Schuster Addresses Treatment Options in DLBCL Treatment
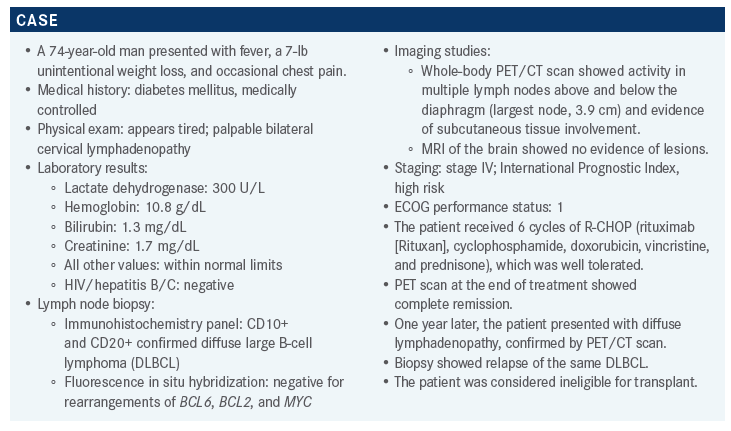
One year after being diagnosed with CD-10- positive and CD10-positive diffuse large B-cell lymphoma being treated with R-CHOP, and achieving complete remission, a PET/CT scan confirmed relapse in a 74-year-old male patient.
Stephen J. Schuster, MD
One year after being diagnosed with CD-10- positive and CD10-positive diffuse large B-cell lymphoma (DLBCL), being treated with R-CHOP, and achieving complete remission, a PET/CT scan confirmed relapse in a 74-year-old male patient.
Stephen J. Schuster, MD, the Robert and Margarita Louis-Dreyfus professor in Chronic Lymphocytic Leukemia and Lymphoma Clinical Care and Research in the Division of Hematology Oncology, Perelman Center for Advanced Medicine, University of Pennsylvania, discussed this case during a Targeted OncologyTM Cased-Based Roundtable event.
Targeted OncologyTM: What are the treatment options for a patient like the one described here?
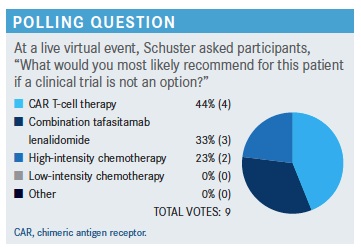
SCHUSTER: The National Comprehensive Care Network [NCCN] guidelines [offer several regimens] for second-line and subsequent therapies for large B-cell lymphoma patients who are not transplant candidates.1 Gemcitabine [Gemzar] plus oxaliplatin [GemOx] with or without rituximab is preferred by the NCCN. I’m not enthusiastic about GemOx as a stand-alone regimen, though it [can serve as] a bridge to other things. Polatuzumab vedotin-piiq [Polivy], the CD79b-directed drug-antibody immunoconjugate, [is also a preferred therapy], with or without bendamustine and with or without rituximab. One of the newer regimens is the tafasitamab [Monjuvi] plus lenalidomide [Revlimid] regimen.
The other [regimens suggested by the NCCN] are combinations of existing antimetabolite [drugs] and alkylating agents; I’m [not enthusiastic about these] if [the patient has] already failed rituximab-based alkylating agent therapy. [For patients with CD30-positive disease,] brentuximab vedotin [Adcetris] is an option. Bendamustine plus rituximab is listed as “useful in certain circumstances,” though I do not like it. Ibrutinib [Imbruvica] is good for activated B-cell or nongerminal center B-cell [non-GCB] disease, particularly if there is an activating CD79 mutation. I like [ibrutinib] because it preserves T cells and is a good bridge to chimeric antigen receptor [CAR] T-cell therapy or other immunotherapies that might [require] an endogenous and somewhat fit immune system. [Last on the list is] lenalidomide with or without rituximab, [which is likewise] more active in non-germinal center or CD10-negative DLBCL. Occasionally, that can lead to a fairly durable remission.
What notable guidelines does the NCCN offer for patient follow-up?
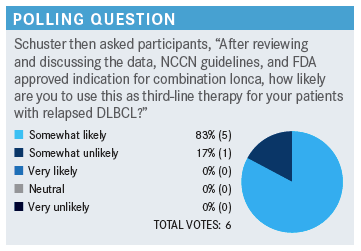
If [the patient] achieves a complete response [after an alternative in the second line], you [need to consider] allogenic transplant [for consolidation]. When you get to the third line and later, you’ve got to [consider their present therapy] as a bridge to potential CAR T-cell therapy. That’s why it’s paramount to preserve the immune system with your third line of therapy. [Approved agents for third-line therapy and later include] loncastuximab tesirine [Zynlonta], an antibody-chemotherapy immunoconjugate, and selinexor [Xpovio], a [nuclear] export inhibitor.
What is your opinion about this treatment choice?
This [combination] was approved in July 2020.3 It was primarily studied as the second line of therapy, so for this patient, it would [be appropriate].4 I’d be careful with this patient’s creatinine clearance. You have to adjust lenalidomide for renal function, and a patient of this age with renal insufficiency is not going to tolerate the standard regimen that begins with 25 mg for 21 days out of a 28-day cycle.
What is the mechanism of action of this combination?
Lenalidomide increases natural killer [NK] cells, enhances antibody-dependent cell-mediated cytotoxicity, and [also] has some direct effects [on cell death]. Tafasitamab is a CD19-directed [antibody], but the key to this doublet is that the Fc portion of this recombinant antibody has been engineered to enhance its interaction with the Fc receptor. It interacts with NK cells and macrophages much better.
What data support the use of tafasitamab plus lenalidomide in a patient such as this?
The L-MIND study [NCT02399085] is the trial that led to the FDA approval of the tafasitamab plus lenalidomide combination.4 [Enrolled patients could] have had up to 3 prior regimens. These patients were not eligible for high-dose chemotherapy with transplant. Tafasitamab [12 mg/kg] was given weekly during the first month and then on days 1 and 15 for cycles 4 through 12, [with 25 mg of lenalidomide given daily]; after a year, tafasitamab was given alone. It was not uncommon to have to reduce the lenalidomide. Patients on this trial were treated until they had either intolerance or progressive disease. The primary end point was objective response rate [ORR].5,6
The median patient age was 72. With respect to cell of origin [as identified by gene-expression profiling], 24% of the study population had non-GCB disease, 9% had GCB disease, and the cell of origin was unclassified or unknown in the remaining 67%. [About half of the patients had an International Prognostic Index score of 0 to 2; the other half had a score of 3 to 5,] and there was a similar distribution of patients with and without elevated lactate dehydrogenase levels. Fifty percent of the patients [received the experimental combination] as the second line of therapy, 43% received it as the third line. Nineteen percent of the patients were primary-refractory patients, and 42% were refractory to their last prior therapy.
At a median follow-up of 13.2 months, the ORR was 60% [95% CI, 48%-71%], the complete response [CR] rate was 43% [95% CI, 32%-54%], and the partial response [PR] rate was 18% [95% CI, 10%-28%]. A best response of stable disease occurred in 14% of patients [95% CI, 7%-23%], progressive disease in 16% [95% CI, 9%-26%], and disease control in 74% [95% CI, 63%-83%]. The median duration of response was 21.7 months [95% CI, 21.7– not reached (NR)].6 These responses were durable; when length of follow-up was at least 35 months, the CR rate was 40% and the ORR was 57.5% [95% CI, 45.9%-68.5%]; the median duration of response was 43.9 months [95% CI, 26.1-NR].7 [This study population was] a little biased towards non-GCB [disease], but these are reasonable results.
At a median follow-up of 17.3 months, the median progression-free survival [PFS] was 12.1 months [95% CI, 5.7-NR].6 What impresses me about this PFS curve is that it seems to plateau at a year; when the median follow-up was extended to 33.9 months, median PFS was 11.6 months [95% CI, 6.3-45.7].7 At a median follow-up of 19.6 months, median overall survival [OS] was not reached [95% CI, 18.3-NR],6 and at a median follow-up of 42.7 months, median OS was 33.5 months [95% CI, 18.3-NR].7
Duration of response was analyzed separately for patients with a CR and for patients with a PR. At a follow-up of at least 35 months, patients with a CR did the best; their median response duration was not reached [95% CI, 43.9-NR]. But even among patients who had a PR, median duration of response was 5.6 months [95% CI, 2.2-NR].8 For all patients, the median duration of response was 43.9 months [95% CI, 26.1-NR].
Is this regimen a potential cure [or does it] just control the disease?
I suspect there will be a proportion of these patients that are going to be durably responding and [you might even] say “cured.” But we have to wait.
How does the fact that this patient has only received 1 prior line of therapy influence your opinion of tafasitamab plus lenalidomide as a treatment option?
In L-MIND, efficacy [was evaluated according to the] number of lines of prior therapy. The response rate was highest in patients [who had received only 1 prior line of therapy]; 47.5% had a CR, and the ORR was 67.5% [95% CI, 50.9%-81.4%].7 So the choice of [this treatment combination] is very reasonable for this patient. If you’re thinking of using this [combination], [it is] better to use it as your second line of therapy; the patients who had 2 or more lines of prior therapy didn’t do quite as well, with an ORR of 57.5% [95% CI, 45.9%-68.5%].
For those patients who did not achieve a CR they should be able to proceed with CAR T-cell therapy?
Right. Many people are concerned that there could be loss of CD19 antigen, and a small number of patients could potentially lose CD19, [but] I’ve studied this a lot and [CD19] is very infrequently lost.
I also believe that the fact that [the therapy] is not toxic to T cells may keep this option open for patients. On this trial, I know of several patients who went on to CAR T-cell therapy successfully afterwards. CAR T-cell therapy is not excluded as a backup for third-line therapy for people who progress, or even [for patients who are] stable and [whom] you want to [improve].
If you’re in doubt, you can biopsy and look at CD19 expression…we stained all of our biopsies on the JULIET trial [NCT02445248] for CD19 expression and we found the same response rates to CD19-directed CAR T-cell therapy in patients who expressed and [in those who] didn’t express CD19.8
What impresses you the most about this drug combination?
I’m very impressed by the plateau in the PFS [curve]; there’s a proportion of patients that are going to [do well] for quite some time. Also, CRs that last more than a couple years usually bode well for a good outcome.
What adverse events (AEs) were observed during this study?
The [most common] AEs were neutropenia, which occurred in 49% of patients; anemia, in 34%; and thrombocytopenia, in 31%. Febrile neutropenia occurred in 12% of patients, but there was not much sepsis or mortality from sepsis. Lymphopenia only occurred in 5% of patients, and that’s important because most of the circulating peripheral lymphocytes are going to be T cells, TNK cells, or NK cells, and they’re what you want to preserve in case you have to move on to third lines of therapy like CAR T-cell therapy. Alopecia [was not reported]; patients will like that.4
[Other AEs, likely attributable to] lenalidomide, [included] fatigue in 17% of patients, diarrhea in 33%, and rash in 36%. However, none of this was grade 4 or lethal. Rash tends to [occur in the] first cycle [of treatment and can be treated with steroids]. The [change in] bowel habits can be a problem, and sometimes I use a little loperamide [Imodium] or something [similar]. Serious AEs occurred in 51% of patients and 9% had AEs of special interest [3 tumor flares, 1 basal cell carcinoma, and 3 allergic dermatitis]. Of the AEs that lead to death, [which represented 13% of the patients], none were considered drug-related. [In the tafasitamab monotherapy phase], some of these adverse effects persisted, [most commonly neutropenia, anemia, and diarrhea].9
Did some of these patients receive granulocyte colony-stimulating factor [GCSF] or prophylactic antibiotics?
They did receive GCSF. This [treatment] regimen is designed to be tolerable, so you should [be able to] adjust it so [that patients are] not routinely neutropenic. In [neutropenic] patients, I may use GCSF once or twice, but then I adjust the lenalidomide. If [a patient is] severely neutropenic, I’ll interrupt the lenalidomide, [administer] GCSF so they recover, and then resume the next cycle.
Regarding prophylactic antibiotics in this study, it was investigator’s choice. I put all of my patients with relapsed lymphomas and [those] getting primary therapy…on prophylaxis for varicella-zoster virus. I give them valaciclovir [Valtrex] or acyclovir [Sitavig/Zovirax]. If a patient has CD4 counts over 200 cells/mm3, which most of these patients [do], I don’t necessarily do Pneumocystis pneumonia prophylaxis.
What other data show the benefit of tafasitamab plus lenalidomide versus lenalidomide alone?
The RE-MIND study [NCT04150328] was a matching-adjusted indirect comparison analysis. [The investigators] found studies that together reported [on] 490 lenalidomide-monotherapy patients. They matched 76 of these patients with 76 L-MIND patients [with respect to multiple baseline covariates]. [Between these 2 groups], they found a best ORR of 67.1% [95% CI, 55.4%-77.5%] for the tafasitamab plus lenalidomide [L-MIND] group versus only 34.2% [95% CI, 23.7%-46.0%] for the lenalidomide-monotherapy group [odds ratio, 3.89; 95% CI, 1.90- 8.14; P < .0001].10
Do you think there is any role for adding rituximab to this combination?
Yes, but I think tafasitamab is a better [choice] because [tafasitamab] is designed to work better with NK cells. Now, I [did] publish a paper on lenalidomide and rituximab in Clinical Cancer Research [NCT00783367]. We [gave] patients, [most of whom had follicular lymphoma], lenalidomide monotherapy; after a few months, we did more CT [scans] and then gave the [patients] 4 weeks of rituximab. The rituximab did [augment] the responses of those patients, and some of the responses were quite durable.11 So I would certainly consider [adding rituximab] as opposed to monotherapy with lenalidomide.
REFERENCES
- NCCN. Clinical Practice Guidelines in Oncology. B-cell lymphomas, version 4.2021. Accessed July 21, 2021. https://bit.ly/3ijO4Zu
- Bourbon E, Salles G. Polatuzumab vedotin: an investigational anti- CD79b antibody drug conjugate for the treatment of diffuse large B-cell lymphoma. Expert Opin Investig Drugs. 2020;29(10):1079-1088. doi:10.1 080/13543784.2020.1800638
- FDA grants accelerated approval to tafasitamab-cxix for diffuse large B-cell lymphoma. US Food and Drug Administration. July 31, 2020. Updated August 3, 2020. Accessed July 18, 2021. https://bit.ly/2VpvAhd
- Salles G, Duell J, González Barca E, et al. Tafasitamab plus lenalidomide in relapsed or refractory diffuse large B-cell lymphoma (L-MIND): a multicentre, prospective, single-arm, phase 2 study. Lancet Oncol. 2020;21(7):978-988. doi:10.1016/S1470-2045(20)30225-4
- Salles G, Duell J, González Barca E, et al. Primary analysis results of the single-arm phase II study of MOR208 plus lenalidomide in patients with relapsed or refractory diffuse large B-cell lymphoma (L-MIND). Hematol Oncol. 2019;37(suppl 2):173-174. doi:10.1002/hon.130_2629
- Düll J, Maddocks KJ, Gonzalez-Barca E, et al. Long-term analyses from L-MIND, a phase II study of tafasitamab (MOR208) combined with lenalidomide (LEN) in patients with relapsed or refractory diffuse large B-cell lymphoma (R/R DLBCL). J Clin Oncol. 2021;39(suppl 15):7513. doi:10.1200/JCO.2021.39.15_suppl.7513
- Duell J, Maddocks KJ, González-Barca W, et al. Long-term analyses from L-MIND, a phase II study of tafasitamab (MOR208) combined with lenalidomide (LEN) in patients with relapsed or refractory diffuse large B-cell lymphoma (R/R DLBCL). Paper presented at: American Society of Clinical Oncology Annual Meeting; June 4-8, 2021; virtual. Accessed July 21, 2021. https://bit.ly/3xjNSO3
- Schuster SJ, Bishop MR, Tam CS, et al; JULIET investigators. Tisagenlecleucel in adult relapsed or refractory diffuse large B-cell lymphoma. N Engl J Med. 2019;380(1):45-56. doi:10.1056/ NEJMoa1804980
- Salles G, Duell J, González Barca E, et al. Long-term outcomes from the phase II L-MIND study of tafasitamab (MOR208) plus lenalidomide in patients with relapsed or refractory diffuse large B-cell lymphoma. Paper presented at: 25th European Hematology Association Annual Congress; June 11-21, 2020; virtual. Accessed July 21, 2021. https://bit.ly/3ltWL5v
- Nowakowski GS, Rodgers TD, Marino D, et al. RE-MIND study: a propensity score-based 1:1 matched comparison of tafasitamab + lenalidomide (L-MIND) versus lenalidomide monotherapy (real-world data) in transplant-ineligible patients with relapsed/refractory (R/R) diffuse large b-cell lymphoma (DLBCL). J Clin Oncol. 2020;38(suppl 15):8020. doi:10.1200/JCO.2020.38.15_suppl.8020
- Chong EA, Ahmadi T, Aqui NA, et al. Combination of lenalidomide and rituximab overcomes rituximab resistance in patients with indolent B-cell and mantle cell lymphomas. Clin Cancer Res. 2015;21(8):1835-1842. doi:10.1158/1078-0432.CCR-14-2221
Gasparetto Explains Rationale for Quadruplet Front Line in Transplant-Ineligible Myeloma
February 22nd 2025In a Community Case Forum in partnership with the North Carolina Oncology Association, Cristina Gasparetto, MD, discussed the CEPHEUS, IMROZ, and BENEFIT trials of treatment for transplant-ineligible newly diagnosed multiple myeloma.
Read More