Chao Discusses How Ruxolitinib Broadens Treatment Options in GVHD
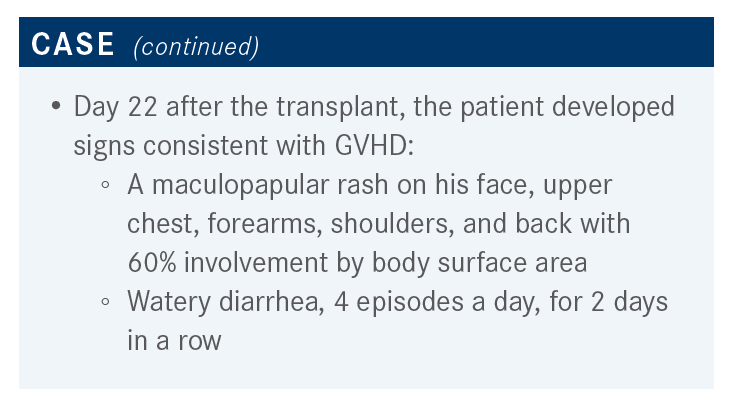
During a Targeted Oncology Case-Based Roundtable event, Nelson Jen An Chao, MD of Duke University School of Medicine discussed a 48-year-old patient with graft-vesus-host disease.
Nelson Jen An Chao, MD
During a Targeted OncologyTM Case-Based Roundtable event, Nelson Jen An Chao, MD of Duke University School of Medicine discussed a 48-year-old patient with graft-vesus-host disease.
Targeted OncologyTM: What are the risk factors for GVHD in this type of patient?
CHAO: The major risk factor is donor-recipient HLA [human leukocyte antigen] mismatch, that is, major mismatch or minor mismatch.1,2 Mismatching is important, but it’s primarily important for multiparous women because they have been HLA sensitized, which reflects a donor parity. Age is important [as] older donors can cause more GVHD than younger donors.1 CMV serostatus is important. Multiple cytokines have been associated with GVHD. Stem cell source is important. Peripheral blood has been shown to cause more, primarily chronic GVHD, than bone marrow; and umbilical cord probably causes the least amount of GVHD. Graft composition makes a difference, so the higher CD34 count, the higher the risk.1,2 With transplantation factors, the conditioning regimen makes a difference; the more intensive the conditioning, the higher the risk of GVHD.3
Can you describe the recent data that you would consider for staging and grading this patient’s GVHD?
The recent MAGIC [Mount Sinai acute GVHD] international consortium [is 1 method for staging and grading], and it’s not very different from either the Glucksberg or CIBMTR [Center for International Blood and Marrow and Transplant Research] grading.4,5 It’s basically [evaluating] the same 3 major systems: the skin, liver, and gut. The difference is they have added persistent nausea, vomiting, and anorexia to the GI [gastrointestinal] tract [in stage 1].5 So, the skin and the liver is no different, but they’ve added not only the volume of diarrhea but also the number of episodes. This is a great example where stage 0 is obvious, stage 4 is obvious, stage 3 is probably obvious as well, and the real problem is in [assessment of] stage 2.
These are people with enough of a skin rash [that you are] worried about GVHD. Some liver [abnormalities, bilirubin] elevation, and [the] diarrhea is more than you would expect from toxicity from the chemotherapy, or the fact that they had pizza the night before, or something that would have caused them more discomfort. Ultimately, the major problem that we frequently have in GVHD is [in assessing] grade 2, where they have a rash, some liver abnormalities, or some GI problems. You’re never sure how much of the liver involvement is due to the azole that they’re on or [if] the [problems in the] GI tract [are] because they ate something they shouldn’t. The problem that we have had for decades is that [determining if someone is stage 2] is a clinical diagnosis that we don’t have a fixed system of biomarkers for yet. Although that is being developed and will hopefully help us in this grading system.
Recently, Maggie MacMillan in Minneapolis pooled [the] data [of 1723 patients] to look at a GVHD risk score.6 She was able to stratify these patients to standard and high risk based on the number of organs involved and which organs were involved. This stratification allowed her to [determine which] people were standard risk, meaning that [they] would have a reaction to steroids, vs those who [were high risk and] would have a less optimal response to steroids. So, if [a patient] had single organ involvement, be that the skin [at stages 1 through 3] or single involvement of the GI tract [at stage 1 or 2, they were in the standard risk group]. If [a patient] had 2 organs involved, either the skin [at stage 1 through 3] and the GI tract [at stage 1], or the skin [at stage 1 through 3] and the liver [at stage 1 through 4], they would likely respond to steroids [and were also considered standard risk]. Basically everything else was in the high-risk group. The probability of treatment-related mortality was doubled in the high-risk group vs the standard-risk group, and this is useful information as we think about clinical trials; if [there are] a lot of patients in the high-risk group, that will impact outcomes. [MacMillan found that] the percentage of response is a reflection upon whether the patient is [considered] standard risk or high risk. So, if [the patient was considered] standard risk, the chances of getting a complete response or partial response to steroids was high, it was in the 70% range. Whereas less than 50% of patients who were considered high risk [had a] complete response or partial response to steroids.
How quickly do you determine whether the patient is steroid-refractory or steroid-dependent?
In general, most of us would accept that the steroid [refractoriness or resistance] is usually within 3 to 5 days.8 If somebody [has progression of acute GVHD within] 3 to 5 days of taking [at least] 2 mg/kg/day of prednisone, or they don’t improve after [5 to 7 days of treatment initiation], or they don’t have a response after 28 days [of treatment], that is refractory resistance. If they are steroid-dependent, the idea is that you can’t taper [prednisone] below 2 mg/kg/day, or every time you try to taper [off steroids], they [have a recurrence of acute GVHD]. Intolerance is people who don’t tolerate steroids, [like having blood] sugars over 800, which is commonly seen.
What data helps direct your choice of therapy for treatment of acute GVHD beyond steroids?
The NCCN [National Comprehensive Cancer Network] guidelines [do not list any preferred agents for second-line therapy], but they do list agents that are commonly used among NCCN member institutions].9 They encourage steroid-refractory acute GVHD to be managed as part of a clinical trial. Even though there is 1 drug that is FDA approved, clinical trials are still 1 of the major ways to go, if we can. Ruxolitinib [Jakafi] is approved as a category 1, but there are lots of different drugs [that can be used to treat acute GVHD]. In chronic GVHD, there’s also 1 drug approved, ibrutinib [Imbruvica], which is similar. These drugs are trying to impact either the cytokines associated with response or trying to target the T cells.10,11
The REACH1 study [NCT02953678] was a phase 2 study that looked at the utility of ruxolitinib in 70 patients with steroid-refractory acute GVHD.12,13 Patients received 5 mg of ruxolitinib twice daily plus steroids, with or without a calcineurin inhibitor; the primary end point was the ORR [overall response rate] at day 28. What ruxolitinib is thought to do is impact antigen presentation through the dendritic cell, which tunes down the IL-23 and IL-12 signaling to decrease IL-17 and IL-22. This impacts Th17 cells, which we think are 1 of the primary immune mediators of acute GVHD. Ruxolitinib is also thought to tune down interferon-ɣ, IL-2 and TNF-α which drives Th17 cells. The ORR [in REACH1] was 55% [at day 28] with 26.8% achieving a complete response.14,15 [The best] ORR at any time during treatment was 73%, the median time to response was fairly rapid at 7 days, and the median duration response was almost 1 year. Ruxolitinib was reasonably well tolerated, and the median overall survival was not reached.
How has data for the REACH 2 (NCT02435433) study impacted your decision making?
[REACH1 results] led to the phase 3 randomized study, called REACH2, [which randomized] almost 300 patients with steroid-refractory acute GVHD [to receive 10 mg of ruxolitinib twice daily plus steroids, with or without a calcineurin inhibitor] or [the control therapy, which was the investigator’s choice of best alternative therapy (BAT)].13,14
[BAT was limited to the following choices: ATG (antithymocyte globulin), ECP (extracorporeal photopheresis), mesenchymal stromal cells, low-dose methotrexate, mycophenolate mofetil (CellCept), everolimus (Zortress) or sirolimus (Rapamune), etanercept (Enbrel), or infliximab (Remicade)].
Patients were randomized to BAT vs ruxolitinib, which allowed for crossover of those [who received BAT] to get ruxolitinib if they hadn’t responded. The end point was ORR for acute GVHD at day 28, [defined as the proportion of patients who had a complete response or partial response as compared with baseline organ staging without the use of additional systemic therapy.]15 There were a lot of secondary end points as well. The ORR at day 28 was significantly better for ruxolitinib, 62% vs 39% [for BAT], and the OR [odds ratio] was 2.64 [95% CI, 1.65- 4.22; P < .001]. [At day 56, ruxolitinib demonstrated a] reasonably durable overall response of 40%, [while BAT was 22% (OR, 2.38; 95% CI, 1.43-3.94; P < .001)]. At day 28, if you break ORR down by the full analysis set of grade 2, grade 3, and grade 4, each of these subsets still favored ruxolitinib. The odds ratio was significant for [the full analysis set (OR, 2.64; 95% CI, 1.65-4.22), grade 2 (OR, 2.96; 95% CI, 1.30-6.76), grade 3 (OR, 2.15; 95% CI, 1.10-4.20), and grade 4 (OR, 3.76; 95% CI, 1.24-11.38).]
[The response duration] tended to be lasting, so the patients on ruxolitinib were better controlled, [and there] was less loss of response with ruxolitinib than the BAT.14
This was important for the [organ staging from baseline to day 28]. Ruxolitinib [showed more improvement in the acute GVHD stage] than BAT both in the skin and the GI tract. [This suggests that], in each of these organs, ruxolitinib also controlled the disease better. One of the more important findings was failure-free survival, and patients who were on ruxolitinib were more likely to stay in response compared to those who received BAT [HR, 0.46; 95% CI, 0.35-0.60].

What adverse events are most concerning with ruxolitinib?
One of the things that is encouraging is that it is not a new drug, it’s been used for other conditions, and [in REACH2, the adverse events are] what you would have expected.14 We know from other hematologic disorders that ruxolitinib causes thrombocytopenia, so [it is] not surprising that thrombocytopenia was much more common. Other than that, [there was] not much difference between ruxolitinib and the other alternative therapies that were allowed. Perhaps slightly more CMV infection, but not a large number.
REFERENCES
1. Flowers ME, Inamoto Y, Carpenter PA, et al. Comparative analysis of risk factors for acute graft-versus-host disease and for chronic graft-versus-host disease according to National Institutes of Health consensus criteria. Blood. 2011;117(11):3214-3219. doi:10.1182/blood-2010-08-302109
2. Grube M, Holler E, Weber D, Holler B, Herr W, Wolff D. Risk Factors and Outcome of Chronic Graft-versus-Host Disease after Allogeneic Stem Cell Transplantation-Results from a Single-Center Observational Study. Biol Blood Marrow Transplant. 2016;22(10):1781-1791. doi:10.1016/j.bbmt.2016.06.020
3. Hahn T, McCarthy PL Jr, Zhang MJ, et al. Risk factors for acute graft-versus-host disease after human leukocyte antigen-identical sibling transplants for adults with leukemia. J Clin Oncol. 2008;26(35):5728-5734. doi:10.1200/JCO.2008.17.6545
4. Harris AC, Young R, Devine S, et al. International, Multicenter Standardization of Acute Graft-versus-Host Disease Clinical Data Collection: A Report from the Mount Sinai Acute GVHD International Consortium. Biol Blood Marrow Transplant. 2016;22(1):4-10. doi:10.1016/j.bbmt.2015.09.001
5. Rowlings PA, Przepiorka D, Klein JP, et al. IBMTR Severity Index for grading acute graft-versus-host disease: retrospective comparison with Glucksberg grade. Br J Haematol. 1997;97(4):855-864. doi:10.1046/j.1365-2141.1997.1112925.x
6. MacMillan ML, Robin M, Harris AC, et al. A refined risk score for acute graft-versus-host disease that predicts response to initial therapy, survival, and transplant-related mortality. Biol Blood Marrow Transplant. 2015;21(4):761-767. doi:10.1016/j.bbmt.2015.01.001
7. Levine JE, Logan BR, Wu J, et al. Acute graft-versus-host disease biomarkers measured during therapy can predict treatment outcomes: a Blood and Marrow Transplant Clinical Trials Network study. Blood. 2012;119(16):3854-3860. doi:10.1182/blood-2012-01-403063
8. Schoemans HM, Lee SJ, Ferrara JL, et al. EBMT-NIH-CIBMTR Task Force position statement on standardized terminology & guidance for graft-versus-host disease assessment. Bone Marrow Transplant. 2018;53(11):1401-1415. doi:10.1038/s41409-018-0204-7
9. NCCN. Clinical Practice Guidelines in Oncology. Hematopoietic cell transplantation: pre-transplant recipient evaluation and management of graft-vs-host disease, version 2.2021. Accessed July 22, 2021. https://www.nccn.org/professionals/physician_gls/pdf/hct.pdf
10. Jakafi. Prescribing information. Incyte Corporation; 2020. Accessed July 22, 2021. https://www.jakafi.com/pdf/prescribing-information.pdf
11. Imbruvica. Prescribing information. Pharmacyclics; 2020. Accessed July 22, 2021. https://www.imbruvica.com/files/prescribing-information.pdf
12. Jagasia M, Zeiser R, Arbushites M, Delaite P, Gadbaw B, Bubnoff N. Ruxolitinib for the treatment of patients with steroid-refractory GVHD: an introduction to the REACH trials. Immunotherapy. 2018;10(5):391-402. doi:10.2217/imt-2017-0156
13. Jagasia M, Perales MA, Schroeder MA, et al. Ruxolitinib for the treatment of steroid-refractory acute GVHD (REACH1): a multicenter, open-label phase 2 trial. Blood. 2020;135(20):1739-1749. doi:10.1182/blood.2020004823