Multikinase Inhibitor Options Flourish for Patients With RET-Mutant Medullary Thyroid Cancer
During a Targeted Oncology Case-Based Peer Perspectives event, Andrew G. Gianoukakis, MD, FACE, discussed the use of multikinase inhibitors for RET-mutated medullary thyroid cancer.
Andrew G. Gianoukakis, MD, FACE

During a Targeted Oncology Case-Based Peer Perspectives event, Andrew G. Gianoukakis, MD, FACE, investigator, The Lundquist Institute, professor of Medicine, David Geffen. School of Medicine at UCLA, Program Director, Endocrinology Fellowship Program, Harbor-UCLA Medical Center, discussed the use of multikinase inhibitors for RET-mutated medullary thyroid cancer.
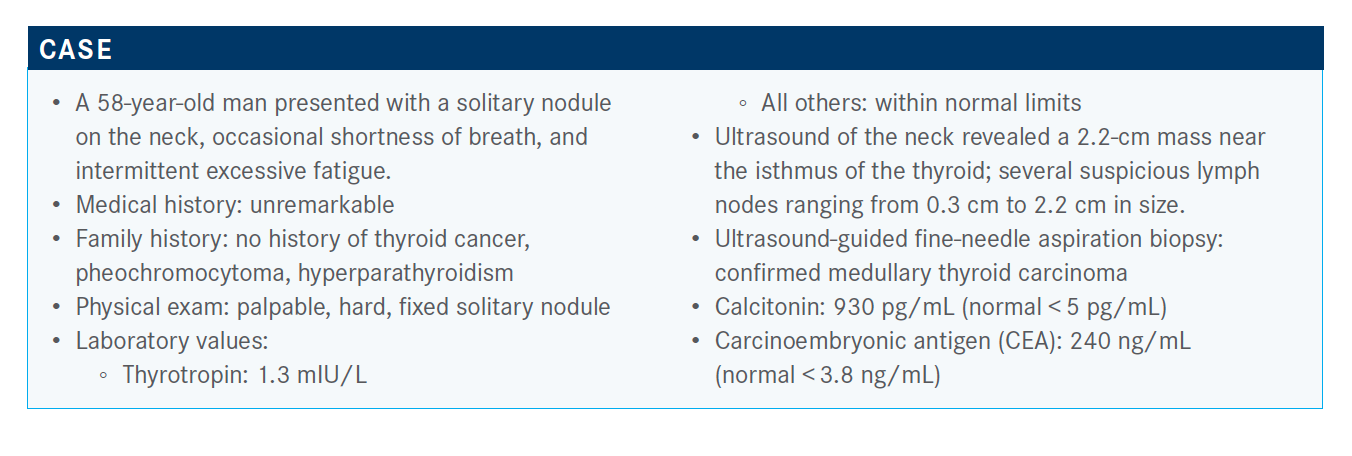
Targeted OncologyTM: As an endocrinologist, how would you interpret this patient’s disease?
GIANOUKAKIS: It’s the endocrinologist who is performing the biopsy and making the original diagnosis and then likely following up. A few rules of thumb: When medullary thyroid cancer presents as a palpable nodule—if it presents as a palpable nodule and that’s when you’re catching it—you’re likely in the order of a 70% to 75% chance of having central neck and lateral neck disease, and about a 10% chance of distant disease.
Looking at the calcitonin levels, a cutoff at presentation of about 500 pg/mL is generally considered a good cutoff to think about metastatic disease. So, if your calcitonin is less than 500 pg/mL versus over 500 pg/mL, [that] less likely suggests metastatic disease, [whereas] over 500 pg/mL suggests metastatic disease; by metastatic, I mean distantly metastatic. Twenty is the cutoff for neck disease. If you diagnose a patient and their level is less than 20 pg/mL, [they are] unlikely to have lymph node disease in the neck. As you progress between 20 pg/mL and 500 pg/mL, you have an increased likelihood of neck disease and then distant disease. So, based on what we have here, a palpable thyroid nodule and a calcitonin level of 930 pg/mL, I suspect that this is likely in the neck and likely distantly metastatic.
If the level is 500 pg/mL, you can stick to focusing on the neck. If it’s close to 500 pg/mL, if it’s over 500 pg/mL, you definitely want to look for distant metastases. You want to be less aggressive in the neck if [there is already metastasis].
You’re less likely [to resect if the calcitonin level is less than 500 pg/mL]. You’re very likely to have neck disease, you’re less likely to have distantly metastatic disease.
What additional testing or scans would you order for this patient?
One thing that’s important is liver metastases. [These] can be a common area for metastasis early in medullary thyroid cancer, and they can escape diagnosis on a regular CT scan. So you either need a triple phase CT, or you need an MRI of the liver, or sometimes direct visualization with a surgical look at the liver, primarily the surface of the liver where you can oftentimes have metastases that are hiding. It’s important to appropriately scan the liver, especially when you’re thinking about distant metastases.
Depending on the level, you can commonly find metastases in bone. So, an MRI of bone or a bone scan are also important tools to consider when you want to [be sure] you’re not missing distant metastases, before going into the neck and being ultra-aggressive with your thyroidectomy and then your lymph node dissection.
A PET scan is not as sensitive, definitely for the bone metastases and I think overall for medullary disease.
How do you determine resectability of the patient’s disease?
At my institution and I think at most centers, the way it works is your endocrinologist does the initial workup and sends the patient to surgery. We have multidisciplinary conferences where we have a discussion, and so the surgeon will have input. But they will lean on our discussion and our recommendation. So, if we feel comfortable that we’re less likely to be dealing with distant disease, they won’t take the patient who we’ve already scanned or evaluated and rescan them.
What is your approach toward genetic testing for a patient with medullary thyroid cancer?
You can start with the genetic screening with your germline mutation analysis, and if you do not detect a germline RET mutation and if there’s no family history, etcetera, you’re less likely to be dealing with [heritable disease]. If you’ve excluded heritable medullary disease, you don’t need to screen for hyperparathyroidism. We all usually screen for pheochromocytomas because genetic testing and complete exclusion of even rare forms of heritable medullary thyroid cancer and RET mutations can be missed there, and you certainly don’t want to miss a pheochromocytoma and [send the patient to] surgery.
[I would] definitely screen with at least plasma metanephrines for pheochromocytomas in the event that you’ve performed your germline mutational testing and excluded a heritable cause for the pheochromocytomas. If you either have a family history or identify a germline mutation, then you also want to exclude hyperparathyroidism. If hyperparathyroidism is occurring, you want to have that taken care of surgically at the same time as you’ll be performing the thyroidectomy. The pheochromocytoma evaluation needs to happen first, and should you identify a pheochromocytoma and that needs to be resected, you would prepare the patient for surgery and have the adrenalectomy performed prior to...parathyroid surgery.
How would you handle this patient knowing his updated genomic testing profile? How do his calcitonin and CEA levels affect his prognosis?
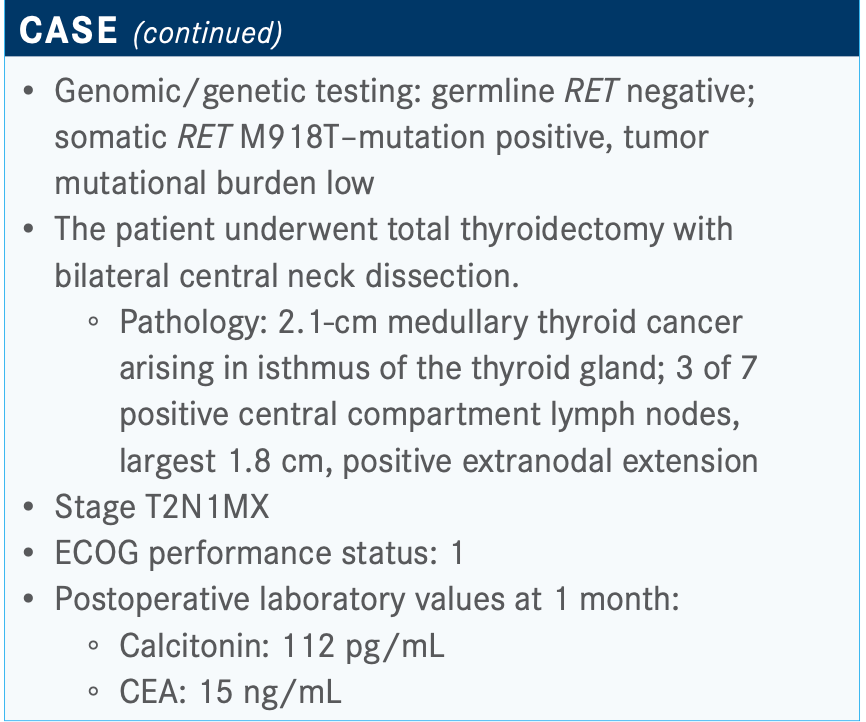
The germline testing was negative. However, a somatic RET M918T mutation with a low tumor burden was noted for the tumor. So we’re not dealing with a heritable syndrome, but there is a RET somatic mutation.
Now, this is someone whom, based on the initial presentation, we should have looked at for distant metastases, and so we’re presuming that we looked distantly and did not identify any disease despite that level of calcitonin. So we were aggressive in the neck. This is what we found in the neck, and this is what was found in the mutational analysis.
About 25% of medullary thyroid cancers are part of a heritable multiple endocrine neoplasia syndrome. The other 75% are negative on germline testing. However, about 50% of that 75% will have a somatic mutation, and the majority of those will be RET M918T mutations. The RET M918T portends a worse or more aggressive prognosis. [Regarding] the calcitonin level of 112 pg/mL postoperatively, it’s a little early; [we should] wait a couple of months more to see how far that will drop. In general, there is a cutoff of about 10 pg/mL to 20 pg/mL; if your calcitonin drops below 10 pg/mL, a tiny fraction of those will come back up. It’s almost considered a cure, whether patients in the low single digits will recur. And then, as that level rises in the follow-up stages, a cutoff of 150 pg/mL is used as the benchmark above which you start to look for anatomic disease.
Eighty percent of the time, CEA and calcitonin will go together, and we’re going to talk about doubling times, and they double similarly and they [match] each other. The other 20% [of the time] they’re discordant. There are tumors that make only CEA and not calcitonin, and sometimes you’ll have tumors as they become more dedifferentiated and aggressive; they’re less likely to make calcitonin and more likely to make CEA. Those are thought to be more aggressive tumors that are dedifferentiating. So they’re both helpful [to know]. They usually go together.
Can you comment on the doubling time of the calcitonin level in this patient?
Calcitonin and CEA doubling time is associated with survival. The cutoffs are 6 months and 24 months; [in other words], a doubling time of less than 6 months versus a doubling time between 6 months and 24 months versus a doubling time over 24 months. The more rapid the doubling time, the worse the 5- and 10-year survival [rates]. Intermediate [rates are] between 6 and 24 months. [There was] slow progression and high survival rates with nearly 100% at 5 years with doubling times over 24 months. Rapid doubling time portends an aggressive course and a poor prognosis, and we’re now 12 months post the initial surgery.
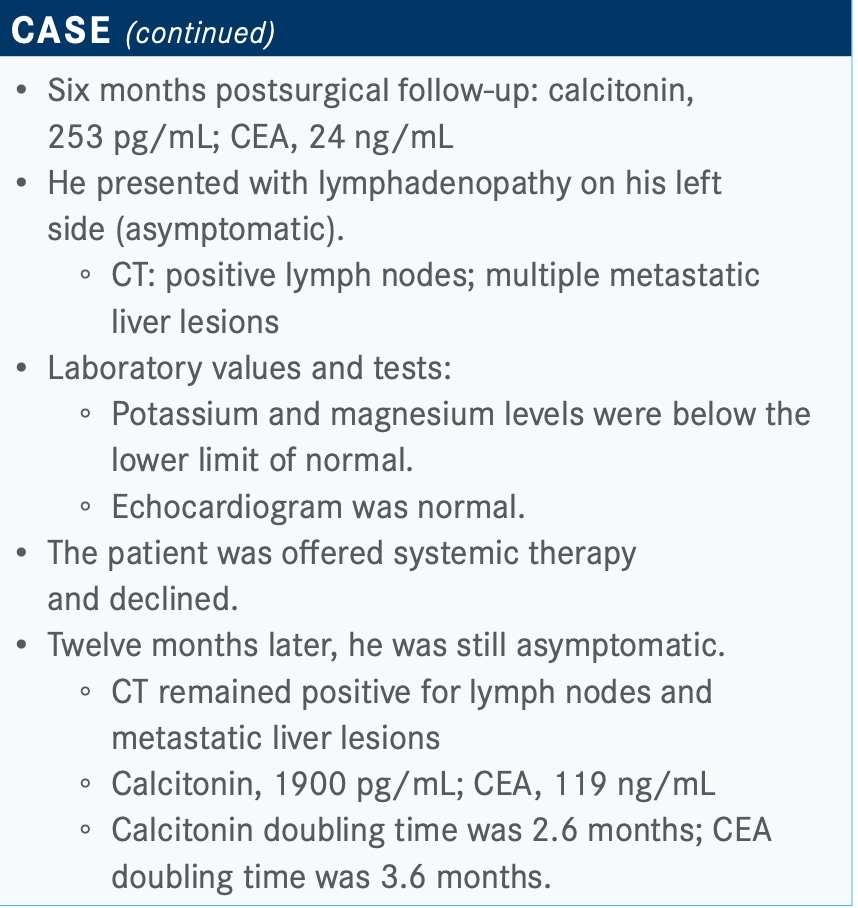
Would you recommend systemic therapy for this patient now or not, and why?
Similar to other solid tumors, the criteria for offering systemic therapy to patients with medullary, or well-differentiated, or anaplastic thyroid cancer are the same. [They’re] based on RECIST progression. Patients have to have measurable disease, progressive disease, or be symptomatic. We do not use a calcitonin level as a reason to treat; it’s a marker to either make us look for disease, as we’ve been discussing, or a prognostic marker via the doubling time calculation. But we won’t make a decision on treating or not treating systemically based on a calcitonin [level].
I’m sure many physicians have patients with calcitonin levels that are in the 3000s and 4000s, who have anatomic disease that’s stable and not progressing, that [they are] watching. So, similar to other solid malignancies, we’re looking for disease progression for symptomatic disease, for symptoms and progression. In well-differentiated thyroid cancer, the third criterion is radioiodine refractoriness, which is not the case here.
We don’t have enough information; we don’t have information on size of lesions, progression of lesions, or change in size of lesions. We just know he has some small lymph node metastases initially. The size isn’t being given to us now, and he has liver metastases that are still there but no mention of anatomic progression. Should the lesions be progressing, should the patient be symptomatic and it be mirroring his calcitonin, I think then we could proceed with therapy. So, for the purposes of this [case], we’ll assume that he’s having progressive or symptomatic disease with a doubling time of less than 6 months.
What are the systemic therapy options for this patient? What do the National Comprehensive Cancer Network (NCCN) guidelines recommend?
Cabozantinib [Cabometyx] in general is considered to be more toxic than vandetanib [Caprelsa]. Vandetanib has QT prolongation, so in someone at risk of arrhythmias or cardiac disease, maybe you would shy away from it and go with the cabozantinib. The cabozantinib also was, in my opinion, a better choice for patients like this one with the RET M918T mutation. There is an overall survival [OS] benefit to cabozantinib in the subgroup with the RET M918T mutation.1 As we’re learning, selpercatinib [Retevmo] and pralsetinib [Gavreto] [have been shown to have] lower toxicities and great efficacy and could be replacing the vandetanib and cabozantinib.
The NCCN guidelines [suggest] disease monitoring, or to consider resection or ablation for asymptomatic disease, basically attempts at local and locoregional therapy.2 [They also suggest] considering systemic therapy [if the disease] is not resectable and progressing by RECIST criteria. It’s a little tricky because the category for symptomatic or progressive [disease also says to use systemic therapy], but they also have it under the asymptomatic category.
Preferred regimens, as we’ve discussed, are vandetanib, cabozantinib, selpercatinib, and now pralsetinib [for both asymptomatic and symptomatic or progressive disease]. Other small molecule kinase inhibitors [are listed for symptomatic or progressive disease]. You could have lenvatinib [Lenvima] on this list, although it’s not on there. [For local symptoms, there’s] external beam radiation therapy/intensity-modulated radiation therapy. Bisphosphonate therapy [is] for bone metastases.
Please describe the trial data behind the use of vandetanib.
The ZETA trial [NCT00410761] of vandetanib was a phase 2 trial.3 Vandetanib showed a median progression-free survival [PFS] advantage of about 30 months versus about 19 months between the treatment arm and placebo arm [HR, 0.46; 95% CI, 0.31-0.69; P < .001]. It did allow crossover once [a patient was] progressing on vandetanib. However, inclusion criteria did not require progression in the year prior to enrollment on trial. There was a benefit to the vandetanib therapy and there was also crossover that didn’t allow OS evaluation down the line.
The ZETA trial looked at a breakdown by mutation, positive versus negative. There was a benefit if you were mutation positive and a benefit if you were RET M918T positive.
Both [vandetanib and cabozantinib] have a good amount of toxicities...diarrhea, rash, nausea, hypertension, [which are] common to all the multikinase inhibitors. What is different and important is the EKG QT prolongation that occurs in about 8% of the [patients taking] vandetanib at a grade 3 level and may be a reason to choose cabozantinib over vandetanib.
What was the efficacy of cabozantinib for these patients?
In the EXAM trial [NCT00704730] for cabozantinib, there was a PFS of 11.2 months versus 4 months, much lower numbers in both categories [compared with vandetanib] because patients had to have progression in the year prior to therapy [HR, 0.28; 95% CI, 0.19-0.40; P < .0001]. Crossover was not allowed in this trial, and so if patients progressed on placebo, they were not allowed to cross over. Ultimately, investigators were able to show and publish, in a subsequent trial, an OS benefit of cabozantinib versus placebo. But, otherwise, with regard to its primary end point of PFS, it showed a benefit in this study, and led to the approval of cabozantinib as a second treatment for medullary thyroid cancer.
[Regarding] the benefit of treatment in RET-positive disease, when you have RET positivity and particularly RET M918T positivity, ...[there were] OS and PFS benefits across the board, except in RET-negative disease.
Cabozantinib, in my opinion, is quite toxic, more toxic than vandetanib. So in patients who may be elderly or frail, if all else was equal, I would go with vandetanib over cabozantinib. But, in terms of potency, [cabozantinib] does appear to be more potent. An additional adverse effect that’s more common in cabozantinib versus vandetanib is the hand-foot syndrome.
What was the result for patients previously treated with vandetanib or cabozantinib?
Efficacy of the LIBRETTO-001 trial [NCT03157128] was broken down via RET-mutant medullary thyroid cancer previously treated versus not previously treated, and previously treated RET fusion–positive differentiated thyroid cancer versus not previously treated.... Objective response [rates were] 69% and 73% for the previously treated versus not previously treated [medullary thyroid cancer groups]. It was 79% and 100% when you look at the RET fusion-positive thyroid cancer previously treated versus not [groups].
There were a good number of complete remissions in addition to a very high number of partial remissions. Duration of response was not [reached] in all the categories.
Focusing on the RET-mutated medullary thyroid cancer not previously treated with vandetanib or cabozantinib, the majority of patients had a partial or complete remission. A percentage had stable disease, and only 1 patient noted progression but did not achieve RECIST 1.1 progression.
Treatment-related adverse events of any grade was 94%. However, grade 4 was only 2%, and grade 3 only 28%. The adverse effects focused on what we know to be common: hyper- tension, diarrhea, fatigue. Some small increase in liver function tests were noted but [there was] much lower toxicity [and it was]much more manageable, much more tolerable than [with other] multikinase inhibitors.
Which therapies are being looked at now for this patient population?
Currently, there’s an ongoing trial of selpercatinib versus cabozantinib or vandetanib [LIBRETTO-531; NCT04211337]. Patients are randomized to receive either selpercatinib or physician choice of cabozantinib or vandetanib. The primary outcome is treatment failure–free survival and then yourtypical secondary outcomes. This trial is available in multiple sites across the county [and is] close to completing enrollment. It has been hampered by both COVID-19 [coronavirus disease 2019] and the approval of selpercatinib. [Because of] the toxicity of cabozantinib and vandetanib and the great preference due to the efficacy and low adverse effect profile for selpercatinib, it’s been more challenging to enroll for this trial. It will be a direct comparison for both toxicity and efficacy between the previous first-line therapies and selpercatinib.
REFERENCES:
1. Schlumberger M, Elisei R, Müller S, et al. Overall survival analysis of EXAM, a phase III trial of cabozantinib in patients with radiographically progressive medullary thyroid carcinoma. Ann Oncol. 2017;28(11):2813-2819. doi:10.1093/annonc/mdx479
2. NCCN. Clinical Practice Guidelines in Oncology. Thyroid carcinoma, version 2.2020. Accessed January 6, 2021. https://bit.ly/2TAGexh
3. Wells SA Jr, Robinson BG, Gagel RF, et al. Vandetanib in patients with locally advanced or metastatic medullary thyroid cancer: a randomized, double-blind phase III trial. J Clin Oncol. 2012;30(2):134-141. doi:10.1200/JCO.2011.35.5040
4. Wirth LJ, Sherman E, Robinson B, et al. Efficacy of selpercatinib in RET-altered thyroid Cancers. N Engl J Med. 2020;383(9):825-835. doi:10.1056/ NEJMoa2005651

Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More