Eskander Addresses HRD in Newly Diagnosed Ovarian Cancer
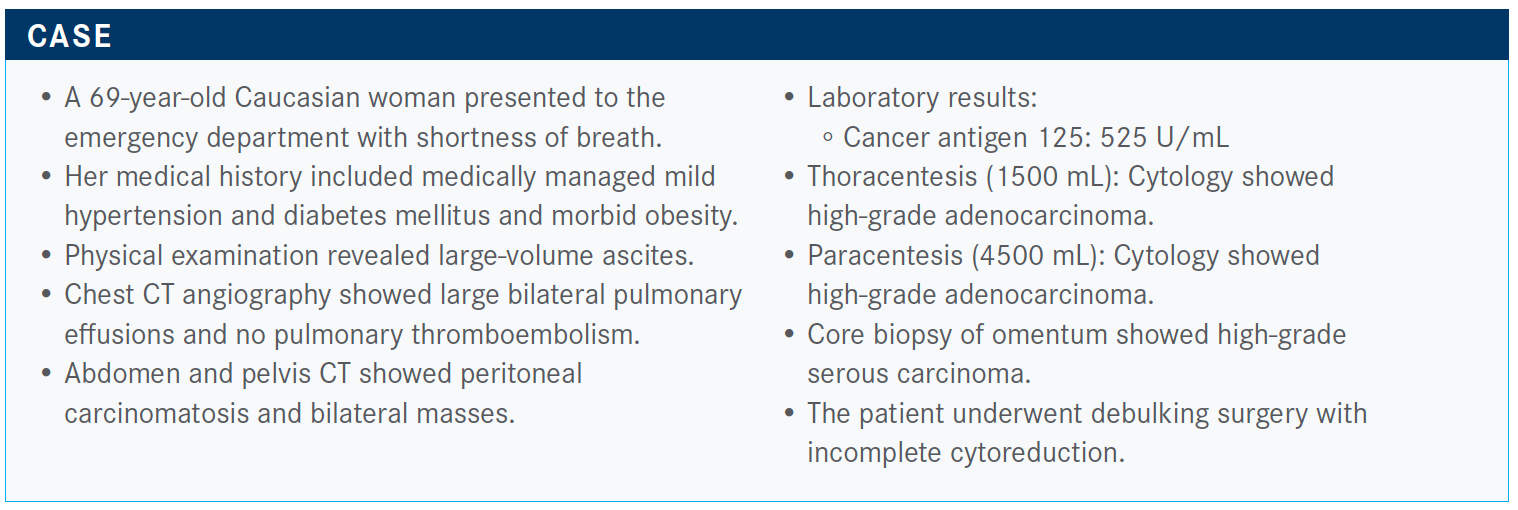
During a Targeted Oncology Case Based Peer Perspective event, Ramez N. Eskander, MD, reviewed the case of a 69-year-old woman with newly diagnosed ovarian cancer.
Ramez N. Eskander, MD

During a Targeted Oncology Case Based Peer Perspective event, Ramez N. Eskander, MD, gynecologic oncologist, assistant professor of Obstetrics, Gynecology, and Reproductive Sciences, Moores Cancer Center, University of California San Diego Health in La Jolla, CA, reviewed the case of a 69-year-old woman with newly diagnosed ovarian cancer.
Targeted Oncology™: Reviewing this patient’s case, what would be your treatment plan of action?
ESKANDER: In my practice, this patient would be treated with neoadjuvant chemotherapy initially because of disease bulk and burden. The patient had large-volume ascites and bilateral pleural effusions that were determined to be malignant based on cytology [findings]. I would probably proceed with neoadjuvant chemotherapy followed by an interval of cytoreduction because the goal is a complete resection with no visible residual disease.
We have moved away from secondary laparotomies or laparoscopies. We have moved away from secondary cytoreductions because of the results from the GOG-0213 trial [NCT00565851].1 That trial was slightly different compared with this case because that trial looked at patients with platinum-sensitive recurrence. It showed that those patients did worse if they underwent cytoreduction, rather than immediately starting them on systemic chemotherapy.
If I’m concerned about cytoreduction, I will usually start with a diagnostic laparoscopy, [to determine] whether or not I can completely resect. If I’m worried that I can’t [resect], then I consider biopsy and neoadjuvant chemotherapy.
What role does bevacizumab (Avastin) play in a patient such as this?
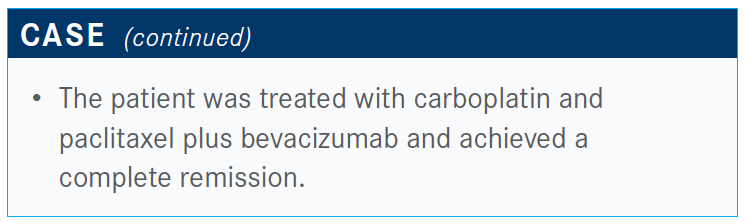
I will use bevacizumab in the neoadjuvant setting even if I’m treating with chemotherapy with an intention to proceed with an interval cytoreduction. I just hold [bevacizumab] the cycle before the patient undergoes surgery, and I hold it for the cycle after surgery. Then I resume normal [treatment] afterward.
How does a cytology evaluation affect your treatment plan moving forward?
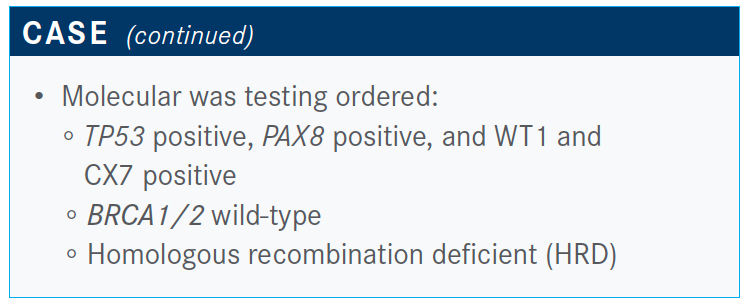
This patient underwent molecular testing of her tumor. She underwent the cytology evaluation in addition to a thoracentesis, a paracentesis, and an omental biopsy. The reason that is important is the cytology isn’t going to allow you to send tumor for molecular testing. For patients with large-volume disease, I would advocate for making sure the interventional radiologist biopsies a tumor implant itself, so that you can have the ability for molecular testing if you feel like there is utility in the neoadjuvant setting.
The omental biopsy was sent for molecular testing, and this patient was BRCA1/2 wild-type, no evidence of a somatic aberration, and germline testing was negative. But the [patient’s tumor] was HRD—so it was submitted, tested, and found to be HRD.
What do the National Comprehensive Cancer Network (NCCN) guidelines recommend regarding the use of bevacizumab in BRCA1/2 wild-type disease?
If patients have wild-type BRCA or unknown complete response or a partial response after primary treatment, the NCCN guidelines allow for the combination of bevacizumab and olaparib [Lynparza].2
What is the primary reason you might opt for single-agent bevacizumab over the combination of bevacizumab and olaparib as maintenance therapy for a patient such as this?
Our clinical picture of the patient so far shows suboptimal cytoreduction, HRD, and complete response to chemotherapy plus bevacizumab. If you elect to choose bevacizumab monotherapy rather than the combination of bevacizumab and olaparib, is it because of a concern about adverse events, cost to the patient, concerns about reimbursement, not enough efficacy data, or another reason altogether?
I think the majority of oncologists are concerned about adverse effects associated with the combination, followed by cost to the patient.
What is the evidence for using a PARP inhibitor for maintenance in a patient who has HRD?
The way the data are maturing in the ongoing clinical trials and based on the information so far, you would think that there is a compelling reason to offer patients PARP inhibitors in this population. Is it offered by everyone? No. There are providers who may not offer a maintenance strategy for these patients.
Some oncologists might argue that until there is an overall survival difference; they might not be convinced. The SOLO2 trial [NCT01874353] results showed that a maintenance strategy in patients with recurrent, BRCA-mutated, and platinum-sensitive disease resulted in a 13-month overall survival difference, which was a fairly dramatic number.3 Still, there are some providers who do not use a maintenance treatment strategy for the front line in ovarian cancer, even with the FDA approvals and the data that we have.
If this patient had a germline BRCA1/2 mutation, what would you offer as maintenance therapy?
If the patient is a carrier for a germline BRCA mutation, we could offer bevacizumab maintenance, bevacizumab plus olaparib, olaparib monotherapy, niraparib [Zejula] monotherapy, or another option. I think the most common treatment would be bevacizumab plus olaparib.
How would you choose between bevacizumab plus olaparib versus PARP monotherapy for a patient with germline mutant BRCA who was previously treated with a bevacizumab-containing primary therapy?
I would consider adverse effects, cost to the patient, concerns about reimbursement, and magnitude of the benefit associated with the combination, which suggests that combining bevacizumab with olaparib in this setting is clinically significant.
I think the majority of practicing oncologists would say the magnitude of the benefit of the combination is the major factor, followed by adverse effects and cost to the patient. That suggests that the data from SOLO-1 [NCT01844986] are so provocative that olaparib monotherapy would be sufficient and that there aren’t enough clinical data right now to suggest that adding olaparib to bevacizumab in this setting would be any better than olaparib alone.4
If this patient had BRCA wild-type homologous recombination–proficient disease, what would you offer as maintenance therapy?
In this patient, after maintenance therapy, I would consider niraparib monotherapy; so, stop the bevacizumab and transition to niraparib.
How does the use of frontline bevacizumab affect your second-line therapy? Would it have any impact on your choices?
There are data looking at giving bevacizumab post initial bevacizumab administration. The progression-free survival advantage is preserved. Giving bevacizumab post bevacizumab initially preserves the magnitude of benefit, at least with respect to progression-free survival.
