Assessing and Monitoring Manifestations of Chronic GVHD
Catherine J. Lee, MD, MS, associate professor of medicine in the Clinical Research Division at Fred Hutchinson Cancer Center in Seattle, Washington, led a live virtual discussion on how to treat patients with chronic graft-vs-host disease (GVHD) and how best to assess the extent of their disease.
Catherine J. Lee, MD, MS
Associate Professor of Medicine
Clinical Research Division
Fred Hutchinson Cancer Center
Seattle, WA

Catherine J. Lee, MD, MS, associate professor of medicine in the Clinical Research Division at Fred Hutchinson Cancer Center in Seattle, Washington, led a live virtual discussion on how to treat patients with chronic graft-vs-host disease(GVHD) and how best to assess the extent of their disease. Moreover, she discussed treatment options beyond the first-line setting, highlighting the case of a 48-year-old man who underwent myeloablative conditioning.
With the help of matched sibling and unrelated donors, the patient had an allogeneic hematopoietic cell transplant for acute myeloid leukemia, with tacrolimus and methotrexate as GVHD prophylaxis. He returned at 6 months for a posttransplant visit. He had normal blood counts but presented with skin changes, with hyperpigmentation and approximately half of each arm showing lichen planus. He also had superficial sclerotic features (skin could be pinched) on his lower trunk and lower extremities.
Frontline Treatments in Chronic GVHD
Catherine J. Lee, MD, MS: Patients [with diagnosed] moderate or severe chronic GVHD are candidates for systemic therapy. According to the National Comprehensive Cancer Network guidelines, enrollment in a well-designed clinical trial for all patients presenting with chronic GVHD is highly encouraged.1 For patients who just have mild chronic GVHD, one could consider just using local therapies. So for someone who has a mild severity of skin GVHD, one might consider using topical steroids; or for mild oral GVHD, one would consider using local treatments such as dexamethasone or clobetasol mouth rinses.
For patients with moderate to severe chronic GVHD who warrant systemic therapy, options for first-line therapy include restarting, continuing, or escalating the original immunosuppressive agent, but administering systemic corticosteroids at doses of 0.5 to 1 mg/kg per day of prednisone dose equivalent. The initial corticosteroid dose may vary depending on the organs involved, the severity of the chronic GVHD, and patient comorbidities. Usually, I think most providers would start at least at 0.5 mg/kg, but 1 mg/kg per day is common.
I have not heard of many providers using 2 mg/kg per day as is used in [patients with] acute GVHD.2 In addition to systemic therapy, one could consider including topical therapy, such as steroid ointments, topical estrogen for [women] who have vulvovaginal chronic GVHD, topical tacrolimus, or dexamethasone rinses. For patients with lung involvement in addition to steroid use, they should probably be started on fluticasone, azithromycin, montelukast [FAM] therapy.
Some institutions have removed the azithromycin from this regimen as there have been recent publications indicating that azithromycin may be associated with new malignancies.3 Some places, like my institution, will start azithromycin and then after 6 months remove it from the FAM therapy. But for the past 40 years, corticosteroids have been the mainstay of treatment in first-line therapy [for patients with chronic GVHD]. Response rates are about 50%, with greater than half of patients requiring second-line therapy within 2 years. Unfortunately, as many of you know, corticosteroids are associated with significant toxicities, including infection, muscle weakness, bone loss, avascular necrosis, [and] lots of late effects.4
Steps to Diagnose and Stage Chronic GVHD
Lee: The revised 2014 National Institutes of Health [NIH] criteria have brought the consistency that was very much needed to help standardize diagnosis and staging.5 Clinical features of GVHD determine whether the clinical syndrome is considered acute or chronic. It’s not the temporal relationship to transplantation [as in] the way we used to diagnose chronic GVHD. [Previously], any [case of] GVHD that was thought to occur before day 100 was considered acute GVHD, and any signs or symptoms that developed after day 100 were labeled as chronic GVHD. That is not the way that chronic GVHD is diagnosed in the modern era, as it’s based on the manifestations [of the disease].
Chronic GVHD has been standardized and validated for outcome assessments. Findings are typically classified as diagnostic signs. Thera are any manifestations that are considered as sufficient to establish a diagnosis of chronic GVHD without needing any biopsy or histologic diagnosis.6 Then there are distinctive signs, which are signs that can be seen in chronic GVHD but are not sufficient to establish the diagnosis and require histologic diagnosis to support the clinical findings, [which would be given an NIH score of 3].
Treatments After Steroids
Lee: For that half of the patients who don’t respond to first-line systemic corticosteroids, therapeutic options for steroid-refractory chronic GVHD again include enrollment in a well-designed clinical trial. Several systemic therapies are available, many of them being used off label, but there are now 3 with FDA-approved indications for the treatment of steroid-refractory chronic GVHD, including ruxolitinib [Jakafi], which is category 1; belumosudil [Rezurock]; and ibrutinib [Imbruvica].7
Ibrutinib was designed as a selective and irreversible inhibitor with a Bruton tyrosine kinase protein. It blocks B-cell receptor signaling and activation of B cells, which we know…can be pathogenic in chronic GVHD and produce anti–host reactive antibodies.8 Ibrutinib blocks B-cell survival, proliferation, and autoantibody production, but it also blocks T-cell activation in downstream cytokine production via its inhibitory effect, otherwise known as IL-2 inducible T-cell kinase.
In comparison, belumosudil is a selective Rho-associated coil to coil kinase-2 inhibitor. The ROCK2 pathway normally upregulates a T helper 17 and T follicular helper cell through interaction and phosphorylation of STAT3, which leads to the upregulation of proinflammatory cytokines.9 Inhibition of ROCK2 thereby downregulates these proinflammatory pathways. Belumosudil also blocks the inhibitory effect of ROCK2 on STAT5 activation, causing increased phosphorylation and upregulation of T-regulatory cells that are also involved in reducing inflammation. ROCK2 pathway is also involved in multiple profibrotic processes, so when it’s activated it leads to transcription of profibrotic genes. Inhibition of ROCK2 decreases the deposition of collagen fibers, stress fiber formation, and other mediators of fibrosis.
Finally, ruxolitinib is a JAK1 and JAK2 inhibitor that suppresses T-cell activation by interfering with cytokine receptor–mediated signaling from a variety of proinflammatory cytokines. This affects downstream proliferation of effector T cells, thereby decreasing tissue damage and fibrosis. This impairs function of dendritic cells, which results in decreased alloreactive T-cell activation while also increasing T-regulatory cells…. Moreover, the [manufacturer] has been interested in JAK1 inhibitors because these JAK inhibitors don’t have any association with cytopenias.10
Assessing and Monitoring Chronic GVHD
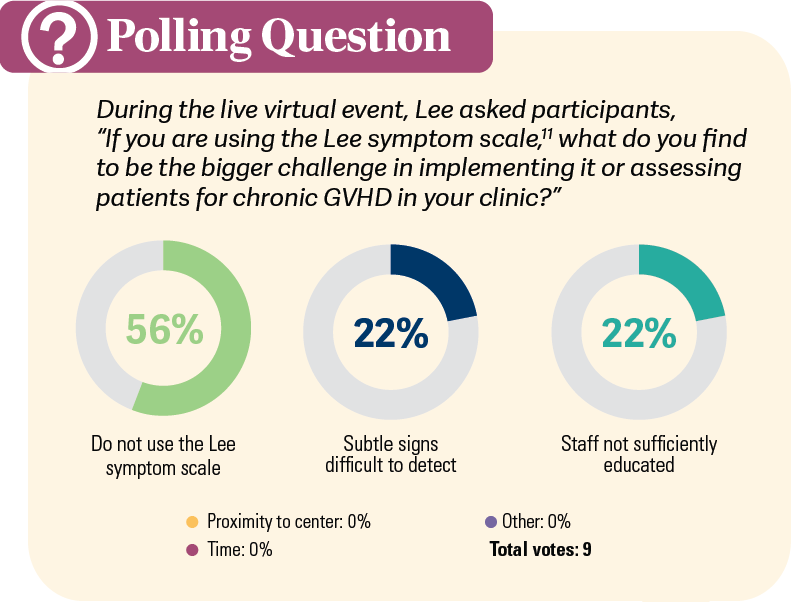
LEE: We give our patients a paper format of the Lee symptom scale, and then our staff will input their answers… Sometimes patients do have questions about exactly how they should answer, and having a better education for staff to be able to answer their questions could be very helpful [POLL].11 However, it presents its own challenges to use in some clinics.
[When monitoring these patients], each institution has [its] own methods. At my old institution, which was the University of Utah, each primary physician’s team would manage the patient all the way from pretransplant throughout the rest of their life. The primary attending [physician] would be very heavily involved in the first year. The first 3 months, they’re seen frequently, and then after the day 100 workup, if everything looks great, the patient’s allowed to go back to their local home. Then they follow up approximately about once a month all the way up to month 12 during their immunosuppressive taper and to make sure they’re not developing any GVHD.
After the 1-year mark, if there’s no evidence of relapse, and if they’re still doing well off their immune suppression, we bring them back in about every 3 months so that they can get their posttransplant immunizations, as well as get a GVHD assessment to talk about survivorship issues with our physician assistants. At every visit, we educate our patients thoroughly on symptoms and signs of chronic GVHD and, of course, I’m always a little bit more particular [with] my patients who might have experienced acute GVHD, who may have received total body irradiation, are ablative, or who might have had an unrelated donor or mismatched type of transplant. Those are some of the risk factors that enhance my radar for chronic GVHD.
In this case, you would give [the patient] a score 2 for that superficial sclerotic feature. Then you could check off anything else that applies to this patient like hyperpigmentation, or maybe some pruritis if [it’s observable]. Overall, we would diagnose him with an overall severity of moderate because he has an organ score of 2 in the skin. You now start thinking about first-line treatment approaches. As I mentioned before, if [a patient such as this] was just considered to have mild chronic GVHD, the recommendations are not necessary to start systemic therapy for mild chronic GVHD, but for moderate to severe GVHD, the recommendations are to start systemic therapy with corticosteroids from 0.5 to 1 mg/kg per day.1
Then we would wait for a response [to the steroids]. You might [give this patient] antimicrobials for prophylaxis while [he is receiving] steroids, including mold prophylaxis. Likely that patient is still [receiving] acyclovir, so you might consider adding penicillin for encapsulated bacteria prophylaxis. Then recommend supportive care or ancillary therapies [for a patient such as this include] stretching exercises, physical therapy, and maybe some topical therapies for the skin.
References
1 .NCCN. Clinical Practice Guidelines in Oncology. Hematopoietic cell transplant (HCT), version 1.2023. Accessed June 27, 2023. https://bit.ly/3m0dGPh
2. Mielcarek M, Storer BE, Boeckh M, et al. Initial therapy of acute graft-versus-host disease with low-dose prednisone does not compromise patient outcomes. Blood. 2009;113(13):2888-2894. doi:10.1182/blood-2008-07-168401
3. Vallet N, Le Grand S, Bondeelle L, et al. Azithromycin promotes relapse by disrupting immune and metabolic networks after allogeneic stem cell transplantation. Blood. 2022;140(23):2500-2513. doi:10.1182/blood.2022016926
4. Velickovic VM, McIlwaine E, Zhang R, Spelman T. Adverse events in second- and third-line treatments for acute and chronic graft-versus-host disease: systematic review. Ther Adv Hematol. 2020;11:2040620720977039. doi:10.1177/2040620720977039
5. Jagasia MH, Greinix HT, Arora M, et al. National Institutes of Health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. The 2014 Diagnosis and Staging Working Group report. Biol Blood Marrow Transplant. 2015;21(3):389-401.e1. doi:10.1016/j.bbmt.2014.12.001
6. Flowers ME, Martin PJ. How we treat chronic graft-versus-host disease. Blood. 2015;125(4):606-615. doi:10.1182/blood-2014-08-551994
7. Zeiser R, Lee SJ. Three US Food and Drug Administration-approved therapies for chronic GVHD. Blood. 2022;139(11):1642-1645. doi:10.1182/blood.2021014448
8. Zeiser R, Sarantopoulos S, Blazar BR. B-cell targeting in chronic graft-versus-host disease. Blood. 2018;131(13):1399-1405. doi:10.1182/blood-2017-11-784017
9. Cutler C, Lee SJ, Arai S, et al. Belumosudil for chronic graft-versus-host disease after 2 or more prior lines of therapy: the ROCKstar Study. Blood. 2021;138(22):2278-2289. doi:10.1182/blood.2021012021
10. Schwartz DM, Kanno Y, Villarino A,Ward M, Gadina M, O’Shea JJ. JAK inhibition as a therapeutic strategy for immune and inflammatory diseases. Nat Rev Drug Discov. 2017;17(1):78. doi:10.1038/nrd.2017.267
11. Teh C, Onstad L, Lee SJ. Reliability and validity of the modified 7-Day Lee Chronic Graft-versus-Host Disease Symptom Scale. Biol Blood Marrow Transplant. 2020;26(3):562-567. doi:10.1016/j.bbmt.2019.11.020
Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More