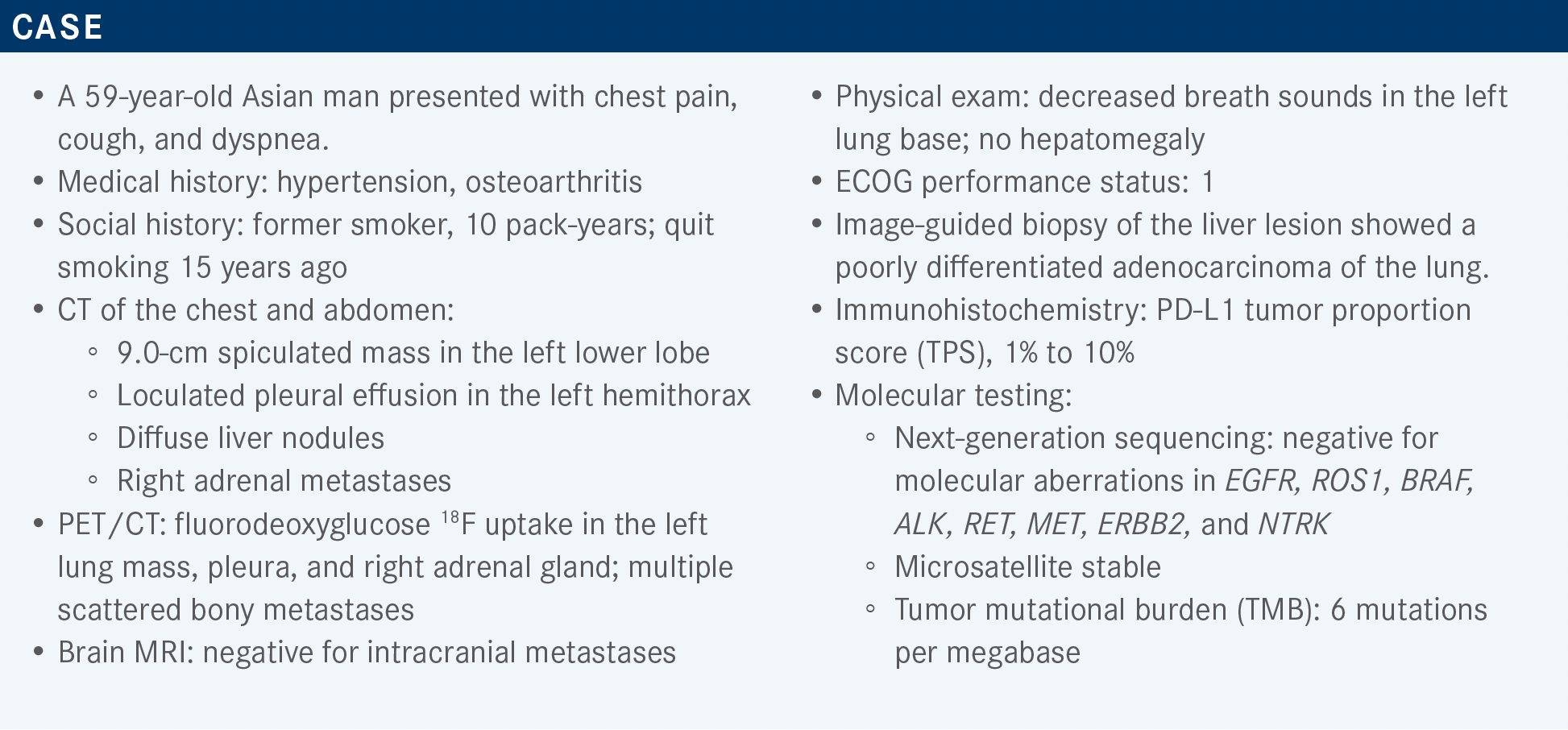
Hegde Considers Combination Regimens for NSCLC With PD-L1 Expression 1% or Higher
During a Targeted Oncology live event, Aparna Hegde, MD, discussed the results of the KEYNOTE-189 study of pemetrexed and pembrolizumab, the KEYNOTE-042 study of single-agent pembrolizumab, and the CheckMate 227 study of nivolumab and ipilimumab in patients with non–small cell lung cancer.
Aparna Hegde, MD
Assistant Professor of Medicine, Hematology & Oncology
Associate Scientist
O’Neal Comprehensive Cancer Center
University of Alabama at Birmingham
Birmingham, AL

Targeted OncologyTM: What therapy does the National Comprehensive Care Network (NCCN) recommend for patients with non–small cell lung cancer (NSCLC) with PD-L1 expression in the range of 1% to 49%?
HEGDE: The preferred regimen as per the NCCN guidelines is the combination of pemetrexed [Alimta] and pembrolizumab [Keytruda] plus either carboplatin or cisplatin. Other recommended regimens are the combination of carboplatin, paclitaxel, bevacizumab [Avastin], and atezolizumab [Tecentriq]; carboplatin, albumin-bound paclitaxel [Abraxane], and atezolizumab; and nivolumab [Opdivo], ipilimumab [Yervoy], and pemetrexed plus either carboplatin or cisplatin. Listed as “useful in certain circumstances” is nivolumab plus ipilimumab and single-agent pembrolizumab. Single-agent pembrolizumab is a category 2B recommendation; all the others are category 1 recommendations.1
What data support the use of NCCN’s preferred regimen of pemetrexed/pembrolizumab plus carboplatin or cisplatin for metastatic NSCLC?
These data come from the randomized phase 3 KEYNOTE-189 trial [NCT02578680]. The patients in this trial had untreated stage IIIB or stage IV nonsquamous NSCLC without activating EGFR mutations or ALK translocations. The patients in the first arm received pemetrexed and pembrolizumab plus either carboplatin or cisplatin every 3 weeks for 4 cycles; this was followed by maintenance with pemetrexed plus pembrolizumab. Patients in the second [control] arm received pemetrexed and placebo plus either carboplatin or cisplatin, according to the same schedule, followed by maintenance with pemetrexed plus placebo. Patients in the control arm were allowed to cross over to the experimental arm at disease progression. The primary end points were overall survival [OS] and progression-free survival [PFS].2 A sustained improvement in OS was observed in the experimental arm compared with the control arm over 2 years of follow-up, with a hazard ratio of 0.56 [95% CI, 0.45-0.70]. Median OS was 22.0 months [95% CI, 19.5-25.2] in the experimental arm and 10.7 months [95% CI, 8.7-13.6] in the control arm. When the results were analyzed according to PD-L1 TPS (< 1%, 1%-49%, or ≥ 50%), it was found that patients experienced OS benefit irrespective of PD-L1 expression.3
What data support the use of single-agent pembrolizumab to treat patients with advanced or metastatic NSCLC?
The KEYNOTE-042 trial [NCT02220894] investigated single-agent pembrolizumab and is a good illustration of the fact that] PD-L1 expression should be regarded as a continuum rather than [as a series of discrete] cutoffs. In this trial, patients with untreated, locally advanced, or metastatic NSCLC of any histology with a PD-L1 TPS of 1% or more and with no sensitizing EGFR or ALK alterations were randomly assigned to 1 of 2 arms. Patients in the first arm received pembrolizumab every 3 weeks for up to 35 cycles. Patients in the second arm received carboplatin plus either paclitaxel or pemetrexed for up to 6 cycles; assignment of paclitaxel vs pemetrexed was dependent upon histology. Crossover was not allowed in this trial.4,5
In patients with a PD-L1 TPS of 1% or more, there was technically an OS benefit [in the pembrolizumab arm vs the chemotherapy arm]; the HR was 0.81 [95% CI, 0.71- 0.93; P = .0018]. For patients with a TPS of 20% or more, there was also some benefit [HR, 0.77; 95% CI, 0.64-0.92; P = .0020]. The greatest benefit was for patients with a TPS of 50% or more [median OS, 20 months vs 12.2 months, respectively; HR, 0.69; 95% CI, 0.56-0.85; P = .0003]; this subgroup drove the OS advantage.4,5
The subgroup that is [relevant to the patient we are discussing here is the subset of patients with] a PD-L1 TPS of 1% to 49%. There was no OS benefit for that subgroup; the HR was 0.92, with a 95% confidence interval that crosses 1 [95% CI, 0.77-1.11]. Most of the benefit was driven by the subgroup that had a PD-L1 TPS of 50% or more.4,5 I almost never use this regimen if a patient’s PD-L1 TPS is less than 50%. [In contrast], in the KEYNOTE-189 study, there was a substantial OS benefit for patients with a PD-L1 TPS of 1% to 49%.3 [In light of] the data, I prefer to use a combination regimen of chemotherapy [plus] immunotherapy6 for patients whose PD-L1 expression is less than 50%.
What data support the use of the quadruplet combination of atezolizumab, carboplatin, paclitaxel, and bevacizumab in recurrent, metastatic NSCLC?
This combination was studied in the IMpower150 trial [NCT02366143], a randomized trial with patients similar to those in KEYNOTE-189 trial, with stage IV, nonsquamous NSCLC. In contrast, this trial did not exclude patients with EGFR mutations. Patients were randomly assigned to 1 of 3 arms. In the first arm, patients received the combination of atezolizumab, carboplatin, and paclitaxel for 4 to 6 cycles, followed by atezolizumab maintenance. In the second arm, patients received the quadruplet combination of atezolizumab, carboplatin, paclitaxel, and bevacizumab, followed by maintenance with atezolizumab plus bevacizumab. Finally, in the third arm, patients received the combination of carboplatin, paclitaxel, and bevacizumab, followed by bevacizumab maintenance. Treatment with bevacizumab continued until disease progression; treatment with atezolizumab continued until disease progression or loss of clinical benefit.7
There was no OS advantage for the first arm vs the third arm. However, there was a benefit for the quadruplet arm vs the third arm [median OS, 19.2 months vs 14.7 months, respectively; HR, 0.78; 95% CI, 0.64-0.96; P = .02].7,8
For patients with liver metastasis or in patients with EGFR mutations, I would consider using this regimen if there were no clinical trial option or any other therapeutic option.
What data support the use of nivolumab plus ipilimumab vs chemotherapy in recurrent or advanced NSCLC?
This comparison was made in the CheckMate 227 study [NCT02477826], a study of stage IV or recurrent NSCLC in patients who had not had any prior systemic therapy and who had no [known] EGFR or ALK alterations. This study had 2 parts, each with 3 arms. In part 1A, patients with a PD-L1 expression level of at least 1% received one of the following regimens: single-agent nivolumab, nivolumab plus ipilimumab, or histology-based chemotherapy. Part 1B involved patients with a PD-L1 expression level of less than 1%; these patients received nivolumab plus histology-based chemotherapy, nivolumab plus ipilimumab, or histology-based chemotherapy. The coprimary end points in this trial were OS in patients with a PD-L1 expression level of at least 1% and PFS in patients with a TMB of 10 or more [both primary end points comparing nivolumab plus ipilimumab vs chemotherapy].9-11
Among patients with a PD-L1 expression level of at least 1%, there was an OS benefit with nivolumab plus ipilimumab compared with chemotherapy alone with a median OS of 7.1 months vs 14.9 months [HR, 0.76; 95% CI, 0.65- 0.90] and compared with nivolumab alone. Duration of response [DOR] and PFS benefits were maintained at 4 years.9 What is interesting in this trial are the results for patients with PD-L1 expression of less than 1%. There was an OS benefit with nivolumab plus ipilimumab vs chemotherapy with a median OS of 17.2 months vs 12.2 months, respectively [HR, 0.64; 95% CI, 0.51-0.81]. That may be one [situation in which] I would consider using nivolumab with ipilimumab. [However,] we have to be mindful that nivolumab and ipilimumab are not [substantially less toxic than] chemotherapy, and we still need long-term survival data.
For patients who received the nivolumab-plus-ipilimumab combination vs those who received chemotherapy, the adverse events [AEs] that are usually associated with chemotherapy, such as anemia, neutropenia, nausea, and decreased appetite, occurred in fewer patients. However, diarrhea, rash, and fatigue affected more patients in the nivolumab-plus-ipilimumab arm than in the chemotherapy arm, mostly because of the ipilimumab.12 The [AEs associated with] ipilimumab can be quite serious.13 I’ve seen patients [develop] significant myocarditis following just 1 cycle of nivolumab plus ipilimumab, such that I could not give these patients any more immune checkpoint inhibitors. In this study, among patients in the nivolumab-plus-ipilimumab arm vs those in the chemotherapy arm, serious treatment-related adverse events [TRAEs] affected a higher percentage of patients], and the percentage of patients with TRAEs leading to treatment discontinuation was almost double. The 2 arms had comparable [numbers of] treatment-related deaths.13
How do nivolumab and ipilimumab perform when combined with chemotherapy?
This was explored in the CheckMate 9LA trial [NCT03215706], another study of stage IV or recurrent NSCLC in patients who had received no prior systemic therapy and who had no sensitizing EGFR or ALK alterations. The patients were randomly assigned to receive either chemotherapy alone for 4 cycles or nivolumab/ipilimumab and 2 cycles of histology-specific chemotherapy. Treatment was given for 2 years [for immunotherapy] or until disease progression or unacceptable toxicity. The primary end point was OS. The secondary end points were PFS and objective response rate [ORR], as well as efficacy [assessed according to] tumor PD-L1 expression.14,15
The 2-year update showed an OS survival benefit with the combination of nivolumab, ipilimumab, and chemotherapy vs chemotherapy alone with a median OS of 15.8 months vs 11.0 months, respectively [HR, 0.72; 95% CI, 0.61-0.86]. The combination regimen vs chemotherapy alone also conferred a PFS benefit [median PFS, 6.7 months vs 5.3 months, respectively; [HR, 0.67; 95% CI, 0.56-0.79], an ORR benefit [38.0% vs 25.4%, respectively], and a prolonged DOR [median DOR, 13.0 months vs 5.6 months, respectively]. Additionally, in the subset analysis, the experimental regimen was found to confer an OS benefit irrespective of PD-L1 expression level.14 However, we need longer survival data. [Additionally, it should be noted that] the control arm in this study was not on par with the current standard of care; that makes it difficult to gauge which regimen is best. I would only use this option if a patient refused chemotherapy [alone], if they were PD-L1 negative, and if they were willing to only do a couple of cycles. This regimen is not my [first choice].
As was observed in the CheckMate 227 study, in CheckMate 9LA, the AEs that are [usually associated] with chemotherapy affected fewer patients in the combination arm than in the control arm.15,16 But remember, adding ipilimumab to nivolumab leads not only to a higher incidence of immunological AEs, but also to more severe [nonimmunological] AEs. It is challenging to diagnose and treat AEs that are induced by checkpoint inhibitor therapy because there’s no definite [time frame during which] these AEs [would be expected to occur]. Most occur within the first 6 months of treatment, but that’s not the rule; they can occur anytime. I’ve seen them occur as soon as the first day of receiving immune checkpoint inhibitors and as late as a year after starting treatment. You have to keep that in mind when using this combination regimen.
The combination of nivolumab and ipilimumab was approved by the FDA for patients with metastatic NSCLC in the first-line setting if their tumor expression level of PD-L1 is 1% or more.17 The more interesting results were those seen in PD-L1–negative patients, but [that application] doesn’t have FDA approval at this time. Finally, the nivolumab, ipilimumab, and chemotherapy regimen was approved for patients with metastatic NSCLC irrespective of PD-L1 expression.18
REFERENCES
1. NCCN. Clinical Practice Guidelines in Oncology. Non-small cell lung cancer, version 1.2022. Accessed December 12, 2021. https://bit.ly/3q52NtU
2. Gandhi L, Rodríguez-Abreu D, Gadgeel S, et al; KEYNOTE-189 Investigators. Pembrolizumab plus chemotherapy in metastatic non-small-cell lung cancer. N Engl J Med. 2018;378(22):2078-2092. doi:10.1056/NEJMoa1801005
3. Gadgeel S, Rodríguez-Abreu D, Speranza G, et al. Updated analysis from KEYNOTE-189: pembrolizumab or placebo plus pemetrexed and platinum for previously untreated metastatic nonsquamous non-small-cell lung cancer. J Clin Oncol. 2020;38(14):1505-1517. doi:10.1200/JCO.19.03136
4. Lopes G, Wu YL, Kudaba I, et al. Pembrolizumab (pembro) vs platinum-based chemotherapy (chemo) as first-line therapy for advanced/metastatic NSCLC with a PD-L1 tumor proportion score (TPS) ≥ 1%: open-label, phase 3 KEYNOTE-042 study. J Clin Oncol. 2018;36(suppl 18):LBA4. doi:10.1200/JCO.2018.36.18_suppl.LBA4
5. Mok TSK, Wu YL, Kudaba I, et al; KEYNOTE-042 Investigators. Pembrolizumab vs chemotherapy for previously untreated, PD-L1-expressing, locally advanced or metastatic non-small-cell lung cancer (KEYNOTE-042): a randomised, open-label, controlled, phase 3 trial. Lancet. 2019;393(10183):1819-1830. doi:10.1016/S0140-6736(18)32409-7
6. Keytruda. Prescribing information. Merck; 2021. Accessed December 15, 2021. https://bit.ly/3F9m57N
7. Socinski MA, Jotte R, Cappuzzo F, et al. Overall survival (OS) analysis of IMpower150, a randomized Ph 3 study of atezolizumab (atezo) + chemotherapy (chemo) ± bevacizumab (bev) vs chemo + bev in 1L nonsquamous (NSQ) NSCLC. J Clin Oncol. 2018;36(suppl 15):9002. doi:10.1200/JCO.2018.36.15_suppl.9002
8. Socinski MA, Jotte RM, Cappuzzo F, et al; IMpower150 Study Group. Atezolizumab for first-line treatment of metastatic nonsquamous NSCLC. N Engl J Med. 2018;378(24):2288-2301. doi:10.1056/NEJMoa1716948
9. Paz-Ares LG, Ciuleanu TE, Lee JS, et al. Nivolumab (NIVO) plus ipilimumab (IPI) vs chemotherapy (chemo) as first-line (1L) treatment for advanced non-small cell lung cancer (NSCLC): 4-year update from CheckMate 227. J Clin Oncol. 2021;39(suppl 15):9016. doi:10.1200/JCO.2021.39.15_suppl.9016
10. Hellman MD, Ciuleanu T, Pluzanski A, et al. Nivolumab (nivo) + ipilimumab (ipi) vs platinum-doublet chemotherapy (PT-DC) as first-line (1L) treatment (tx) for advanced non-small cell lung cancer (NSCLC): initial results from CheckMate 227. Paper presented at: 2018 American Association for Cancer Research Annual Meeting; April 14-18, 2018; Chicago, Illinois. Accessed December 14, 2021. https://bit.ly/3yCVsW7
11. Hellmann MD, Ciuleanu TE, Pluzanski A, et al. Nivolumab plus ipilimumab in lung cancer with a high tumor mutational burden.N Engl J Med. 2018;378(22):2093-2104. doi:10.1056/NEJMoa1801946
12. Yervoy. Prescribing information. Bristol Myers Squibb; 2021. Accessed December 15, 2021. https://bit.ly/3meOIJ0
13. Reck M, Ciuleanu TE, Manuel Cobo, et al. First-line nivolumab (NIVO) plus ipilimumab (IPI) plus two cycles of chemotherapy (chemo) vs chemo alone (4 cycles) in patients with advanced non-small cell lung cancer (NSCLC): two-year update from CheckMate 9LA.
14. Hellmann MD, Paz-Ares L, Bernabe Caro R, et al. Nivolumab plus ipilimumab in advanced non-small-cell lung cancer. N Engl J Med. 2019;381(21):2020-2031. doi:10.1056/NEJMoa1910231
15. 2021. J Clin Oncol. 2021;39(suppl 15):9000. doi:10.1200/JCO.2021.39.15_suppl.9000
16. Paz-Ares L, Ciuleanu TE, Cobo M, et al. First-line nivolumab plus ipilimumab combined with two cycles of chemotherapy in patients with non-small-cell lung cancer (CheckMate 9LA): an international, randomised, open-label, phase 3 trial. Lancet Oncol. 2021;22(2):198-211. Published correction appears in Lancet Oncol. 2021;22(3):e92.
17. Reck M, Ciuleanu TE, Cobo Dols M, et al. Nivolumab (NIVO) + ipilimumab (IPI) + 2 cycles of platinum-doublet chemotherapy (chemo) vs 4 cycles chemo as first-line (1L) treatment (tx) for stage IV/recurrent non-small cell lung cancer (NSCLC): CheckMate 9LA. J Clin Oncol. 2020;38(suppl 15):9501. doi:10.1200/JCO.2020.38.15_suppl.9501
18. FDA approves nivolumab plus ipilimumab for first-line mNSCLC (PD-L1 tumor expression ≥1%). FDA. Updated May 15, 2020. Accessed December 15, 2021. https://bit.ly/327oZeW
19. FDA approves nivolumab plus ipilimumab and chemotherapy for first-line treatment of metastatic NSCLC. FDA. Updated May 27, 2020. Accessed December 15, 2021. https://bit.ly/3GNJmMI