Patient With Newly Diagnosed Multiple Myeloma Eligible for Multiple Triplet and Quadruplet Regimens
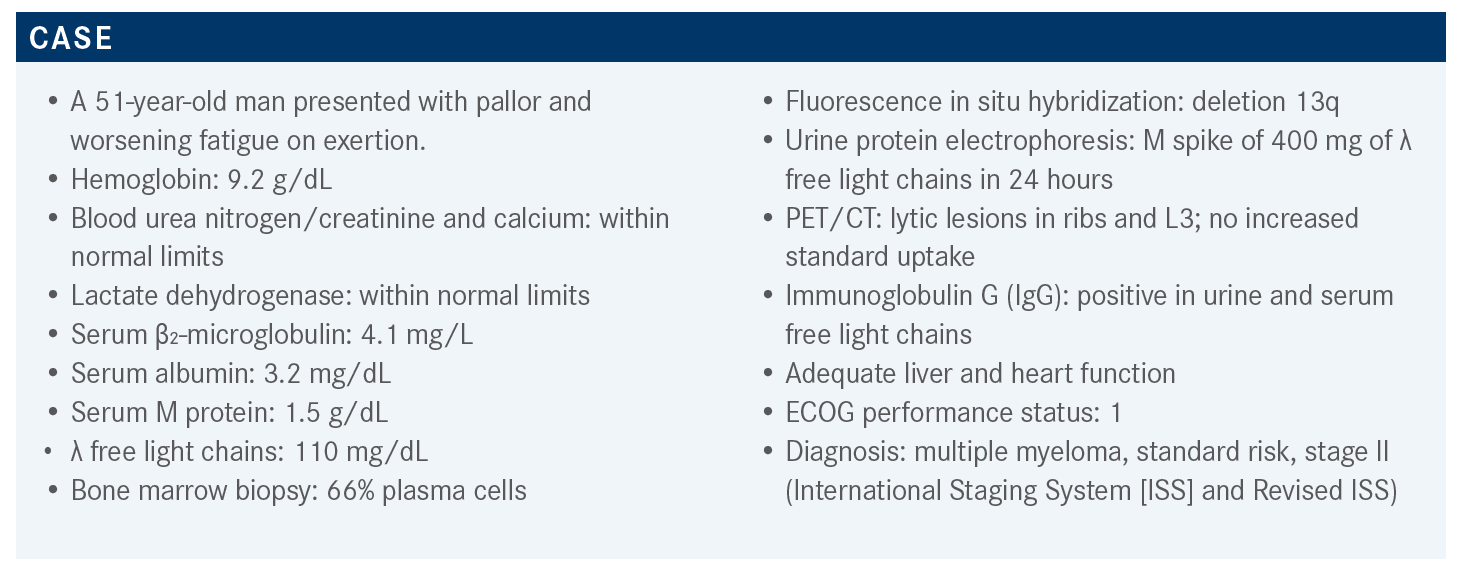
During a Targeted Oncology Case-Based Roundtable event, Noa Biran, MD, discussed the case of a 51-year-old man with newly-diagnosed multiple myeloma.
Noa Biran, MD

During a Targeted Oncology Case-Based Roundtable event, Noa Biran, MD, Hackensack Meridian Health, John Theurer Cancer Center at Hackensack University Medical Center, discussed the case of a 51-year-old man with newly-diagnosed multiple myeloma.
Targeted OncologyTM: What are the recommended regimens for a transplant-eligible patient with newly diagnosed multiple myeloma (NDMM)?
BIRAN: The NCCN [National Comprehensive Cancer Network] guidelines for upfront myeloma are confusing because the preferred regimen, [VRd—bortezomib (Velcade), lenalidomide (Revlimid), and dexamethasone], is listed as Category 1.1 Another preferred regimen is bortezomib, cyclophosphamide [Cytoxan], and dexamethasone [VCd]. VRd is generally a subcutaneous once-weekly dosing that is not based on phase 3 data but on phase 2 randomized trial data and retrospective data.
Other recommended regimens are carfilzomib [Kyprolis], lenalidomide, dexamethasone [KRd]; daratumumab [Darzalex] plus VRd [D-VRd]; and ixazomib [Ninlaro], lenalidomide, dexamethasone. Other regimens that are useful in certain circumstances include bortezomib, doxorubicin, dexamethasone, which is hardly used; carfilzomib, cyclophosphamide, dexamethasone; ixazomib, cyclophosphamide, dexamethasone; bortezomib, thalidomide [Thalomid], dexamethasone [VTd]; cyclophosphamide, lenalidomide, dexamethasone; daratumumab plus VCd; and daratumumab plus VTd. Daratumumab in upfront multiple myeloma can be used both as an infusion or injection.
What aspects of therapy are most important in the treatment of transplant-eligible patients with NDMM?
The most recent phase 3 randomized trial data using upfront regimens [in transplant-eligible patients can be compared using] median follow-up; stem cells mobilization; postconsolidation overall response rate; postconsolidation very good partial response [VGPR] rate, which is an important end point; postconsolidation stringent complete response [sCR]; median progression-free survival [PFS]; PFS hazard ratio; and minimal residual disease [MRD] negativity, which varies depending on whether it is done when patients have achieved a CR or VGPR or just a CR, hence there is a lot of variability in the MRD negativity across studies.
The IFM 2009 trial [NCT01191060] compared patients who had VRd plus transplant vs VRd alone. It had a long follow-up of 89.9 months, so with longer follow-up larger differences can be seen between the 2 arms because in myeloma they’re not progressing for years or decades. All the regimens [in the different trials] are robust.
The VGPR rates range from 69% with VRd all the way to 90.9% with the quadruplet D-VRd. The CASSIOPEIA study [NCT02541383], which compared D-VTd vs VTd, had a shorter median follow-up of 19 months and did not show a big difference in median PFS and VGPR rate compared with other studies.2
The IFM 2009 trial was a large international trial that looked at VRd for 3 cycles followed by stem cell collection and then VRd consolidation. The comparator arm [had patients undergo autologous stem cell transplant (ASCT)] then consolidation with VRd. Both arms [received] lenalidomide maintenance. The nontransplant arm had a diminished median PFS at both 44 months and 90 months of follow-up. At 90 months, median PFS was 35 months for the nontransplant arm vs 47.3 months for the transplant arm. Overall survival [OS] at 8 years was similar in both transplant and nontransplant patients. This could be because follow-up was not long enough. Standard-risk patients live more than a decade, so it is difficult to show OS benefit in patients with NDMM. That’s why the FDA is accepting surrogates such as MRD negativity and PFS for these trials.2,3 The subgroup analysis for PFS shows patients with standard cytogenic risk have a significant improvement in PFS for those in the transplant arm.
For the MRD status at the start of maintenance, the median PFS was not reached [among patients with MRD-negative status] and was 29 months [among patients with MRD-positive status]. Patients with MRD-positive, standard-risk status do worse than those with MRD-negative, high-risk status. Achieving MRD negativity is more important than having high-risk cytogenetics.3
How is MRD status defined and how is it done?
It is a bone marrow biopsy done by 10-color flow cytometry or by next-generation sequencing [NGS] where RNA or DNA is sequenced. The flow cytometry is very sensor dependent and must be done on the spot because the plasma cells are very fragile. There’s no standardization for flow.
There is a company that does NGS but it’s not approved by all insurances, at least in New Jersey. We don’t do it because No. 1, you have to send a diagnostic sample at time of diagnosis to this company, which we don’t always do; No. 2, we don’t want our patients getting billed. We prefer doing flow cytometry, which has a sensitivity of 10-5 and is a bone marrow aspirate.4
MRD is important for prognosis, but at this point is not treatment changing. We have no data to support changing treatment or stopping maintenance therapy if someone is MRD negative at 6 months post transplant or what to do if they are MRD positive. However, there are ongoing trials looking at that.4
Does it matter if patients who are high risk achieve an MRD-negative status?
Data from the Multiple Myeloma Research Foundation CoMMpass trial [NCT01454297] show that these patients with homozygous TP53 deletion can achieve MRD negativity, but it’s meaningless. This may be due to a sampling problem, patchy bone marrow in myeloma, or a mutant calmodulin not identified with MRD. There is a subset of high-risk patients who achieve MRD negativity and relapse immediately. So in high-risk patients, MRD negativity is not as relevant.5
What are standard-of-care regimens for the induction phase?
The FORTE study [NCT02203643] looked at 3 arms with carfilzomib, cyclophosphamide, dexamethasone [KCd] vs 12 cycles of KRd vs KRd followed by ASCT. Patients in all 3 arms [received mobilization of peripheral blood stem cells] after 4 cycles of chemotherapy.
The first analysis showed KCd was inferior in terms of PFS. The lenalidomide is a key part of the induction, and I try to get everybody in the upfront setting at least a few cycles of it. Even if not in the first cycle, because it takes a while until you get it, it’s important to incorporate it into a portion of the induction. All the patients in the 3 arms were randomized to either lenalidomide [R] maintenance or carfilzomib and lenalidomide [KR] maintenance.6
The median PFS rate in the KCd arm was 58%, KRd-ASCT was 78%, and 12 cycles of KRd without ASCT was 66%. There is improvement in median PFS [for the arms with lenalidomide]. That was supported in all the subgroups, including ISS II/III and high risk. We’re going to look at this high-risk subset in other trials.7
The high-risk subset is important because you have more events, so it’s like a quick readout, whereas in the standard risk it takes much longer for [patients] to progress or to die so it’s harder to show differences. If something applies in high risk, it should theoretically apply in the standard risk as well. I always pay attention to that part of the subgroup analysis in all these trials.
In the second randomization, 356 patients were randomized to maintenance therapy with KR vs R. The more treatment we give patients the better they’re going to do. The 3-year PFS rate from second randomization was 75% vs 66% [HR, 0.63; P = .026]. Most subgroups also showed an improvement with the doublet.7
Is the best treatment approach triplet or quadruplet therapy?
The CASSIOPEIA phase 3 trial looked at 1085 patients who were transplant-eligible, over 65 years old, and ECOG performance status 0 to 2. The primary end point was sCR and randomization was 1:1 with a triplet, VTd vs the quadruplet, D-VTd both for 4 cycles. [Patients in both arms were then] mobilized with cyclophosphamide and then went on to their respective consolidation therapies with D-VTd or VTd. A second randomization was done where patients were either [randomized to observation alone until progression of disease] or [had] daratumumab maintenance done every 8 weeks for 2 years [followed by observation until progression of disease].8
The primary end point of sCR was achieved. The rate of sCR was 29% with the quadruplet compared with 20% with the triplet [Odds ratio (OR), 1.60; 95% CI, 1.21-2.12; P ≤ .001]. The CR, VGPR, and MRD negativity were significantly higher in the quadruplet arm. MRD negativity is a surrogate end point for duration of response [DOR]. If a higher rate of MRD negativity is achieved, there will be a longer DOR. The sCR in the quadruplet arm was favored across all subgroups except in high-risk patients.8
There is increase of sCR after induction, after ASCT, 100 days after ASCT, and then at best response. MRD negativity rate after ASCT using NGS, which is the more sensitive test, was 57% vs 37%, and with flow cytometry it was 64% vs 44% in the quadruplet vs triplet therapy, respectively. This translates into an improvement in PFS in the D-VTd arm.8 Usually what we see is the more drugs, the better the outcome, but we always consider the cost and high-risk cytogenetics.
The GRIFFIN trial [NCT02874742] was a phase 2 randomized study of D-VRd vs VRd in transplant-eligible patients with NDMM. The median age of these patients was 60 years. The median ages for the previous 2 trials were 64 and 65 years, which is a slightly [older] population. Of these, 15% had high-risk status, which was a bit less than what we see in other studies. In the general population we see 25% with high-risk cytogenetic status. Those with ISS stage III were 14%. There was a significantly lower rate of ASCT in the VRd arm due to early discontinuation, which I assume was related to neuropathy.9
Randomization was in a 1:1 fashion with D-VRd vs VRd for 4 induction cycles. In the D-VRd arm, 90% of patients had ASCT and 76% in the VRd arm had ASCT. Patients in both arms were mobilized before that and then had 2 additional consolidation cycles with either D-VRd or VRd followed by maintenance. Patients in the D-VRd arm went on to [daratumumab]-R maintenance for up to 32 cycles, and then the VRd arm went on to R maintenance. The primary end point was sCR.9
As a reminder, sCR means biochemical remission plus bone marrow with less than 5% plasmacytosis. You must confirm with bone marrow to achieve sCR.They also looked at MRD, CR, overall response rate, and VGPR as secondary end points.
The responses were significantly better in the D-VRd arm. The sCR rate deepened after induction at 12.1 months vs 7.2 months, and by the end of the 12 months of maintenance cutoff you have 63.6 months vs 47.4 months for the D-VRd vs VRd arms, respectively. Median follow-up was 13.5 months, which really isn’t a long time, and the cutoff for the median follow-up at 12 months of maintenance therapy was 27.4 months. So we have a deepening of response over time and a significantly deeper response with D-VRd.10
For the subgroup analyses, D-VRd improved sCR and MRD negativity across most subgroups. MRD negativity rates were better in the quadruplet arm at 62.5% vs 27.2% for the triplet arm. MRD negativity is a surrogate for PFS and most subgroups favored the quadruplet, except for ISS III, non-IgG, which tend to be sometimes higher risk, and high-risk cytogenetic status where there is not much benefit. Again, it’s harder to show a benefit in the high-risk group, but 4 drugs were used, and they didn’t benefit as much from the addition of daratumumab based on sCR and MRD negativity.9
For PFS, median follow-up was more than 40 months, which is a good follow-up time. The [patients taking] D-VRd had significantly better PFS. At 36 months, 94.5% of patients had not yet progressed. Most [patients were] still alive using a median follow-up of 40 months, and the difference was not big for the 2 arms.9
Most quadruplets are better than triplets. The recent data for elotuzumab [Empliciti]-VRd showed that it is not better than VRd, but for the most part, more drugs are going to translate into better response and longer DOR.11
We must consider infections and cytopenias, especially in the COVID-19 era. Comparing VRd with D-VRd showed that thrombocytopenia grade 3 doubled, grade 3 or 4 neutropenia doubled, leukopenia was 6.9% vs 16.2%, anemia was 5.9% vs 9.1%, and lymphopenia was 21% vs 23%.9,10 Interestingly, despite more hematologic toxicity, you had more dropouts in the VRd arm compared with the D-VRd arm.
Grade 3 or 4 fatigue, upper respiratory tract infections, constipation, and nausea [made] no big difference in the D-VRd and VRd arms. Infusion reactions are more with the D-VRd. There is more grade 1 and 2 peripheral neuropathy with VRd at 74% vs 59%, but grades 3 and 4 were similar for both arms. Interestingly, the addition of daratumumab doesn’t add more peripheral neuropathy.9,10
Gasparetto Explains Rationale for Quadruplet Front Line in Transplant-Ineligible Myeloma
February 22nd 2025In a Community Case Forum in partnership with the North Carolina Oncology Association, Cristina Gasparetto, MD, discussed the CEPHEUS, IMROZ, and BENEFIT trials of treatment for transplant-ineligible newly diagnosed multiple myeloma.
Read More
Key Trials From ASH 2024 Impact Treatment for Plasma Cell Disorders Going Forward
February 20th 2025Peers & Perspectives in Oncology editorial board member Marc J. Braunstein, MD, PhD, FACP, discussed the significant advancements in multiple myeloma treatment at the 2024 ASH Annual Meeting and Exposition.
Read More