Exploring Treatments in Patients With Favorable-Risk RCC
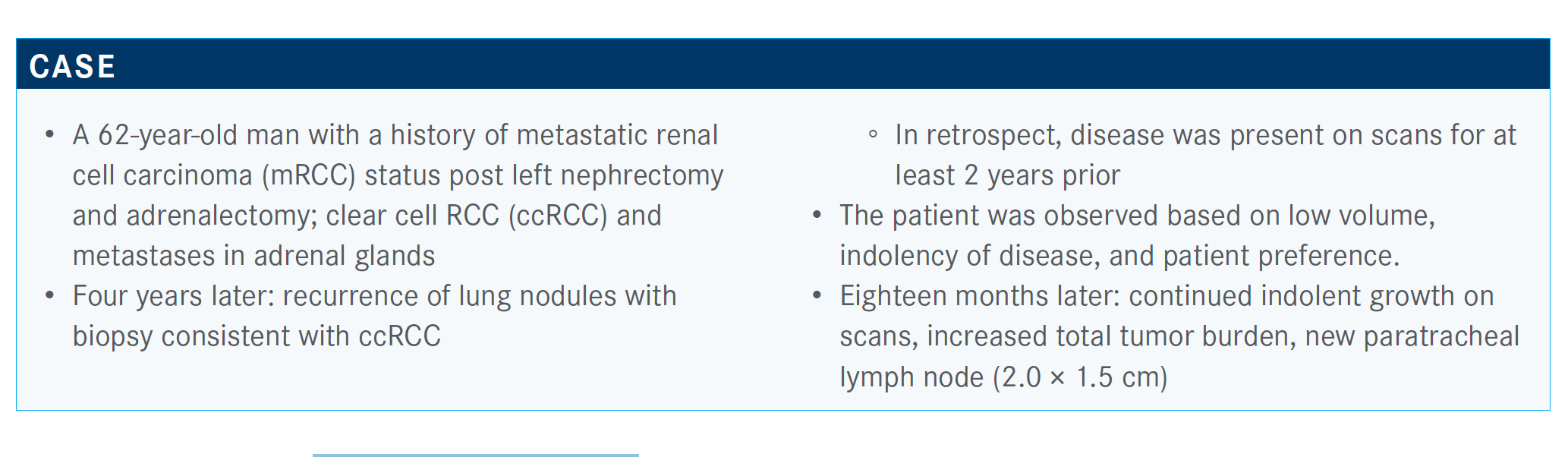
During a Targeted Oncology Case Based Peer Perspectives event, Marc Matrana, MD, MS, discussed the case of a 62-year-old male patients with renal cell carcinoma.
Marc Matrana, MD, MS

During a Targeted Oncology Case Based Peer Perspectives event, Marc Matrana, MD, MS, director, Precision Cancer Therapies (Phase I) Research Program, Endowed Professor of Experimental Therapeutics, and associate director of Clinical Cancer Research at Ochsner Cancer Institute, discussed the case of a 62-year-old male patients with renal cell carcinoma (RCC).
Targeted Oncology™: What additional work-up do you typically order for patients such as this one?
MATRANA: He has favorable risk; zero risk factors puts him at favorable risk. If you have a CT of a chest, abdomen, and pelvis, to me, that’s about all you need in these patients; that’s enough. As I was trained, and in my opinion, PET scans in RCC are difficult because they’re hit-or-miss. Sometimes RCC [shows up and sometimes it doesn’t], so if you get a negative PET, that doesn’t tell us a whole lot. If you get a positive PET scan, that’s fine, but negative PET is not enough, let’s say.

How do you feel about these poll results?
I like pazopanib [Votrient], but I’m not [sure] we should do that for this patient. A lot of folks are saying axitinib [Inlyta]/pembrolizumab [Keytruda] or nivolumab [Opdivo]. Looks [as though] we [have] an equal number. A good number of folks say nivolumab/ipilimumab. A lot [said] cabozantinib [Cabometyx]. None of these [is] wrong. We don’t have good head-to-head data [for] these therapies. All of these are potential treatments [in this case]. They’re all valid.
In a patient who has low-volume indolent disease such as this, which is slowly progressive, would you consider using up-front radiation therapy and then continue observing?
It depends on the burden of their disease. If it’s oligometastatic, meaning that they just have 1 or 2 small spots, then we’ll try to render them no evidence of disease [NED] with metastasectomy or radiofrequency ablation, or in some cases with radiation. I have a patient right now who has a history [such as] this. He had a nephrectomy, and then he had a thyroid recurrence.
How would you characterize pancreatic metastases in RCC for this patient?
Years later, the patient [had] a metastasectomy, then it was discovered that he had a pancreatic recurrence. A little caveat, pancreatic metastasis in RCC is a very indolent disease. That’s a marker for very indolent disease. This guy [had] a partial pancreatectomy, and then he had another recurrence.
So, he was able to avoid systemic therapy for a long time with that approach. He has just recently had a worsening of his disease. A switch has been flipped. But if we can render somebody with NED and who has indolent disease, by all means, we [avoid systemic therapy].
Now, in this particular case, I think the issue was that the patient had multiple bilateral pulmonary nodules. They were small but they were growing. That’s a little bit more difficult and challenging because of a wider spread disease burden.
But [it’s ideal] to render people with NED. And even if you don’t think that this person is going to get a long-term cure, if I can get another 2 or 3 years without progression of disease out of a metastasectomy, I definitely think that’s worth it, because their overall survival [OS] just jumped by that much.
What do the National Comprehensive Cancer Network (NCCN) guidelines recommend in this setting?
If we look at our NCCN guidelines regarding favorable risk, the preferred regimens are axitinib, pembrolizumab, pazopanib, sunitinib, and other great regimens.1 For patients who are at poor or intermediate risk, the preferred regimens are ipilimumab [Yervoy]/ nivolumab [Opdivo] or axitinib/pembrolizumab in category 1, or cabozantinib.
For KEYNOTE-426 (NCT02853331), what do outcomes for patients with a favorable risk look like?
When we looked at the favorable risk, it’s interesting. Our control arm fared a bit better compared with sunitinib, but not necessarily as well as those who had intermediate and poor risk.2
We see no real difference in the OS. The hazard ratio, confidence interval, 0.6 to 1.8; so, no real difference in OS there. Progression-free survival [PFS] [trended] better in the pembrolizumab/axitinib arm. The hazard ratio is 0.7, but still that confidence interval crosses 1. Overall response rate definitely looks a little better, 50% versus almost 70% with a jump in that complete response rate, so 11% in the pembrolizumab/axitinib arm.
Which first-line tyrosine kinase inhibitors (TKIs) compare with each other?
First-line TKI therapy involves pazopanib and sunitinib. The study evaluating sunitinib compared it [with] interferon-α.3 Median PFS was 11 months.
Median PFS on pazopanib [was] 8.4 months.4,5 Median OS [was] a bit better in the pazopanib arm, 28 months.
That said, these 2 have been compared head-to-head in the COMPARZ trial [NCT00720941] by Motzer.6 It was a noninferiority trial, so it wasn’t powered to say if one was better than the other. But what it did show was that pazopanib was noninferior to sunitinib, so they were at least the same.
There was another study that was conducted that was essentially a patient preference study, and patients did prefer pazopanib over sunitinib due to a more favorable adverse effect profile.
How does sunitinib compare with nivolumab/ipilimumab in this setting?
We could look at OS in the CheckMate 214 study [NCT02231749] for favorable-risk patients.7 When we look at this, we get some interesting data. The data showed a trend toward the sunitinib arm at 18 months, at 30 months, and even down to 42 months, where we have a difference of only 3%. But throughout the course of treatment, we see a bit of favoring of sunitinib in the patients with favorable-risk RCC, as compared with nivolumab/ipilimumab alone.
Were there any interesting findings for the confirmed responses reported in CheckMate 214?
When we look at confirmed response rates, we can see that intermediate and poor risk certainly favored nivolumab/ipilimumab, but when we look at the favorable-risk population, the response rate favored sunitinib, and I think that was a surprise. For some reason favorable risk seems to respond better to VEGF blockade and VEGF TKIs.
When we examine PFS, we saw similarities for favorable-risk patients. Median PFS at 17.5 months was 70% with sunitinib, 46% with nivolumab/ipilimumab. When we go out to 42 months, 28% compared [with] 34%. So, something about that VEGF TKI for patients with favorable-risk RCC is important.

What do these findings suggest about patients with favorable risk?
I think the take-home message is [that] with favorable risk, you probably want to think about TKI VEGF blockade in the up-front setting, even if it is with immunotherapy. I think that’s fine, but I think that VEGF is important.
[As far as] evolving approaches in advanced RCC, I think the interferon-α inhibitors are the next big thing we’ll see approved in this setting. How it will all play out with the other targeted therapies, the immunotherapies, who knows? There will probably be some head-to-head studies that will be done in years to come.
Several years ago, our options were high-dose IL [interleukin]-2 and interferon-α, but today there are a dozen different options to choose from. We’re in a much better place with this disease.
References:
1. NCCN. Clinical Practice Guidelines in Oncology. Kidney cancer, version 1.2021. July 15, 2020. Accessed October 15, 2020. https://bit.ly/37a7jPV
2. Plimack ER, Rini BI, Stus V, et al. Pembrolizumab plus axitinib versus sunitinib as firstline therapy for advanced renal cell carcinoma (RCC): updated analysis of KEYNOTE- 426. J Clin Oncol. 2020;38(suppl 15):5001. doi:10.1200/JCO.2020.38.15_suppl.5001
3. Motzer RJ, Hutson TE, Tomczak P, et al. Overall survival and updated results for sunitinib compared with interferon-α in patients with metastatic renal cell carcinoma. J Clin Oncol. 2009;27(22):3584-3590. doi:10.1200/JCO.2008.20.1293
4. Motzer RJ, Hutson TE, Cella D, et al. Pazopanib versus sunitinib in metastatic renalc ell carcinoma. N Engl J Med. 2013;369(8):722-731. doi:10.1056/NEJMoa1303989
5. Motzer RJ, Hutson TE, McCann L, Deen K, Choueiri TK. Overall survival in renal-cell carcinoma with pazopanib versus sunitinib. N Engl J Med. 2014;370(18):1769-1770. doi:10.1056/NEJMc1400731
6. Motzer RJ, Hutson TE, Cella D, et al. Pazopanib versus sunitinib in metastatic renal cell carcinoma. N Engl J Med. 2013;369:722-731. doi:10.1056/NEJMoa1303989
7. Motzer RJ, Tannir NM, McDermott DF, et al. Nivolumab plus ipilimumab versus sunitinib in advanced renal-cell carcinoma. N Engl J Med. 2018;378(14):1277-1290. doi:10.1056/NEJMoa1712126

Enhancing Precision in Immunotherapy: CD8 PET-Avidity in RCC
March 1st 2024In this episode of Emerging Experts, Peter Zang, MD, highlights research on baseline CD8 lymph node avidity with 89-Zr-crefmirlimab for the treatment of patients with metastatic renal cell carcinoma and response to immunotherapy.
Listen
Beyond the First-Line: Economides on Advancing Therapies in RCC
February 1st 2024In our 4th episode of Emerging Experts, Minas P. Economides, MD, unveils the challenges and opportunities for renal cell carcinoma treatment, focusing on the lack of therapies available in the second-line setting.
Listen