CASPIAN Trial Results Offer Another Option for SCLC
The results from the phase 3 CASPIAN trial were reviewed and compared with the phase 3 IMpower133 by Jyoti D. Patel, MD, during a Targeted Oncology Case Based Peer Perspectives event.
Jyoti D. Patel, MD

The results from the phase 3 CASPIAN trial were reviewed and compared with the phase 3 IMpower133 by Jyoti D. Patel, MD, professor of Medicine, (Hematology and Oncology), and associate vice chair for Clinical Research at Northwestern University in Chicago, IL during a Targeted Oncology Case Based Peer Perspectives event.
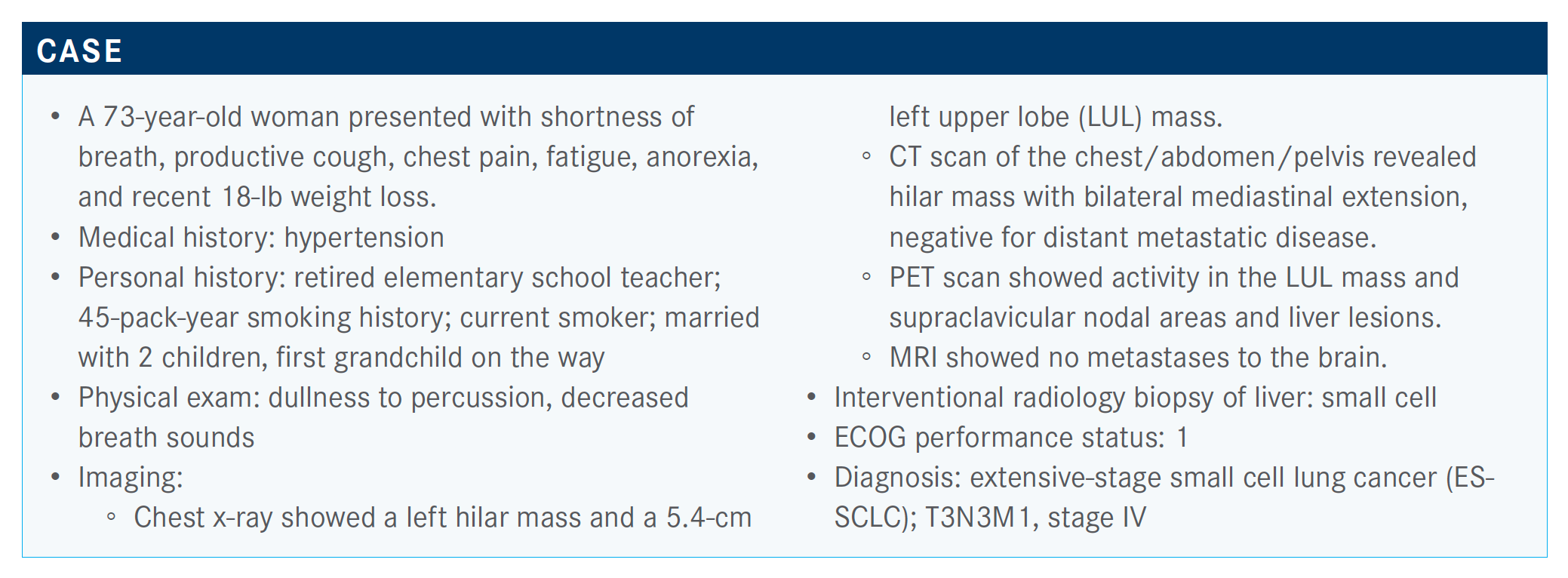
Targeted Oncology™: What do the National Comprehensive Cancer Network (NCCN) guidelines suggest in this setting?
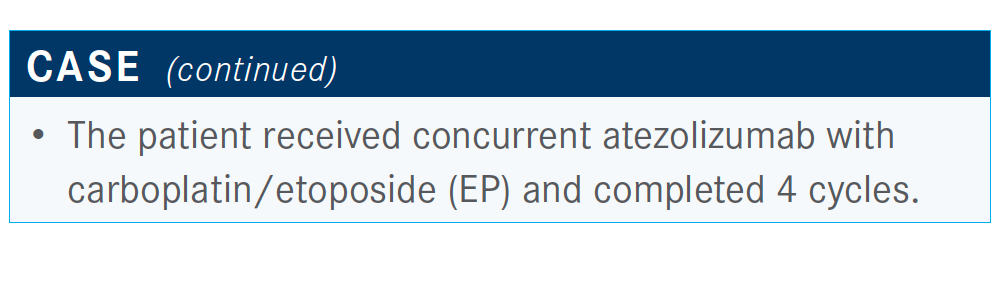
PATEL: Atezolizumab [Tecentriq] has been approved, [and] now durvalumab [Imfinzi] has been approved.1 With durvalumab, you have the option of using either carboplatin or cisplatin. But those are the 3 preferred therapies.
What are the data that support using atezolizumab?
Half have used atezolizumab with chemotherapy, and half haven’t.
In IMpower133 [NCT02763579], patients were randomized 1:1.2 I think the salient points are that patients had good performance status and that brain metastases had to be treated before patients could go on. Often in clinical practice, if patients are asymptomatic, we usually just move forward. The primary end point was overall survival [OS].
There was a 2-month difference between atezolizumab and EP versus EP alone [for OS; HR, 0.70; 95% CI, 0.54-0.91; P = .007] and less than a month’s [difference] in the progression-free survival [PFS]. At 1 year, this was where you see the difference…during the initial treatment period, patients were the same [in both arms].
How did patients respond according to updated data?
The updated data from 2-year OS [showed] the survival benefit persisted.3 It was still 2 months’ [difference]. The hazard ratio was less than 0.80; it was those patients who benefit a bit later. Depressingly, the Kaplan-Meier curves came together, as many people have noted with small cell disease further down the road.
All subgroups tend to benefit from immunotherapy; there are no subgroups who don’t benefit modestly. The brain metastases’ confidence interval was wide—that’s such a small number of patients who were enrolled [n = 35]. Patients with liver metastasis tended to benefit. Numerically, their OS was a bit worse; OS was 16.3 months [with atezolizumab] for patients with no liver metastases compared with placebo with liver metastases, 7.8 months—so very different patient populations.
They were able to ascertain TMB [tumor mutational burden] in a significant proportion of patients. The patients with high TMB fared a bit better. This wasn’t all patients; it was a subset of patients who had sufficient tissue, about half of patients.
What other important information did the trial show?
In terms of response, as has been indicated, these patients respond early to chemotherapy.2 The problem is keeping it—the number of complete responses was numerically higher with atezolizumab. The overall response rate was slightly higher [with placebo], but I don’t think [there were] many differences in terms of radiographic response.
In terms of adverse events [AEs], immunotherapy, when given with chemotherapy, does not cause significant toxicity when both drugs are given. So, this regimen was generally well tolerated. A lot of the toxicity was hematologic, as one would expect from platinum and etoposide.
Other AEs of special interest were the immune-related AEs [like] rash. Thyroid and endocrine disorders were a bit higher with atezolizumab, as one would expect.
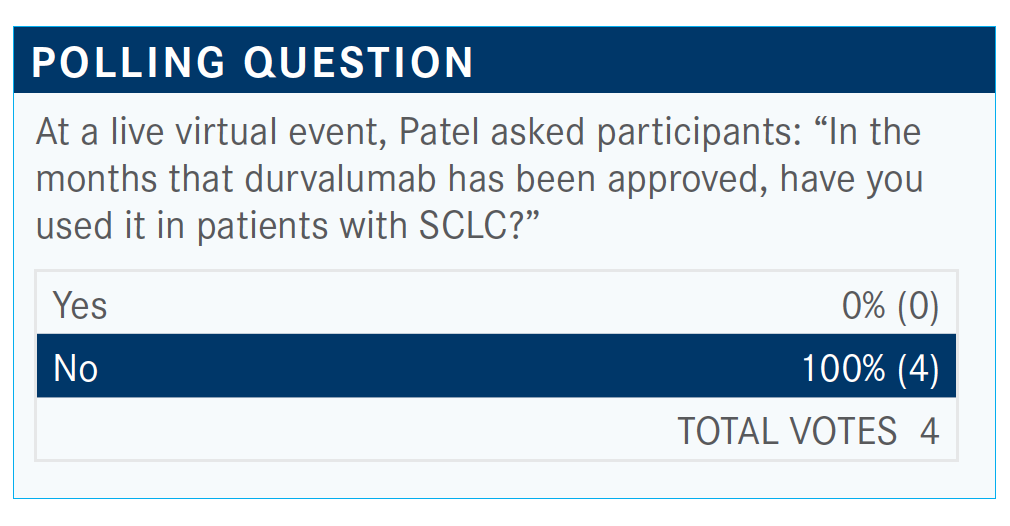
Which trial is relevant for the use of durvalumab in this setting?
The CASPIAN study [NCT03043872] was presented with tremelimumab at the ASCO [American Society of Clinical Oncology] meeting this year.4 These patients could have asymptomatic and untreated brain metastasis and could get either cisplatin or carboplatin. It was a 3-arm study, with durvalumab/tremelimumab— CTLA-4 inhibition—with EP versus durvalumab plus EP versus EP. The primary end point was OS.
The primary end point of the durvalumab trial was presented last year.5 That led to the approval. What I think is most interesting about this trial is how similar it looks to the IMpower133 regimen. The placebo arm is exactly the same [median OS, 10.5 months], and in the durvalumab arm, the immuno-oncology arm is about the same, at 12.9 months.4 There was a similar hazard ratio of 0.75 [95% CI, 0.62-0.91; P = .0032]. All subgroups seemed to benefit.
The updated median PFS…for these curves ended up looking similar. The PFS with durvalumab and EP numerically was a bit less, at 5.1 [months versus 5.4 with EP]. But the hazard ratio favored the addition of durvalumab, at 0.80. There was a broad difference at 18 months, 13.9 months PFS versus 3.4 [months PFS with durvalumab/EP versus EP]. That persisted at [24 months].
The response rate was slightly higher with durvalumab, 68% versus 58%.
What was the efficacy in the tremelimumab arm compared with the other 2 arms?
I think what’s interesting about this is we didn’t expect those patients would do less well than with durvalumab alone. But it’s better than chemotherapy. Durvalumab/EP is significantly better if you look at OS: 12.9 months with durvalumab/EP; with durvalumab/What was the efficacy in the tremelimumab arm compared with the other 2 arms?
I think we can explain some of that worse survival with tremelimumab primarily based on the safety data. With both CTLA-4 and PD-L1, the toxicities were higher; there was a higher [rate] of grade 3/4 toxicities [with tremelimumab], at 70% versus 62% with durvalumab/EP and 63% with EP. Serious AEs were 46% with tremelimumab, AEs leading to discontinuation [were 21%], and 36% of these patients had immune-related AEs.
Importantly, 4.5% of patients on the durvalumab/tremelimumab arm had AEs leading to death, [which is] significantly higher than we see in most frontline trials.
How do IMpower133 and CASPIAN compare?
The 2 studies head-to-head [have] similar follow-up. The number of patients was a bit higher in CASPIAN with the 3 arms. The control arm was 4 [cycles in IMpower133] versus 6 [cycles in CASPIAN]. A lot of patients on CASPIAN got 6 cycles of therapy. The OS is similar. So we can say with confidence that [median OS with] chemotherapy is about 10.3 to 10.5 months. Hazard ratios are similar, and the toxicities are similar.
What do you think is to come in this setting?
We know that immunotherapy [has] level 1 evidence that changed practice. But none of us are that happy with the improvements we’ve done. There’s still a lot of work to do. I’d say anecdotally, some of my longest-term responders are patients who’ve had ipilimumab [Yervoy]/nivolumab [Opdivo] as second-line therapy, [before] atezolizumab and durvalumab. So I’m still a bit conflicted.
Then trying to figure out now what to do post immunotherapy progression in the second-line setting—whether it’s etoposide or a taxane. I think it’s up for grabs, and whether or not you end up rechallenging those patients with single-agent immunotherapy after immunotherapy is unclear to me.
References:
1. NCCN. Clinical Practice Guidelines in Oncology. Small cell lung cancer; version 1.2021. Accessed October 12, 2020. https://bit.ly/3nEPnCJ
2. Horn L, Mansfield AS, Szczęsna A, et al; IMpower133 Study Group. First-line atezolizumab plus chemotherapy in extensive-stage small-cell lung cancer. N Engl J Med. 2018;379(23):2220-2229. doi:10.1056/NEJMoa1809064
3. Reck M, Liu SV, Mansfield AS, et al. IMpower133: updated overall survival (OS) analysis of first-line (1L) atezolizumab (atezo) + carboplatin + etoposide in extensive-stage SCLC (ES-SCLC). Ann Oncol. 2019;30(suppl 5):v710-v717. doi:10.1093/annonc/mdz264
4. Paz-Ares LG, Dvorkin M, Chen Y, et al. Durvalumab Å} tremelimumab + platinum etoposide in first-line extensive-stage SCLC (ES-SCLC): updated results from the phase III CASPIAN study. J Clin Oncol. 2020;38(suppl 15):9002. doi:10.1200/JCO.2020.38.15_suppl.9002
5. Paz-Ares L, Dvorkin M, Chen Y, et al; CASPIAN Investigators. Durvalumab plus platinum-etoposide versus platinum-etoposide in first-line treatment of extensive-stage small-cell lung cancer (CASPIAN): a randomised, controlled, open-label, phase 3 trial. Lancet. 2019;394(10212):1929-1939. doi:10.1016/S0140-6736(19)32222-6
