Shammo Debates the Triggers for Treatment of Patients With High-Risk Myelofibrosis
During a Targeted Oncology case-based virtual event, Jamile M. Shammo, MD, discussed testing, risk assessment, and therapy for patients with high-risk myelofibrosis.
Jamile M. Shammo, MD (Moderator)
Professor of Medicine and Pathology
Rush Medical College

SHAMMO: I always [go for bone marrow testing] because MF is one of those entities [for which] you must demonstrate fibrosis by doing a bone marrow biopsy.
Granted, you must rule out other entities that could present as MF, so accessing next-generation sequencing [NGS] may give you some very important prognostic features. You could obtain results from the peripheral blood, but it is an incredibly important diagnostic and prognostic tool.
KOKO: I tend to use a combination of the criteria as well as the bone marrow diagnosis. I do rely on the hematopathology to read the bone marrow biopsy specimen, which gives me information as to whether [the disease] is fibroses or atypical megakaryocytes.
Often, differential diagnosis could be essential thrombocythemia, especially in the patient who is not the sickest.
KASSEM: After you get a JAK2-positive or -negative result, one of the things you would want to figure out, or rule out, is whether it’s primary or secondary myelofibrosis. That being said, a bone marrow biopsy does help in defining a particular percentage [of patients], but it is not something that we often see in many cases.
However, one of the diagnostic criteria is [determining] a Dynamic International Prognostic Scoring System [DIPSS] score to define the risk classification, if you are truly thinking of myelofibrosis. Otherwise, I would also think of it as part of the [myelodysplastic syndrome (MDS)] conversion.
SHAMMO: You are correct, because MDS with fibrosis is one of the differential diagnoses, at least from a pathological perspective, and you are also right in that you want to do an IPSS risk stratification. However, that’s done once the diagnosis of myelofibrosis is made.
For instance, say you couldn’t find a driver mutation—but if you found JAK2 it would make treatment easier. But what if it’s one of those triple-negative [cases]? Then how easy is it to make that diagnosis of MF? Sometimes it can be difficult if you want to make sure that there are 2 or 3 [or more areas of] fibrosis.
You also want to rule out other entities, like chronic myeloid leukemia, MDS, fibrosis, or perhaps other entities with neurotensin or myeloproliferative syndrome [MPS] overlaps. You also want to demonstrate clonal nature of the myeloproliferative neoplasms that you are dealing with by showing JAK2 or some other clonal hematopoiesis.
Ten percent of the patients with myelofibrosis [MF] don’t have that which could be problematic. Granted, you can look at the megakaryocytic morphology, and if [the patient has] dysplasia, then of course you are guided by the cytogenetics, because that too may be very helpful.
FLEJSIEROWICZ: In our system, we usually request [testing for] specific mutations, but they come as a panel, too. Then our strong hematology person is always reminding [us about] requesting the NGS on new cases. There is so much [that is targetable to treat at this moment], but maybe prognostically I’ll ask a little bit more about what the course of the disease may be.
KALAKOTA: [Our practice is pretty similar.] I’ll usually order a JAK2 test, then it’ll reflex to MPL or CALR mutations, so it usually goes sequentially from there. Then once the diagnosis has been confirmed, I’ll order high-risk mutations for further analysis, but that’s a separate test.
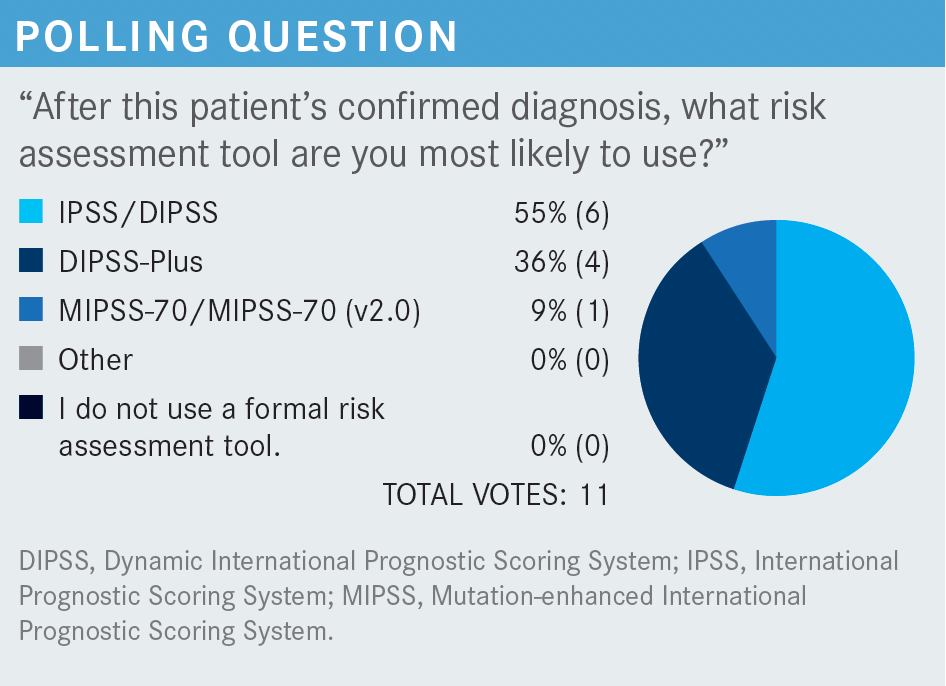
SHAMMO: I am pleased to see that no one does not use any formal risk assessment tool. Everybody [should] use some form of risk assessment, because this is a disease [in which] allogeneic [transplantation] and subtransplantation is of use and is a curative therapy. So, it’s very important, and even from a prognostic perspective, it’s important to get an idea about where a patient may be going because the disease is characterized by heterogeneity.
FLEJSIEROWICZ: I’ll just talk for myself, a person who is not a MF specialist, but I do happen to practice in an inner-city hospital, where anything comes through the door. I have encountered several cases in my now 16-year career at that practice and, to my surprise, 2 of those patients who were categorized as high risk were then [aged] in their 60s.
Transplant was offered to them, and they refused. Despite what the cytogenetics said, these patients are still around, still alive. They may be struggling with cytopenia at their [first line of treatment], but in my experience, those high-risk patients have not transformed or progressed.
[Again in my] limited experience, I have noticed that some patients who would be [classified as] intermediate risk ended up having lots of cytopenias. Those were the patients I worried about the most, and in fact, they did progress faster than cytogenetics would tell me.
SHAMMO: I do think that when people talk about risk, it’s exactly that: a risk. I could take 100 patients who may have an increased risk, but maybe your patient happens to be the one that [actually doesn’t have that increased risk]. [Calculating risk is] good from a statistical perspective, but it might not apply for particular patients. That comment about transplant is totally not new to me because I have been through the same experience with my own patients.
I don’t know if the transplanter has scared the patients by talking about risks and benefits. Even when you go through the data, there is a whole lot of room for improvement, but [undoubtedly] this is the only curative option that we have. Nevertheless, it may have to do also with some older patients’ philosophy that they would rather focus on quality of life rather than the word cure.
SHAMMO: [At the time of] diagnosis, [we] assess their risk by utilizing one of the risk models. This is the recommendation of the [National Comprehensive Cancer Network].1 For example, if you have the Mutation-enhanced IPSS [MIPSS] score, MIPSS70 or MIPSS70+, [and] you have the IPSS+, then you can use the MYSEC [Myelofibrosis Secondary to PV and ET] prognostic model in the secondary setting. So, now you have risk stratification between low risk and high risk, depending on the score.
KALAKOTA: For [a patient whom] I’ve been following [most recently], I have been using the symptom-burden tool. Using the 10 symptoms that are listed, including fatigue, bone pain, cytopenias, and weight loss, I kind of gauge those symptoms as a trigger of when to start treatment.
SHAMMO: So, you go with the symptoms—but what about timing? Is there any timing to start that? For instance, do you do the symptom assessment form when the patient tells you something in particular—like splenomegaly-related symptoms? Is it weight loss, night sweats? What particular trigger might you get? Or, do you do the symptom assessment form every time they come to see you in the clinic?
FLEJSIEROWICZ: Pretty much I [follow that], and then it’s all symptom driven. Also, if there’s progression of anemia, [and] the spleen gets bigger, they complain about early satiety and they cannot perform their daily activities. So that’s where I always try to find where the window really is. Do I wait until they’re very sick? Or do I intervene before they get very sick? That’s a struggle; it always is.
SHAMMO: How important is it to start treatment early? Or, how should we be thinking about starting treatment early? Or, should we even [change their treatment], for that matter? Any insight on this from the rest of the group?
KOKO: [I think this question] is something to be debated. If the patient is asymptomatic, I am not sure what the benefit of initiating therapy would be. I have waited for a patient to be symptomatic unless they have severe cytopenia, but if they are asymptomatic, I don’t initiate any therapy.
SHAMMO: Can anyone [else] weigh in on the [decision when a patient is] asymptomatic, or on early vs late [treatment]?
KOKO: When you say “early,” what I have done is initiate therapy earlier on at the presentation of symptoms, not necessarily late.
SHAMMO: The question when it comes to [initiating therapy] early is kind of a trick. I don’t mean that the question is tricky, obviously, but the question is, when it comes to their symptoms, how hard have we looked at those symptoms? How [closely] have we assessed those patients? [I ask this because] sometimes those diseases tend to be chronic, so the patients may learn how to live with them. [The patient may] gradually diminish their level of physical activity without even noticing, and if they are becoming slightly or gradually more anemic, they may not even notice that they are basically getting more and more fatigued or tired.
[Furthermore, if] their spleen is [gradually] getting larger and larger, they may not even actually report symptomatology. So, it is very tricky, and I agree with you. I don’t claim to know the right answer, but I am just saying that I think what you said about cytopenia resonates with me. If we are utilizing drugs that do tend to cause cytopenia, then I think, from a practical perspective, there probably is no reason to wait for the patient to develop a bad cytopenia. Then you are going to start drugs that will cause them to have even more cytopenias, and then you may have issues with that. Nevertheless, that’s a point of debate. There are no trials of early vs late [treatment initiation], but I think it is a matter of debate and certainly [to be determined on] a case-by-case basis.
So, what about clinical trial involvement? Have you had the chance to consider patients for clinical trials?
FLEJSIEROWICZ: Well, that’s ideally what we should be doing, so I always look and make sure that I am not missing anything—although there are not a lot of trials for which our patients are eligible, or are ongoing, at my practice. Many times, patients ask [whether a trial is available], and nothing has been recently, at least [at my practice]. Not too many people are willing to travel, [although] Chicago is around the corner. Again, I am only speaking [of] my practice, in which most patients are inner-city patients, and they don’t have means to get to a bigger center or [to be seen] outside the [Medicaid system].
SHAMMO: It is difficult to put patients on clinical trials, in general, in the United States. However, this is not a reason for us to stop [trying to get them on trials]. Of course, I am biased, but I think all of us need to consider that as a possibility to improve on those [options] that we already have.
REFERENCE
1. NCCN. Clinical Practice Guidelines in Oncology. Myeloproliferative neoplasms, version 1.2021. Accessed December 10, 2021. https://bit.ly/31QFMCD