Gupta Makes a Case for PD-L1 Inhibitors in Bladder Cancer
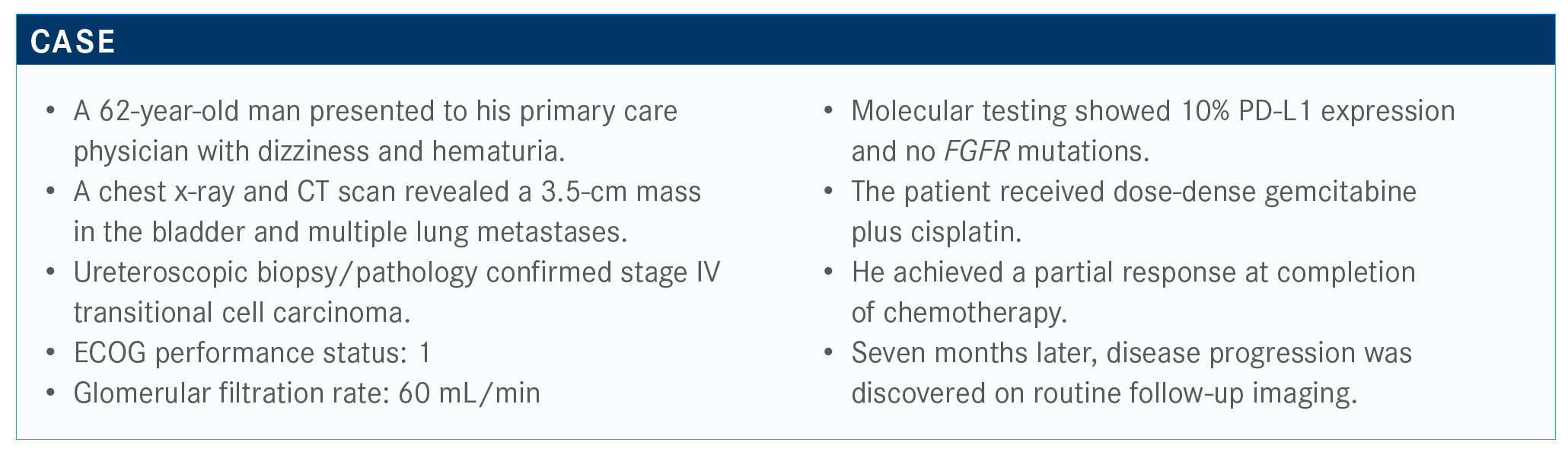
During a Targeted Oncology Case Based Peer Perspective event, Shilpa Gupta, MD, discussed the case of a 62-year-old man with bladder cancer.
Shilpa Gupta, MD

During a Targeted Oncology Case Based Peer Perspective event, Shilpa Gupta, MD, leader, Bladder Cancer Program, Taussig Cancer Institute at the Cleveland Clinic in Cleveland, OH, discussed the case of a 62-year-old man with bladder cancer.
Targeted Oncology™: Would you repeat PD-L1 expression testing on this patient if initially we knew that the patient had PD-L1 expression and was FGFR negative?
GUPTA: This is an interesting question. We talk about this all the time—that we should have serial tissue testing, which a lot of clinical trials mandate. But, in the real world, is it feasible to do, or is it [even] necessary? If the patient has disease progression, do you do a repeat biopsy and test it?
I would. That’s ideal to be able to do because we know that the PD-L1 biomarker may be a dynamic biomarker and may change over time. But if it’s not feasible to do it, then you would use the original information.
Because this patient already received platinum therapy and progressed, how would it affect your treatment if the tumor was PD-L1 negative on the repeat biopsy?
We have multiple immunotherapy agents available. Based on the KEYNOTE-045 [NCT02256436] data for patients who get chemotherapy upfront and progress, pembrolizumab [Keytruda] is the one with phase 3 evidence that it’s better than salvage chemotherapy, so we don’t need PD-L1 expression for that.1 I would offer [this] patient pembrolizumab. If we don’t have an original biopsy, then it’s reasonable to do next-generation sequencing to look for FGFR3 alterations for additional treatment options. But, other than that, if we already know it was negative, that’s what the original study also used. We are not repeating the metastatic site biopsies outside a clinical trial protocol if it’s not affecting our decision-making.
The FGFR3 status was looked at in the primary tumors in a study, and we would like to know how the metastatic sites are behaving. For that purpose, doing a liquid biopsy is feasible if the [tumor] biopsy is not feasible. But for PD-L1 expression, it doesn’t matter if it’s positive or negative for disease progression, and even for avelumab [Bavencio] maintenance it doesn’t matter.
I think the use of PD-L1 to guide treatment may not be that relevant moving forward unless it’s that first-line patient where the patient doesn’t want chemotherapy or is not fit for chemotherapy— even carboplatin—even then the use of immunotherapy is approved. I’m not using PD-L1 to guide first-line therapy decisions unless a patient refuses, even though they are eligible for chemotherapy.
What therapies are available for this patient?
[Pembrolizumab] is the only agent [that] showed superiority over chemotherapy in a phase 3 randomized trial. Even though [avelumab, durvalumab (Imfinzi), and nivolumab (Opdivo)] are approved based on single-arm studies, none of them [has] the phase 3 data. Atezolizumab [Tecentriq] was the only [other] one that was studied in phase 3, and it was not found to be statistically significantly better, but regardless it is approved. Our practice also uses pembrolizumab based on the level 1 evidence. But it’s not wrong to use any other data or any other agent.
Please describe the data from trials in this setting.
The phase 3 data [for] the atezolizumab showed similar OS [overall survival] benefit compared with salvage chemotherapy, but it was not statistically significant over chemotherapy, which was even better than what we see traditionally.2
If we want to follow the level 1 evidence and the NCCN [National Comprehensive Cancer Network] guidelines, pembrolizumab is the drug of choice for these patients.3 The KEYNOTE-045 study [NCT02256436] where pembrolizumab was used as second-line therapy [showed the] OS was significantly better than salvage chemotherapy.1 And, for patients who had a positive PD-L1 score, the results were better and the hazard ratio was lower [at 0.89; 95% CI, 0.66-1.20]. Across the board, pembrolizumab was better than chemotherapy regardless of PD-L1 status.
Interestingly and surprisingly, atezolizumab was not better than chemotherapy—not statistically significant, anyway.2 The other surprising thing was that even the patients with PD-L1 high expression did not have better OS than the chemotherapy group. This was a big contrast compared [with] the pembrolizumab trial, and that’s why this is a level 2 evidence on the NCCN, and pembrolizumab is level 1.3
How do other data compare with what is seen with pembrolizumab and atezolizumab?
Avelumab, durvalumab, and nivolumab all showed good responses compared with historical controls, regardless of PD-L1 status.4-6 Responses were better in high–PD-L1 expressers.
Avelumab was already approved for platinum-refractory patients, based on [the JAVELIN Solid Tumor] study [NCT01772004]. Now avelumab is the only drug with the phase 3 evidence to be used in maintenance therapy [based on JAVELIN Bladder 100 (NCT02603432)].7 None of these other agents [is] approved in that setting. That is the key difference.
According to the NCCN guidelines for locally advanced or metastatic disease, post platinum therapy, we should try to encourage clinical trials when recommended. But the preferred regimen is pembrolizumab, based on the KEYNOTE-045 data. Alternative preferred regimens can be any of these other immunotherapies [such as] atezolizumab, nivolumab, durvalumab, and avelumab. Erdafitinib [Balversa] is for FGFR3-positive patients.
If patients can’t get immunotherapy, then we use any salvage therapy such as paclitaxel, docetaxel, gemcitabine, [etc].
If a patient has started any immunotherapy and is deriving benefit, then it doesn’t matter whether it’s atezolizumab, nivolumab, or durvalumab. But if we had to choose between these drugs and follow the phase 3 data, [then] pembrolizumab [is suggested]. I think the ease of dosing every 6 weeks is quite attractive with that therapy. But if a patient is already on nivolumab and responding, we don’t want to switch. All these drugs showed similar activity, and it was surprising why atezolizumab did not pan out; I think it was just some study design logistics more than the drug itself.
What drugs do you consider in the third line and beyond for these patients?
The indication of enfortumab vedotin [Padcev], which is an antibody-drug conjugate, is for anybody who has received both prior platinum therapy and immunotherapy. The key thing to note is that platinum therapy does not need to be in the metastatic setting. If a patient [received] neoadjuvant cisplatin, then had cystectomy, then recurred and [received] immunotherapy, they can get enfortumab. The label is just that it has to be prior platinum and immunotherapy, no matter what setting. That does not require any biomarker testing, and it’s an effective drug, with over 40% responses in heavily pretreated patients.
I have used it in a couple of patients. I know with all these trials patients are always excluded, but we have not had any unique issues using it for patients on hemodialysis. Try to use it the day after their dialysis and go from there if there [are] no other options. You have to do something for them.
How do the NCCN guidelines recommend handling immune checkpoint inhibitor–related toxicities?
For grade 1 pneumonitis, we can just hold immunotherapy, reassess in [the] short term, and see how the patient is doing and decide about resuming.3 In grade 2, you can hold immunotherapy and [go for] pulmonary consultation. If needed, you can admit the patients. It all depends…on how they get better with or without steroids. We treat them, and if they keep getting worse, we treat them as grade 3 or 4. Patients with grade 3 and 4 don’t usually get rechallenged unless it’s necessary. [For] severe pneumonitis, [it is suggested to] permanently discontinue immunotherapy—with exceptions—and consider adding other immunosuppressive agents as needed.
I think it’s becoming more of a multidisciplinary approach with all these immune-related adverse events [AEs]. It’s always a multiconsult approach. At our institution, we also have immunotherapy-related AE tumor boards where all the specialties are well engaged and provide their input. It’s a lot of help that we need from our gastrointestinal doctors, pulmonologists, and neurologists for different AEs.
References:
1. Bellmunt J, de Wit R, Vaughn DJ, et al. Pembrolizumab as second-line therapy for advanced urothelial carcinoma. N Engl J Med. 2017;376(11):1015-1026. doi:10.1056/NEJMoa1613683
2. Powles T, Durán I, van der Heijden MS, et al. Atezolizumab versus chemotherapy in patients with platinum-treated locally advanced or metastatic urothelial carcinoma (IMvigor211): a multicentre, open-label, phase 3 randomised controlled trial. Lancet. 2018;391(10122):748-757. doi:10.1016/S0140-6736(17)33297-X
3. NCCN. Clinical Practice Guidelines in Oncology. Bladder cancer, version 6.2020. Accessed September 9, 2020. https://bit.ly/3lold5s
4. Patel MR, Ellerton J, Infante JR, et al. Avelumab in metastatic urothelial carcinoma after platinum failure (JAVELIN Solid Tumor): pooled results from two expansion cohorts of an open-label, phase 1 trial. Lancet Oncol. 2018;19(1):51-64. doi:10.1016/S1470-2045(17)30900-2
5. Powles T, O’Donnell PH, Massard C, et al. Efficacy and safety of durvalumab in locally advanced or metastatic urothelial carcinoma: updated results from a phase 1/2 open-label study. JAMA Oncol. 2017;3(9):e172411. doi:10.1001/jamaoncol.2017.2411
6. Galsky MD, Saci A, Szabo PM, et al. Nivolumab in patients with advanced platinum-resistant urothelial carcinoma: efficacy, safety, and biomarker analyses with extended follow-up from CheckMate 275. Clin Cancer Res. Published online July 24, 2020. doi:10.1158/1078-0432.CCR-19-4162
7. Powles T, Park SH, Voog E, et al. Maintenance avelumab + best supportive care (BSC) versus BSC alone after platinum-based first-line (1L) chemotherapy in advanced urothelial carcinoma (UC): JAVELIN Bladder 100 phase III interim analysis. J Clin Oncol. 2020;38(suppl 18):LBA1. doi:10.1200/JCO.2020.38.18_suppl.LBA1

Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More