genotypic assays.
Does the LOH assay from Foundation Medicine have a cutoff?
They have a percentage, but their cutoff has never been studied. The LOH was studied in the rucaparib trial, ARIEL3 [NCT01968213], but that’s the only trial.⁷ The ARIEL2 trial [NCT01891344], which established LOH as a marker of rucaparib sensitivity, was investigated by Elizabeth Swisher, MD, at the University of Washington, and it’s a different LOH assay from the one that was used by Foundation Medicine.⁸
But Foundation Medicine had a commercial assay, and when the program went to phase 3, they needed an assay that could be done commercially if they got approval [of the drug that was] conditional with the companion [assay]. But it did not receive companion designation; it received complementary designation, just as the myChoice got complementary designation for niraparib. The designation applied to both the NOVA and PRIMA trials.3,9
What would you use as therapy for this patient?
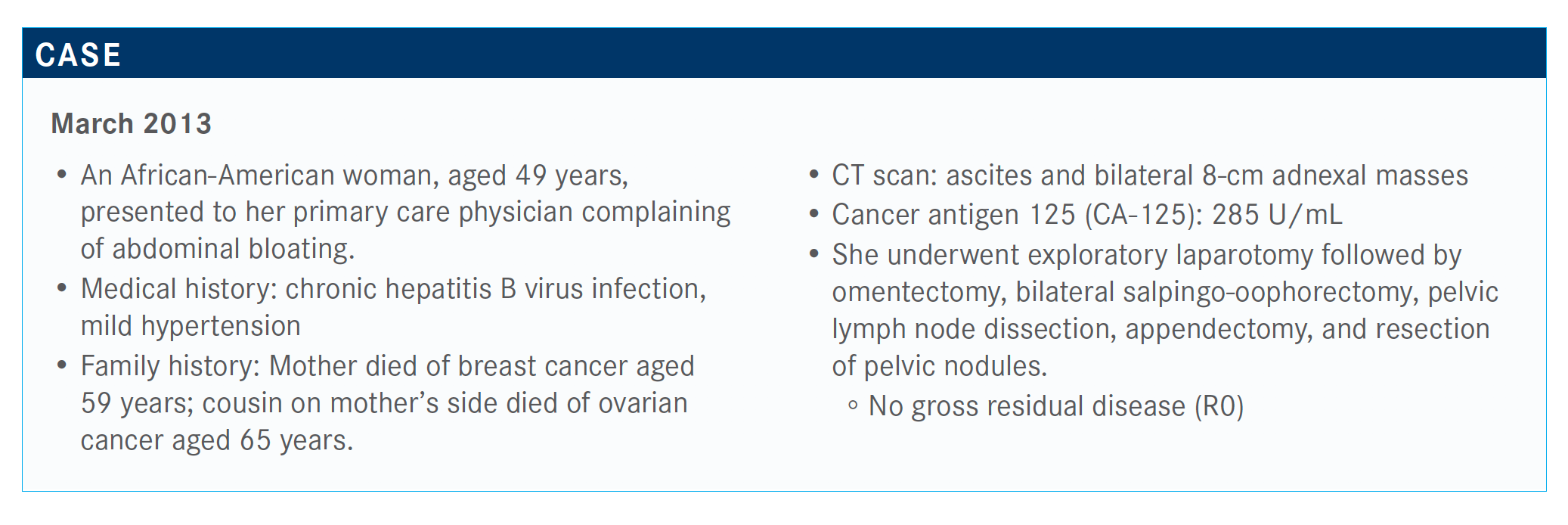
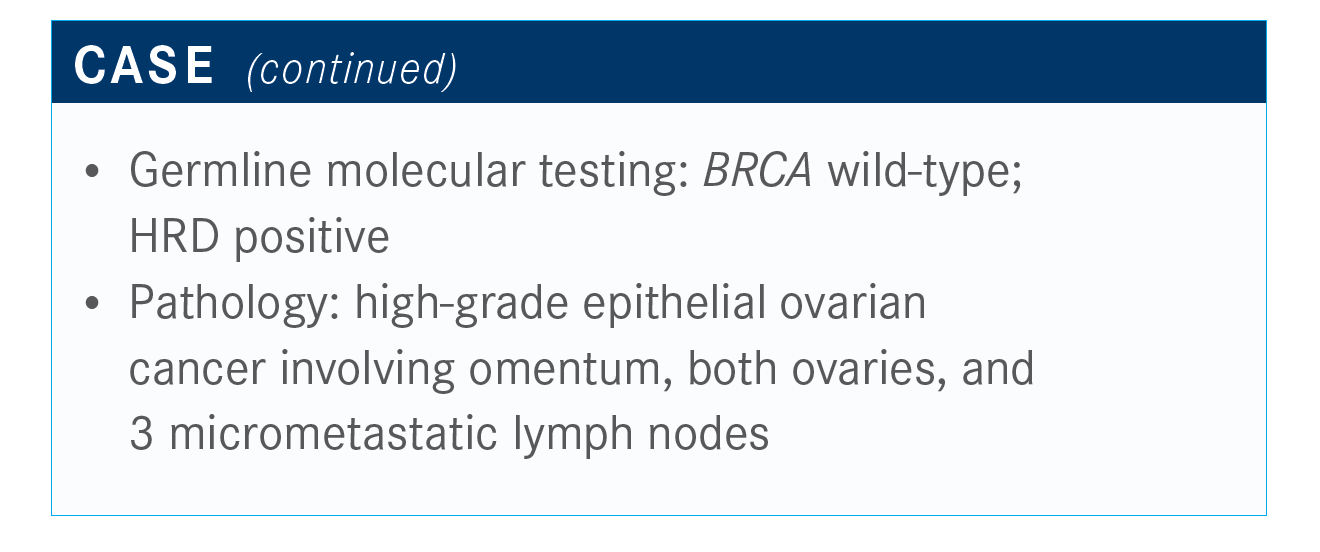
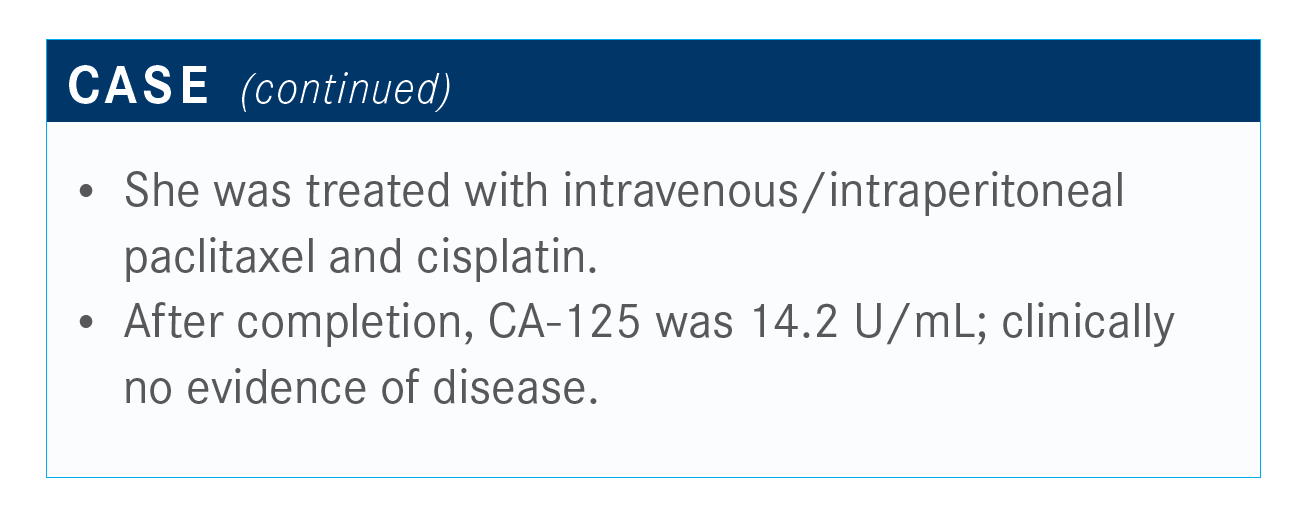
This patient has stage IIIC ovarian cancer and optimal resection. Her tumor is BRCA wild-type but HRD positive.
[Options are] carboplatin and paclitaxel, carboplatin and bevacizumab [Avastin], and then carboplatin and liposomal doxorubicin. Most of us would use carboplatin and liposomal doxorubicin more in a recurrent setting, but that’s acceptable treatment—especially for someone who’s not tolerating a taxane. Most [physicians] would typically start with carboplatin and paclitaxel.
At this point, what would you recommend for this patient?
This patient was treated with paclitaxel and cisplatin, which we don’t do often, but when we do, it’s to treat these patients with low risk and no residual disease. After completion, CA-125 was within the normal limits, and she was clinically without disease.
[The main options are] observation or niraparib.
If you start with niraparib and there are some issues with dosing, would it be a possibility to transition to drugs such as olaparib or rucaparib?
We have no data on that, but there are [physicians] who do that. I think for this patient, who has a germline wild-type mutation, you would start with niraparib. We didn’t get too much granularity on the adverse effect profile.
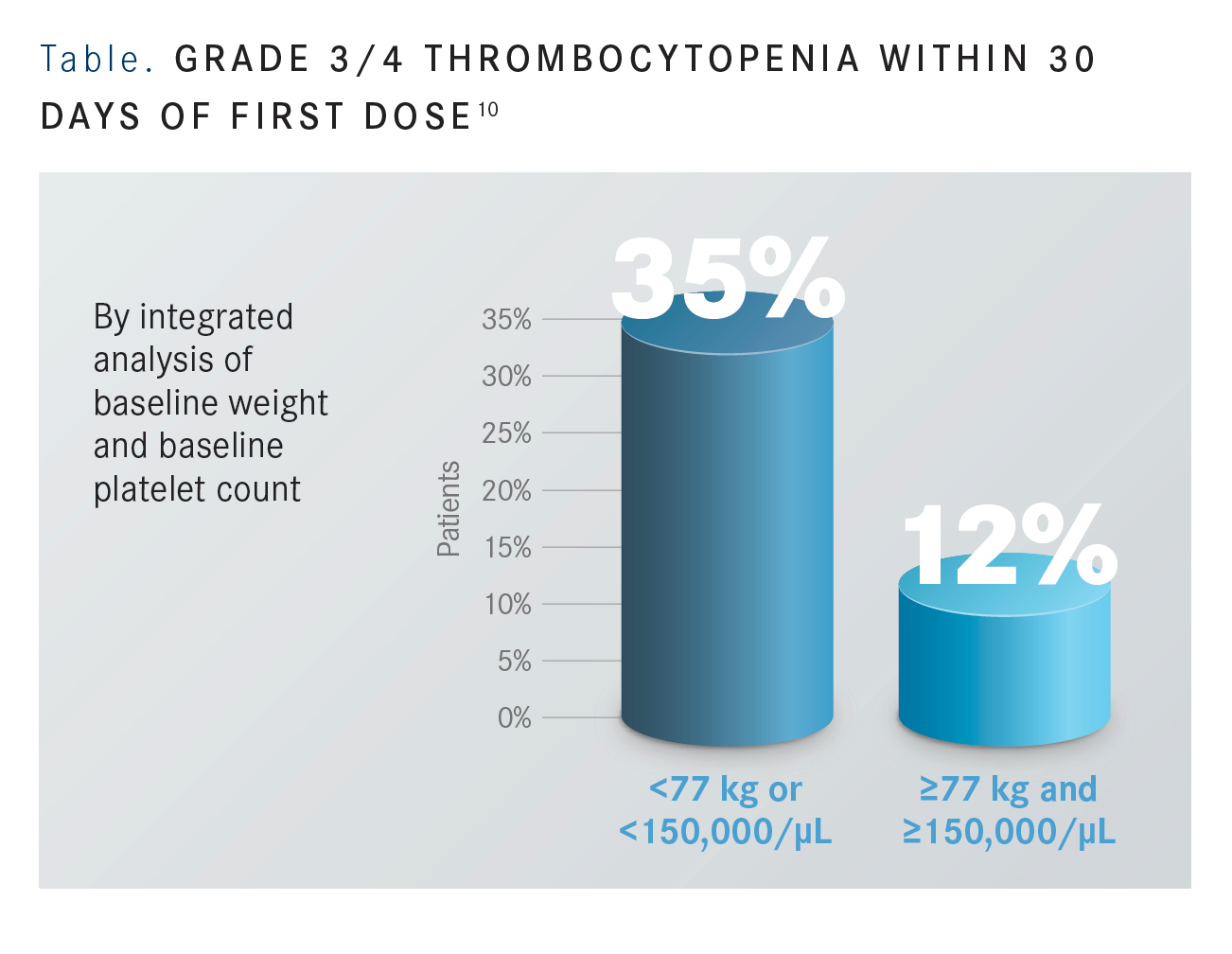
For niraparib, the investigators tested the weights [of the patients] and platelet [counts per] dose. We know that thrombocytopenia is [high] with niraparib at the 300-mg starting dose, but you can decrease that by more than 50% if you drop that starting dose to 200 mg specifically in patients who weigh less than 77 kg or have platelet counts less than 150,000 μL [FIGURE].10
What will be interesting to see, which will be reported soon, are the efficacy data between the 2 doses. The platinum-sensitive niraparib trial, NOVA, reported that most of the patients were dose-reduced. Only 23% of the patients remained on that 300-mg dose because of the thrombocytopenia. They did not show an efficacy difference.9
I would rather switch to another PARP inhibitor than my patient not have the chance to get a PARP. I think they’ve demonstrated sufficient activity, and PARP is probably—as many other drugs we give—the most effective the earlier we give it. While it’s not on label per se, I would rather try another PARP inhibitor than not use PARP at all, and I’ve done that in my practice.
Did you use niraparib as soon as data came out for it, or did you wait for the approval?
I know many people who started using niraparib after the European Society for Medical Oncology Annual Congress 2019, and they were getting it approved. I did not; I didn’t use it until the approval came, and that’s just kind of how I function and practice. If I had a patient who was highly motivated to receive it, I probably would have tried to get it for her, but I did not use it until the approval.
References:
1. FDA approves niraparib for HRD-positive advanced ovarian cancer. FDA. October 23, 2019. Accessed May 21, 2020. www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-niraparib-hrd-positive-advanced-ovarian-cancer
2. myChoice CDx. Myriad. Accessed May 21, 2020. myriad.com/products-services/ precision-medicine/mychoice-cdx/
3. NCCN. Clinical Practice Guidelines in Oncology. Ovarian cancer, version 1.2020. Accessed May 21, 2020. NCCN.org/professionals/physician_gls/pdf/ovarian.pdf
4. González-Martín A, Pothuri B, Vergote I, et al; PRIMA/ENGOT-OV26/GOG-3012 Investigators. Niraparib in patients with newly diagnosed advanced ovarian cancer. N Engl J Med. 2019;381(25):2391-2402. doi:10.1056/NEJMoa1910962
5. Coleman RL, Fleming GF, Brady MF, et al. Veliparib with first-line chemotherapy and as maintenance therapy in ovarian cancer. N Engl J Med. 2019;381(25):2403-2415. doi:10.1056/NEJMoa1909707
6. FoundationOne CDx technical information. Foundation Medicine; 2017. Accessed May 21, 2020. rochefoundationmedicine.com/f1cdxtech
7. Coleman RL, Oza AM, Lorusso D, et al; ARIEL3 Investigators. Rucaparib maintenance treatment for recurrent ovarian carcinoma after response to platinum therapy (ARIEL3): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2 017;390 (10106):1949-1961. Published correction appears in Lancet. 2017;390(10106):1948. doi:10.1016/S0140-6736(17)32702-2
8. Swisher EM, Lin KK, Oza AM, et al. Rucaparib in relapsed, platinum-sensitive high-grade ovarian carcinoma (ARIEL2 Part 1): an international, multicentre, open-label, phase 2 trial. Lancet Oncol. 2017;18(1):75-87. doi:10.1016/S1470-2045(16)30559-9
9. Mirza MR, Monk BJ, Herrstedt J, et al; ENGOT-OV16/NOVA investigators. Niraparib maintenance therapy in platinum-sensitive, recurrent ovarian cancer. N Engl J Med. 2016;375(22):2154-2164. doi:10.1056/NEJMoa1611310
10. Berek JS, Matulonis UA, Peen U, et al. Safety and dose modification for patients receiving niraparib. Ann Oncol. 2018;29(8):1784-1792. Published correction appears in Ann Oncol. 2019;30(5):859. doi:10.1093/annonc/mdy255

Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More