Heymach Discusses MET Exon 14 Skipping Mutations in NSCLC
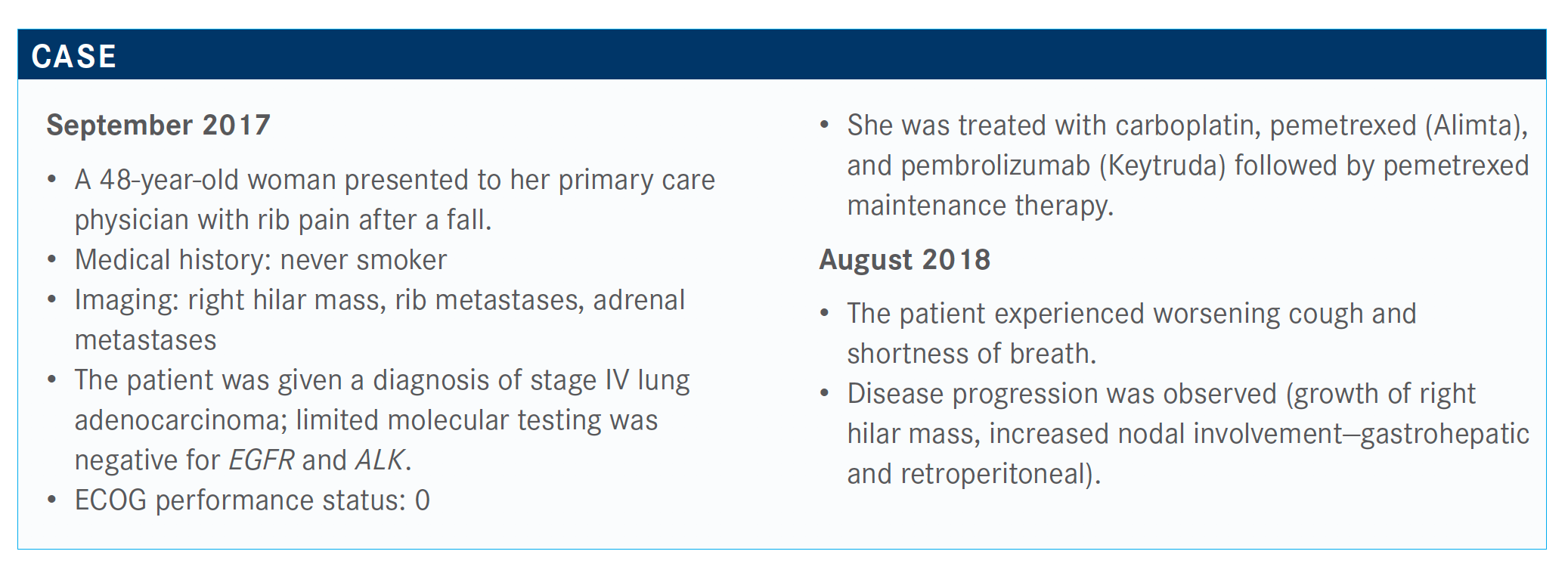
During a Targeted Oncology Case Based Peer Perspective event, John V. Heymach, MD, PhD, discussed the testing methods for non–small cell lung cancer with MET exon 14 skipping mutations. The discussion was based on the case of a 48-year-old woman.
John V. Heymach, MD, PhD

During a Targeted Oncology Case Based Peer Perspective event, John V. Heymach, MD, PhD, chair, Department of Thoracic/Head and Neck Medical Oncology, Division of Cancer Medicine, at The University of Texas MD Anderson Cancer Center in Houston, TX, discussed the testing methods for non–small cell lung cancer (NSCLC) with MET exon 14 skipping mutations. The discussion was based on the case of a 48-year-old woman.
Targeted Oncology™: What do you think of the answers to this poll? Do you think physicians should treat with a chemoimmunotherapy or a targeted agent in this setting?
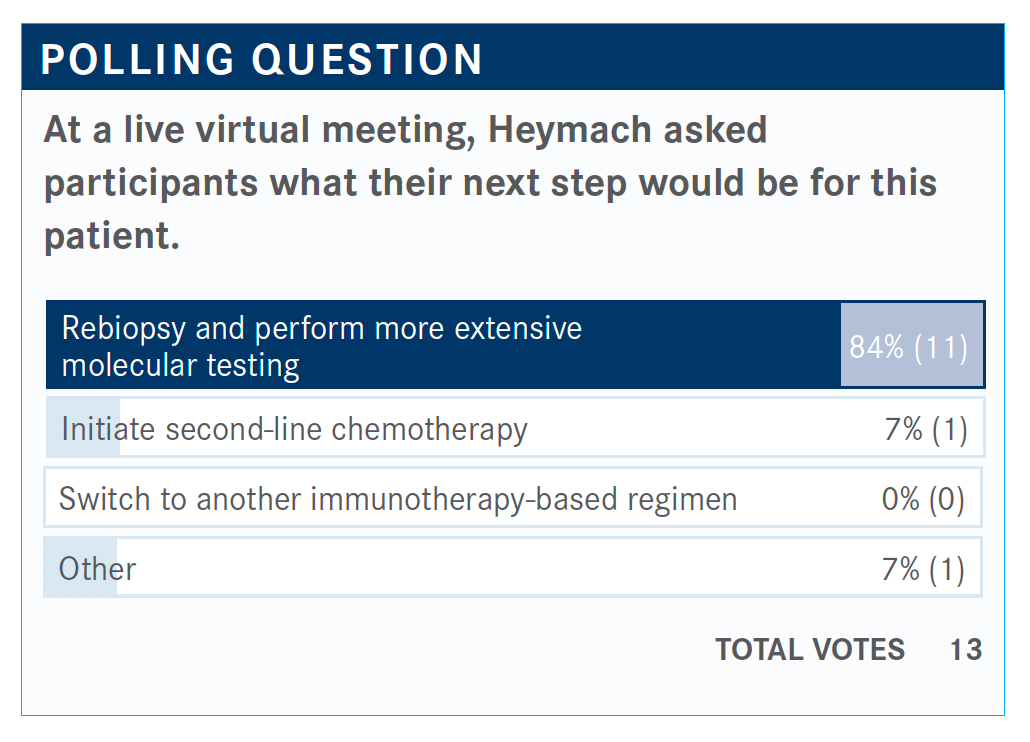
HEYMACH: It looks as if we have a good agreement here. A majority would rebiopsy and do more extensive molecular testing. It’s possible to go back to the original biopsy and try to test it as well.
In general, for the patients with driver [mutations], I still go with targeted agents first. If you take, for example, patients with BRAF, [their] response rates are a bit lower. Progression-free survival [PFS] is shorter if you treat with dabrafenib [Tafinlar] and trametinib [Mekinist], but I still use the targeted agent first when we discover [the tumor] because even if the response rate is in the 50% [range], [targeted agents have fewer adverse effects] than chemotherapy and [give] the chance to avoid chemotherapy or chemoimmunotherapy. In the majority of cases, I will still [choose] the targeted agent first.
When we get to some of the drugs that have lower response rates like ones for EGFR exon 20 or HER2, where these new drugs are going to have closer to 30% response rates, that’s where it’s more of a toss-up. In general, I’ll go with a targeted agent first regardless of what the alteration is.
Ponatinib [Iclusig] works well; we have TAK-788, which looks good; none of them are FDA approved yet. For HER2, there’s DS-8201a, the new antibody-drug conjugate. I’m hoping in the next year or 2, we will have these drugs approved and then we’ll have those choices, but in those cases, the early data for the tyrosine kinase inhibitors [show] response rates are more in that 30% neighborhood, not in the 70% response range. That’s where it’s more of a trade-off.
Do you normally test for MET exon 14 skipping mutations? Which testing panel do you use?
Because this MET exon 14 skipping mutation is brand-new and we just got the drug approved [recently], some of the tests don’t have this alteration. This is important. When you send a test, you can’t [do only] EGFR and ALK testing. We have EGFR, ALK, BRAF, ROS1, NTRK fusion, and now MET exon 14 alterations and RET fusions. That’s 7 alterations that you need to test for. Really, it tells us we need to do next-generation sequencing.
Some of the panels don’t cover MET exon 14 skipping mutations, so whichever panel you’re using, please check to make sure that it’s covering it. At MD Anderson Cancer Center, we were using the Oncomine panel. The Oncomine version 2 didn’t cover MET exon 14. It’s just the version 3, which we got recently, that does. We were missing all these patients for a long time.
There are a couple of things that make MET exon 14 mutations different. Unlike the driver mutations like ALK and EGFR, where the median age is younger, here the median age is older, commonly 70-year-olds. It’s often in smokers, so this isn’t just young, nonsmoking Asian patients that we think about. This is older individuals; it’s often smokers. The other thing is these are patients with adenocarcinoma, but sometimes they have sarcomatoid, and sometimes they have squamous disease. [There was a] big analysis in patients with squamous disease, and often they had these MET exon 14 alterations.
Now, if you run the Guardant360 [panel], it does cover it. I believe Caris Life Sciences does, and I know FoundationOne does. This is brand-new, and I think everybody needs to look out for this. It’s fairly common; it’s just about as common as ALK. It’s often in patients with squamous disease. It’s often in the sarcomatoid subtype as well. MET amplification by contrast doesn’t seem to be a driver in the same way. If you get a patient with MET amplification, it may be associated with resistance like EGFR resistance, but it’s not a driver when it’s first showing up. MET exon 14 skipping mutation is a driver with great responses.
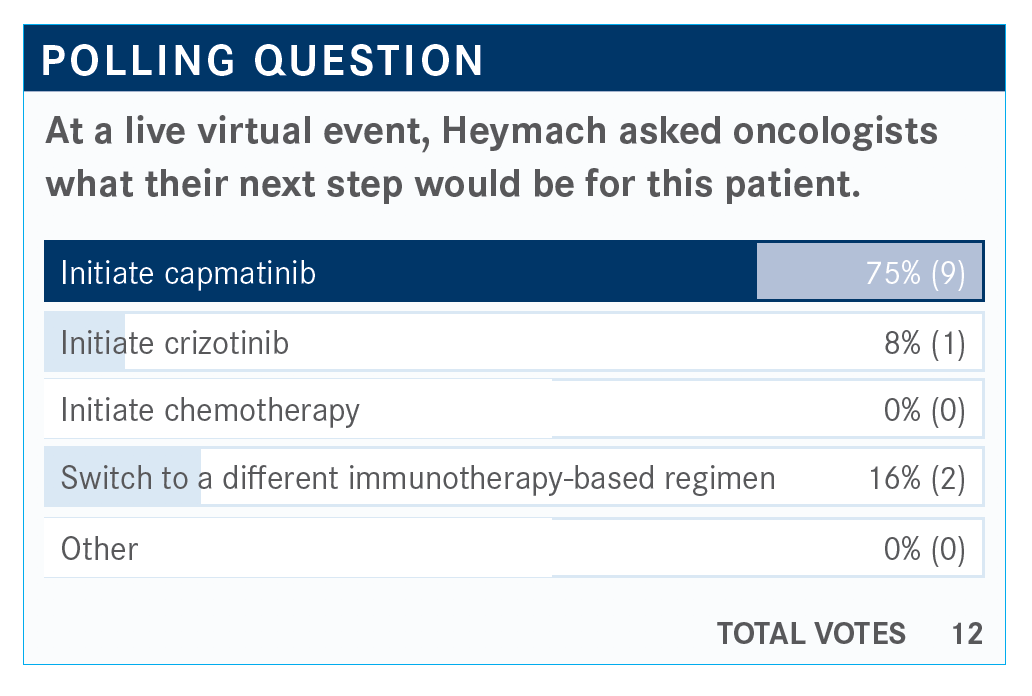
What do you think of the poll results? How does the patient’s mutation affect their treatment?
Capmatinib [Tabrecta] was just approved for MET exon 14 skipping mutations. Sixteen percent would go to a different immunotherapy-based regimen. Then 8% went with crizotinib [Xalkori]. Crizotinib has some data behind it.
The data for crizotinib are from the PROFILE 1001 trial [NCT00585195] in patients with MET exon 14, and the drug was certainly active.1 The response rate was 35%. Median PFS was 7.3 months, and the median duration of response was 9.1 months. For anyone who said crizotinib, it is an active drug in this setting, and most of these were refractory patients. It’s been my experience that you get decent responses for a decent period.
For crizotinib, [common treatment-related adverse events were] edema at 51% and visual disorders [at 45%], and I’ve had a couple of patients where this has really been disturbing; it usually gets better over time. There’s also some nausea, diarrhea, [and vomiting], so I think crizotinib is tolerable but not that easy. Most patients have some significant adverse effects from this. Thirty-eight percent had a dose reduction.
The FDA approved capmatinib in May [2020], and it’s approved only for MET exon 14 skipping mutations. It’s not approved for MET amplification right now. This is based on the GEOMETRY study [NCT02414139].2
How do capmatinib and crizotinib fit into the National Comprehensive Cancer Network (NCCN) guidelines? What are the data behind them?
The NCCN guidelines for first-line therapy recommend capmatinib as the preferred option.3 Crizotinib is useful, or you can give systemic therapy. Then, for patients who have MET exon 14 after first-line therapy was initiated, they recommend completing systemic therapy, or you could interrupt it and move to capmatinib but at progression. [Or] you could go to capmatinib afterward. The NCCN does support using capmatinib as first-line therapy if you discovered [the mutation], and the approval is for either first-line or later lines for capmatinib.
The GEOMETRY study [of capmatinib had] multiple cohorts.4 Cohort 4 was [patients who were] pretreated in the second or third line. In the refractory second- and third-line cohort, there was a 40.6% overall response rate. The disease control rate was 78.3%. Median duration of response was 9.7 months, and median PFS was 5.4 months in the refractory cohort. This was a bit better than crizotinib.
The naïve population had a response rate of 68% by blinded review. The median PFS was 9.7 months, and duration of response was 11.4 months. This was a small cohort, but it looks good in the first-line setting. These data are why I would start with capmatinib for a first-line patient. I wouldn’t hold it for the second line because if you compare this with first-line chemotherapy and pembrolizumab…this looks better. That group doesn’t respond great to immunotherapy.
What was the safety profile of capmatinib in the GEOMETRY trial?
Pneumonitis [was observed] in 4.5% [of patients], and in 2.4% [of patients,] it led to discontinuation. [It took] about a month and a half [for patients to have onset of pneumonitis]. There was grade 3/4 peripheral edema in 7% of patients and nausea in 2%. Overall, you get the picture that this was better tolerated than crizotinib, with some patients having grade 3/4 toxicity. Discontinuation because of an adverse event was 11% overall.
References:
1. Drilon A, Clark JW, Weiss J, et al. Antitumor activity of crizotinib in lung cancers harboring a MET exon 14 alteration. Nat Med. 2020;26(1):47-51. doi:10.1038/s41591-019-0716-8
2. FDA grants accelerated approval to capmatinib for metastatic non-small cell lung cancer. FDA. May 6, 2020. Accessed September 12, 2020. https://bit.ly/35CGfb4
3. NCCN. Clinical Practice Guidelines in Oncology. Non–small cell lung cancer, version 8.2020. Accessed September 12, 2020. https://bit.ly/2RnzyBD
4. Wolf J, Seto T, Han JY, et al. Capmatinib (INC280) in METex14-mutated advanced non-small cell lung cancer (NSCLC): efficacy data from the phase II GEOMETRY mono-1 study. J Clin Oncol. 2019;37(suppl 15):9004. doi:10.1200/JCO.2019.37.15_suppl.9004

Osimertinib Plus Savolitnib May Address MET Resistance in EGFR+, MET-Amplified NSCLC
January 28th 2021Patients with EGFR-mutant, MET-amplified or -overexpressed non–small cell lung cancer and MET resistance treated with osimertinib in combination with savolitinib may be able to overcome resistance, according to final analysis findings.
Read More
Identification of key oncogenic drivers and the development of targeted therapies with clinical activity in patients harboring actionable mutations have revolutionized the treatment paradigm in non–small cell lung cancer, redirecting attention toward advances in biomarker testing methodologies.
Read More
Safety, Pharmacokinetic Findings Are Revealed for MET Inhibitor TPX-0022
December 1st 2020The MET inhibitor TPX-0022 was safe and well tolerated in a phase 1 dose-escalation study, SHIELD-1, involving patients with advanced solid tumors harboring MET alterations, according to results presented during the 32nd Molecular Targets and Cancer Therapeutics Symposium.
Read More
Crizotinib Activity in MET-Altered Non-Small Cell Lung Cancer Undetermined
October 29th 2020While the remarkable activity of crizotinib as treatment of patients with ROS1 fusion-positive advanced non–small cell lung cancer was confirmed in a recent systemic review and meta-analysis, the efficacy of this small molecular inhibitor remains unknown in patients with MET-altered disease.
Read More