Matasar Considers Treatment Options in B-Cell Lymphoma
Matt Matasar, MD, discusses treatment options in B-cell lymphomas.
Matt Matasar, MD
During a Targeted OncologyTM Case-Based Roundtable, Matt Matasar, MD, discusses treatment options in B-cell lymphomas.
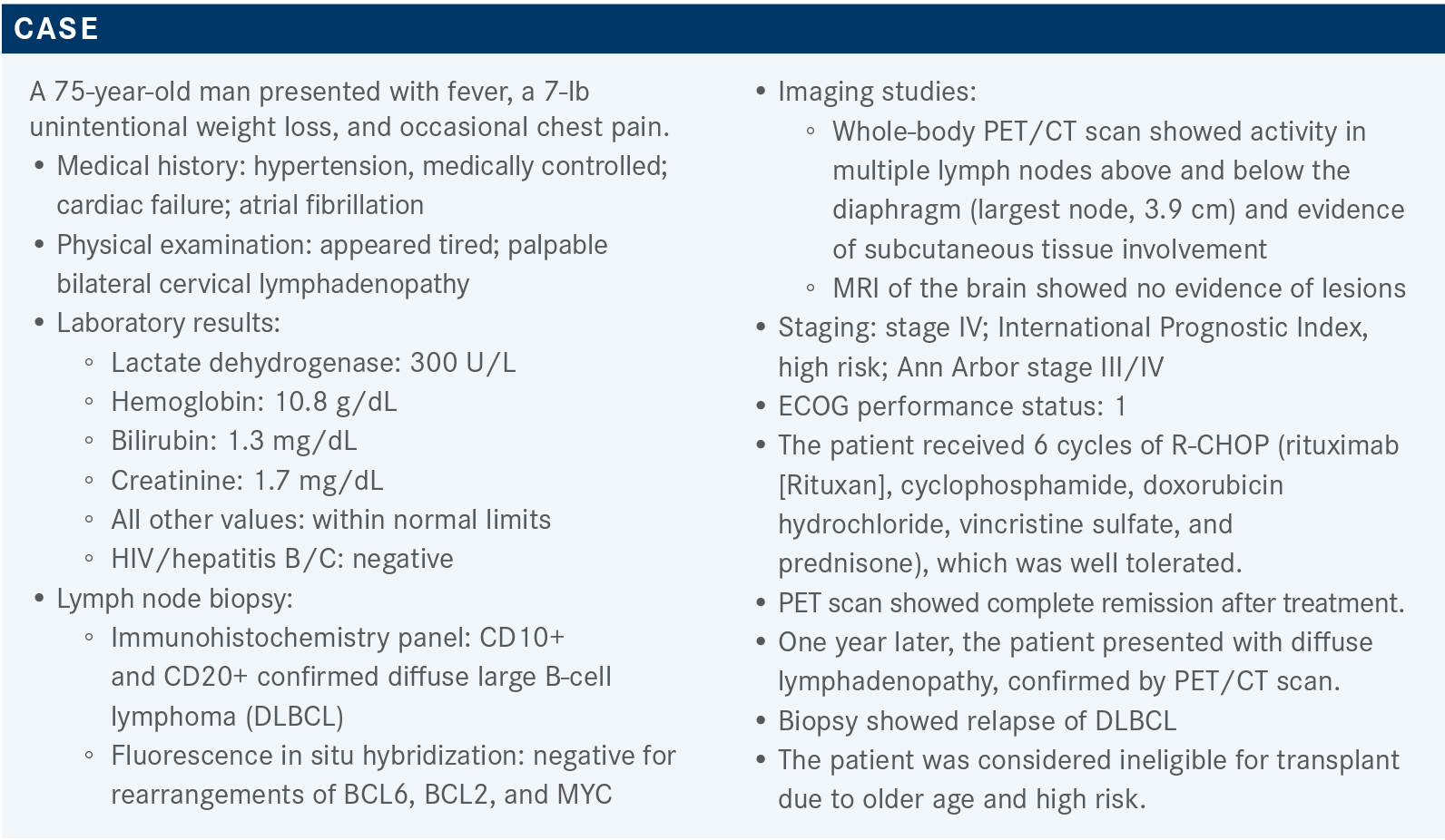
Case overview
Targeted OncologyTM: What are the treatment options in the second-line setting?
MATASAR: The NCCN [National Comprehensive Cancer Network] criteria recommend 2 preferred regimens, the first being the R-GemOx [gemcitabine, oxaliplatin (Eloxatin), plus or minus rituximab (Rituxan)] that our patient here received, and the second being the combination of BR/pola [polatuzumab (Polivy), plus or minus bendamustine, plus or minus rituximab].¹ There are a number of other alternative regimens NCCN recommends, most of which are cytotoxic-based with the exception of tafasitamab [Monjuvi] and lenalidomide [Revlimid], which are listed as the last of the “other recs.” Under the category of “useful in certain circumstances,” there are things like brentuximab vedotin [Adcetris] for CD30+ disease; BR without polatuzumab; and then ibrutinib [Imbruvica] or R2, the lenalidomide plus or minus rituximab program for non-GCB [germinal center B-cell] large cell lymphoma.
Which of these regimens are FDA approved?
The only regimens that are specifically FDA approved are the BR/pola regimen and the tafasitamab plus lenalidomide regimen.1-3 The BR/pola regimen’s FDA approval is specifically for third-line [therapy] and beyond, but given the data from the clinical trial [NCT02257567] leading to its approval and subsequent updates on those data, it’s NCCN-listed as second-line [therapy] and beyond.1,4 The tafasitamab plus lenalidomide program is simply approved for relapsed/refractory large cell lymphoma, regardless of line of therapy, as long as [patients are] transplant ineligible.1,5
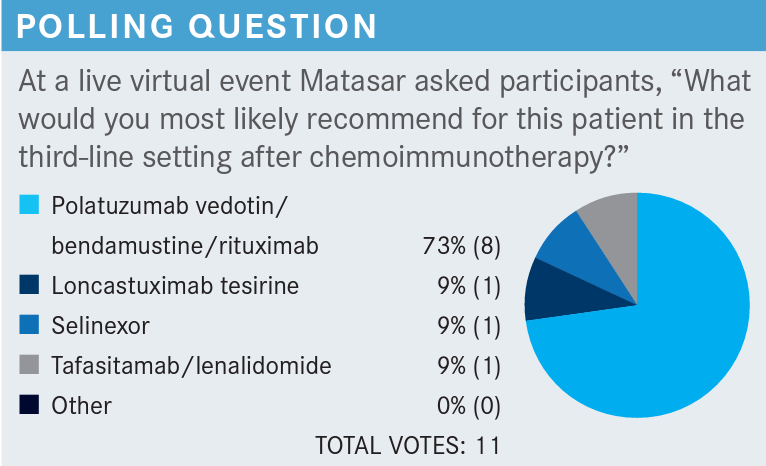
What factors influence decision-making in the thirdline treatment setting?
In terms of how you follow patients after they’ve gotten their treatment for relapsed/refractory disease, if they’ve either only had a PR [partial response], or relapsed subsequently, or progress on their second-line treatment, then you’re thinking about third-line therapy.1 Third line in NCCN is either CAR [chimeric antigen receptor] T-cell therapy, which has FDA approvals for third line and beyond, or you pick some other second-line program. Or you can give palliative radiotherapy, or just palliative care with considerations for an allogeneic transplant in patients who respond, although that’s a little bit controversial, truthfully. When you look at the third-line subsequent therapy with CAR T cell, there are 3 that are approved: axi-cel [axicabtagene ciloleucel (Yescarta)], tisagen [tisagenlecleucel (Kymriah)], and now liso-cel [lisocabtagene maraleucel (Breyanzi)].1,6-8 But NCCN recommends 2 additional drugs: the first is loncastuximab tesirine [Zynlonta], and selinexor [Xpovio], which is approved as third-line [therapy] or beyond.1,2,9
Challenges with tafasitamab or loncastuximab include that these are both drugs that target CD19. Loncastuximab is a CD19-targeted antibody-drug conjugate and tafasitamab is a naked anti-CD19 antibody.3,9 There’s a lot of uncertainty in the medical and lymphoma communities about how to sequence CD19-directed therapies. Is it OK to give people loncastuximab or tafasitamab if you’re thinking about a subsequent therapy with a CD19-directed CAR T cell, or are you potentially cutting off your nose to spite your face?
Please discuss the data that led to the approval of axi-cel, tisagen, and liso-cel.
Axi-cel we think of as maybe the most active, with an ORR [overall response rate] north of 80%, and a CR [complete response] rate approaching 60%.10 Tisagen was a little bit milder, with an ORR of 50%.11 Liso-cel had an ORR of 70%, although some of the mature overall survival [OS] data are around liso-cel, which is helpful.12,13
Toxicity-wise, they do differ, and they seem to track along with the activity. So, [the general theme] the stronger the toxicity has been the general theme. Axi-cel is a little bit stronger than liso-cel, maybe, but definitely more toxic.10,14 Tisagen has much lower rates of neurotoxicity, and so it is more like liso-cel than axi-cel.10-12,14 The CRS [(cytokine release syndrome) was determined by a] different scale with tisagen, [they used the University of Pennsylvania grading scale which yielded a score of 23% of patients having a grade 3 or 4 CRS]; but a lot of that would be classified as grade 1-2 by the Lee criteria that the axi-cel and liso-cel data use.10-12,14,15
Please discuss some of these data that supports the use of newer therapies in this patient population.
The most recent approval was for loncastuximab tesirine, which was approved [in April 2021 for] the treatment of relapsed/refractory large cell lymphoma.16 Loncastuximab’s design is an antibody-drug conjugate, like polatuzumab, in terms of its design, but very different. It targets CD19, as do the CD19-targeting CAR T-cell therapies; and the payload is not MMAE [monomethyl auristatin E], as it is in brentuximab or polatuzumab, but teserine, which is a cytotoxin.9,17 It’s a PBD [pyrrolobenzodiazepine] payload and it causes cross-links. So, this is a direct cytotoxic agent.
The data behind loncastuximab’s approval come from the LOTIS-2 study [NCT03589469], which was a single arm phase 2 study of loncastuximab in the treatment of relapsed/refractory large cell lymphoma.18 It was designed for third line and beyond. They had to be proven to be CD19 positive if they’d had prior CD19-directed therapy. Bulky diseases were excluded, and that’s based on the phase 1 data, showing that it doesn’t have activity at an adequate level in bulky disease. It did allow for transformed low-grade lymphoma, and high-grade lymphoma, but Burkitt’s lymphoma was excluded; that’s a very different animal along with active central nervous system disease, as well as the other factors.
The way you give loncastuximab [is to administer] a loading dose of 150 µg/kg for the first 2 cycles and after that you decrease to 75 µg/kg.⁹ It’s given as a brief 30-minute infusion every 3 weeks for up to a year of treatment, after which you stop. The ORR was the study’s primary end point and there were a host of secondary clinical end points.
In terms of the patients who were treated with loncastuximab in LOTIS-2, the majority were regular large cell lymphoma, although there was a small percentage of patients who had high-grade lymphoma or primary mediastinal lymphoma.18 A small percentage of patients had a double hit [10%], whereas most patients had advanced-stage disease. The median number of prior lines of therapy was 3, so this is median fourth-line therapy in this study. A minority of patients, but a substantial minority, were primarily refractory to their original anthracycline-based therapy and the majority were refractory to the most recent line of therapy.
What were the efficacy results of LOTIS-2?
In terms of the activity, we see an ORR with loncastuximab monotherapy of 48% [95% CI, 39.9%-56.7%], and a CRR of 24% [95% CI, 17.4%-31.9%].18 Most patients responded early; there were very few late responders. The median time to response was 40 days, and the median number of cycles administered was 4, but some patients did go on to get the full 18 as specified by protocol. When you look at the LOTIS-2 data by subgroup, in that small group of patients who did have double or triple hit, there were responders even in high-grade lymphoma. There were responders in both de novo and transformed disease. There were responders even among the relatively few patients who had a prior transplant.
Even in the small number of patients who had prior CAR T that still had CD19 expression, there was response in that small group. So, the take-home from the subgroup analysis with loncastuximab is that there’s not a prespecified group of patients in whom the drug lacks activity, and that’s important to remember. Although cell of origin may influence decision-making here; for the subset of patients that we had cell of origin, which was not all patients, the activity seemed comparable for GCB and non-GCB, and that makes sense. This is just a cytotoxin; there’s no reason to believe that the B-cell [treatment] differs between GCB and non-CGB.
The duration of response was reasonable, particularly in the CR patients; for those who did achieve a CR, the median duration of response over a year is favorable.18 PRs were relatively few and they tended to drop off quickly, as you’d expect with relapsed aggressive lymphoma.
The median PFS [progression-free survival] was 5 months and the median OS approached 10 months. These are not great survival rates, but for median fourth-line therapy, where the median survival expectancy without active treatment would be measured in weeks and not months, it’s worthwhile contextualizing these results. In terms of subsequent treatment, there were patients who went on to receive CD19-directed CAR T-cell therapy, and those patients did have an adequate response to subsequent CAR T-cell therapy. We don’t know how many patients lose CD19 when they are refractory to loncas-tuximab; that’s an area of ongoing clinical investigation.
In terms of toxicity, loncastuximab does have some well-characterized toxicity at this point, including hematologic toxicity—particularly thrombocytopenia, although not overwhelmingly so.18 One adverse effect [AE] of loncastuximab that’s unusual, and we think that’s related to the PBD payload because we’ve seen it in other PBD-delivering drugs, is a fluid accumulation issue. This can be peripheral edema and it can also be pleural effusions. This is a clinical pearl: If you ever want to prescribe loncastuximab for patients, be thoughtful about evaluating patients’ weight, look for peripheral edema, listen for effusions, and at the onset of fluid accumulation, start spironolactone [Aldactone] early during treatment.9
What are some tips for treatment with loncastuximab?
As I said, you start with a loading dose for 2 cycles and then you continue it for up to a year at a lower dose. Premedicating with steroids is important; you give them ahead of time.9 If you can’t do that, then definitely at least give dexamethasone premedication, and that’s continued through the course of treatment. A little bit of guidance here, particularly regarding the fluids as we’ve just said: If you start getting into trouble despite spironolactone, hold the loncastuximab, dial the dose down if you need to. The same goes for cytopenias, particularly thrombocytopenia. You can also use growth factor support along with loncastuximab if you need to, such as pegfilgrastim.
There’s a lot of work ongoing with developing loncastuximab further. LOTIS-2 was a monotherapy study, and usually we don’t stop at monotherapy. Right now, they’re working on developing LOTIS-5 [NCT04384484], a randomized trial of R-GemOx as an erstwhile standard of care vs loncastuximab plus rituximab.19
What data supports tafasitamab’s approval?
That data that supported tafasitamab’s approval come from the L-MIND study [NCT02399085], it's important to understand the pros and cons of that study.20 This was treatment for second line and beyond large cell lymphoma transplant-ineligible patients with large cell lymphoma, that excluded patients who had primary refractory disease.
That differs from the loncastuximab study, as well as from PBR. [The regimen was] tafasitamab, they get loaded the first month, for 4 weeks in a row, in combination with lenalidomide, and then patients go on to every other week treatment intravenously. After those first 12 cycles, lenalidomide is dropped, and patients stay on tafasitamab maintenance therapy until progression or intolerance.
It was an older patient population, median number of prior lines of therapy was 2, so a little bit less heavily pretreated number of patients.21 Early relapse was only 20%, those with primary refractory disease were excluded. There was a little bit of an amendment process that allowed some patients on who progressed between 3 and 6 months after first-line therapy. So, less heavily pretreated, and less aggressive subset of patients. They all still did have relapsed/refractory large cell lymphoma.
The outcomes show there was good activity in this admittedly select group of patients, with 43% patients achieving a CR, an additional 18% of patients achieving a PR, for an ORR of 60%.22 For those, a median duration of response of almost 2 years and it was quite active in this selected patient population.
At the initial time of reporting, the median PFS was 12 months and OS had not yet been met. This was favorable, compared to what else was available at the time in this patient setting. These data have been updated recently by Dr [Gilles] Salles with a median PFS now estimated at 16 months, and median OS of almost 3 years, an extraordinarily favorable OS.22
What is the toxicity profile of tafasitamab?
In terms of the tolerability, tafasitamab itself seems to add very little toxicity on top of lenalidomide.3,20 We are all very well acquainted with the toxicity of lenalidomide monotherapy, including some cytopenias. In addition to tafasitamab maintenance, lenalidomide seems to have very little additional toxicity. In terms of nonhematological toxicity, there was maybe a little bit of additional myelosuppression from tafasitamab and most of this we believe is attributable to lenalidomide.
Only 12% of patients came off [of therapy] due to AEs and there were 13% of patients who came off due to death; however, in the opinion of the investigators, none of those were attributable specifically to therapy, and instead were due to progression of disease.
What other studies impact treatment decisions for clinicians?
The GO29365 study [NCT02257567] study was designed to look at both large cell lymphoma and follicular lymphoma, but we’re focusing on the large cell lymphoma part of that study.22 It was a small, randomized component after a safety run-in of BR alone vs BR/pola. This was for second line and beyond, transplant-ineligible patients. Primary refractory patients were allowed, however. The median number of prior lines of therapy was 2. The duration of response of the last treatment was less than 12 months, which was most patients, suggesting these were patients who were relatively highly refractory. A substantial fraction of patients had received a prior stem cell transplant, as well.
In terms of the response rates, BR/pola was significantly better than BR alone, with an ORR of 45% compared with only 17% for BR alone.21 The median PFS was 10 months for the BR/pola combination compared with only 4 months for BR alone. Median OS with BR/pola was 12 months compared with 5 months with BR alone.
You may say, “we have a median OS of 12 months for BR/pola, we had a median OS of over 2 years for tafasitamab plus lenalidomide,” and I would caution against that type of cross-trial comparison, given the exclusion of refractory patients. There will be updated data for the BR/pola combination, looking at the patients who would have been eligible for L-MIND, excluding the refractory patients, trying to draw some more cross-trial comparisons that should hopefully shed more light on the activity of BR/pola vs tafasitamab plus lenalidomide in that lower risk patient population.
In terms of AEs, we are all very well familiar with the AEs caused by BR in our patient population, myelosuppression in particular.22 Polatuzumab is an antibody-drug conjugate delivering MMAE, which is an antitubule agent that has wellcharacterized neuropathy. The neuropathy in this study was relatively modest and largely reversible, and polatuzumab does seem to add a little bit on top of the myelosuppression from BR alone.
REFERENCES:
1. NCCN. Clinical Practice Guidelines in Oncology. B-cell lymphomas, version 5.2021. Accessed August 24, 2021. https://bit.ly/3geoS5N
2. Xpovio. Prescribing information. Karyopharm Therapeutics Inc; 2021. Accessed August 24, 2021. https://www.karyopharm.com/wp-content/uploads/2019/07/NDA-212306-SN-0071-Prescribing-Information-01July2019.pdf
3. Monjuvi. Prescribing information. MorphoSys US Inc; 2021. Accessed August 24, 2021. https://www.monjuvi.com/pi/monjuvi-pi.pdf
4. FDA approves polatuzumab vedotin-piiq for diffuse large B-cell lymphoma. FDA. News release. FDA Drug Approvals and Databases. June 10, 2019. Accessed August 24, 2021. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-polatuzumab-vedotin-piiq-diffuse-large-b-cell-lymphoma
5. FDA grants accelerated approval to tafasitamab-cxix for diffuse large B-cell lymphoma. FDA Drug Approvals and Databases. August 3, 2020. Accessed August 24, 2021. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-grants-accelerated-approval-tafasitamab-cxix-diffuse-large-b-cell-lymphoma
6. Yescarta. Prescribing information. Kite Pharma, Inc; 2021. Accessed August 24, 2021. https://www.gilead.com/-/media/files/pdfs/medicines/oncology/yescarta/yescarta-pi.pdf
7. Kymriah. Prescribing information. Novartis Pharmaceuticals Corp; 2021. Accessed August 24, 2021. https://www.novartis.us/sites/www.novartis.us/files/kymriah.pdf
8. Breyanzi. Prescribing information. Bristol Myers Squibb; 2021. Accessed August 24, 2021. https://packageinserts.bms.com/pi/pi_breyanzi.pdf
9. Zynlonta. Prescribing information. ADC Therapeutics; 2021. Accessed August 24, 2021. https://www.adctherapeutics.com/wp-content/uploads/2021/04/pi.pdf
10. Locke FL, Ghobadi A, Jacobson CA, et al. Long-term safety and activity of axicabtagene ciloleucel in refractory large B-cell lymphoma [ZUMA-1]: a single-arm, multicentre, phase 1-2 trial. Lancet Oncol. 2019;20[1]:31-42. Accessed August 27, 2021. doi:10.1016/S1470-2045[18]30864-7
11. Schuster SJ, Bishop MR, Tam CS, et al. Tisagenlecleucel in Adult Relapsed or Refractory Diffuse Large B-Cell Lymphoma. N Engl J Med. 2019;380[1]:45-56. Accessed August 27, 2021. doi:10.1056/NEJMoa1804980
12. Abramson JS, Palomba ML, Gordon LI, et al. Lisocabtagene maraleucel for patients with relapsed or refractory large B-cell lymphomas [TRANSCEND NHL 001]: a multicentre seamless design study. Lancet. 2020;396[10254]:839-852. Accessed August 27, 2021. doi:10.1016/S0140-6736[20]31366-0
13. FDA approves lisocabtagene maraleucel for relapsed or refractory large B-cell lymphoma. FDA Drug Approvals and Databases. February 5, 2021. Accessed August 27, 2021. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-lisocabtagene-maraleucel-relapsed-or-refractory-large-b-cell-lymphoma
14. Neelapu SS, Locke FL, Bartlett NL, et al. Axicabtagene Ciloleucel CAR T-Cell Therapy in Refractory Large B-Cell Lymphoma. N Engl J Med. 2017;377[26]:2531-2544. Accessed August 27, 2021. doi:10.1056/NEJMoa1707447
15. Bachanova V, Westin J, Tam C et al. Correlative analyses of cytokine release syndrome and neurological events in tisagenlecleucel-treated relapsed/refractory diffuse large b-cell lymphoma patients. Hemat Oncol. 2019; 37[S20]:308-310. Accessed August 27, 2021. https://doi.org/10.1002/hon.118_2630
16. FDA grants accelerated approval to loncastuximab tesirine-lpyl for large B-cell lymphoma. FDA Drug Approvals and Databases. April 23, 2021. Accessed August 27, 2021. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-grants-accelerated-approval-loncastuximab-tesirine-lpyl-large-b-cell-lymphoma
17. Zammarchi F, Corbett S, Adams L, et al. ADCT-402, a PBD dimer-containing antibody drug conjugate targeting CD19-expressing malignancies. Blood. 2018;131[10]:1094-1105. Accessed August 27, 2021. doi:10.1182/blood-2017-10-813493
18. Caimi PF, Ai W, Alderuccio JP, et al. Loncastuximab tesirine in relapsed or refractory diffuse large B-cell lymphoma [LOTIS-2]: a multicentre, open-label, single-arm, phase 2 trial. Lancet Oncol. 2021;22[6]:790-800. doi:10.1016/S1470-2045[21]00139-X
19. Study to Evaluate Loncastuximab Tesirine With Rituximab Vs Immunochemotherapy in Participants With Relapsed or Refractory Diffuse Large B-Cell Lymphoma [LOTIS 5]. ClinicalTrials.gov. Identifier: NCT04384484. Updated August 23, 2021. Accessed August 27, 2021. https://clinicaltrials.gov/ct2/show/record/NCT04384484?term=NCT04384484&draw=2&rank=1
20. Salles G, Duell J, González Barca E, et al. Tafasitamab plus lenalidomide in relapsed or refractory diffuse large B-cell lymphoma [L-MIND]: a multicentre, prospective, single-arm, phase 2 study. Lancet Oncol. 2020;21[7]:978-988. Accessed August 27, 2021. doi:10.1016/S1470-2045[20]30225-4
21. Salles G, Duell J, González Barca E, et al. Long-term outcomes from the phase II L-MIND study of tafasitamab [MOR208] plus lenalidomide in patients with relapsed or refractory diffuse large B-cell lymphoma. Abstract presented at: The 25th European Hematology Association Annual Congress; June 11-21, 2020; Virtual. Accessed August 27, 2021. https://library.ehaweb.org/eha/2020/eha25th/293691/gilles.salles.long-term.outcomes.from.the.phase.ii.l-mind.study.of.tafasitamab.html
22. Zinzani PL, Rodgers T, Marino D, et al. RE-MIND: Comparing tafasitamab + lenalidomide [L-MIND] with a real‑world lenalidomide monotherapy cohort in relapsed or refractory diffuse large B-cell lymphoma. Clin Cancer Res. [online ahead of print] Accessed August 27, 2021. doi:10.1158/1078-0432.CCR-21-1471
23. Sehn LH, Herrera AF, Flowers CR, et al. Polatuzumab Vedotin in Relapsed or Refractory Diffuse Large B-Cell Lymphoma. J Clin Oncol. 2020;38[2]:155-165. Accessed August 27, 2021. doi:10.1200/JCO.19.00172

Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More
Examining the Non-Hodgkin Lymphoma Treatment Paradigm
July 15th 2022In season 3, episode 6 of Targeted Talks, Yazan Samhouri, MD, discusses the exciting new agents for the treatment of non-Hodgkin lymphoma, the clinical trials that support their use, and hopes for the future of treatment.
Listen