Roundtable Roundup: Skin Cancer
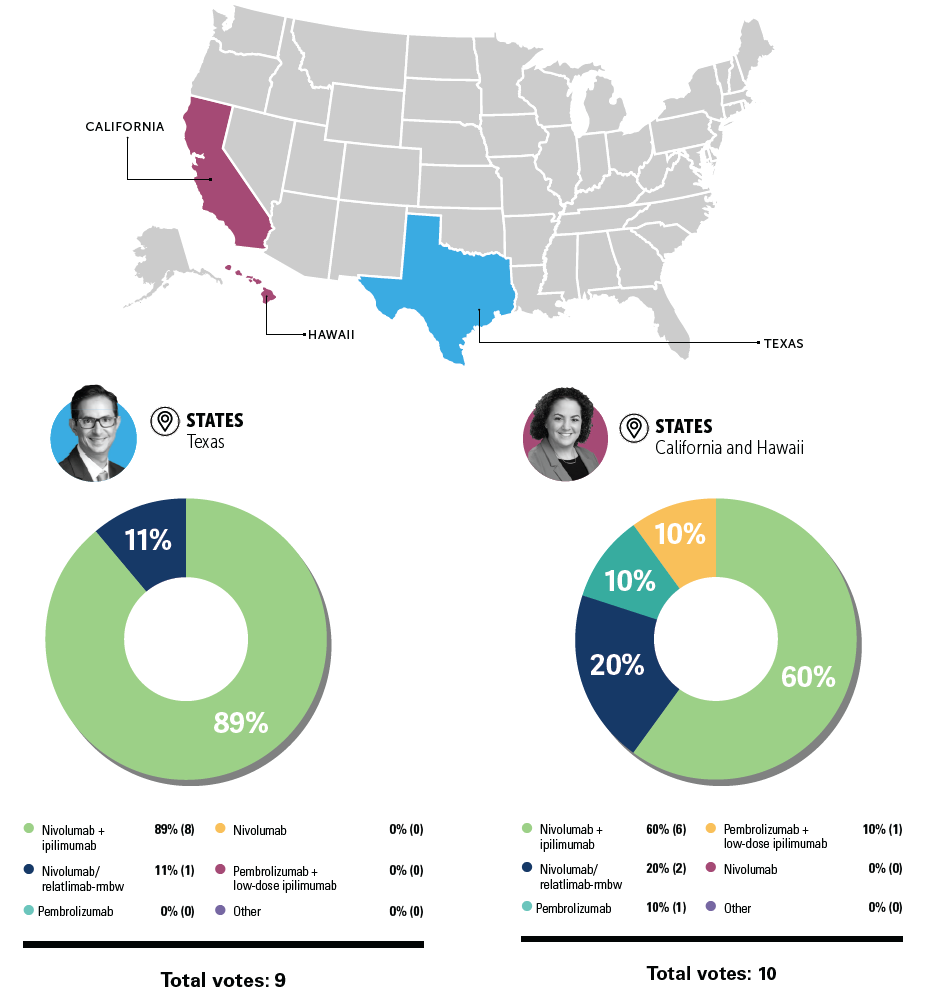
In separate live, virtual events, Hussein A. Tawbi, MD, PhD; and Allison Betof Warner, MD, PhD, discuss potential treatment options for a patient with BRAF mutation–negative melanoma.
Case Summary
- A 78-year-old man had a history of stage III melanoma.
- Patient underwent surgical resection 12 years prior.
- Lymph node dissection was positive for nodal involvement.
- Patient declined complete lymph node dissection and adjuvant systemic therapy.
- Patient remained active since his surgery and maintained regular follow-up.
- On routine follow-up, the patient presented with moderate asthenia that limited his daily activities, without other relevant clinical symptoms.
- ECOG performance status: 1
- Physical examination was unremarkable.
- Notable laboratory findings: lactate dehydrogenase (LDH) level of 380 IU/L (reference range, 110-240 IU/L)
- A full-body CT scan revealed the presence of pulmonary and hepatic nodules but no evidence of brain metastases.
- The patient underwent a core-needle biopsy of the largest hepatic lesion in segment IVb without any complications.
- Pathology revealed metastatic melanoma.
- Mutation testing was BRAF negative.
Hussein A. Tawbi,
MD, PhD
Professor
Deputy Chair
Director, Personalized Cancer Therapy
Department of Melanoma Medical Oncology
Division of Cancer Medicine
The University of Texas
MD Anderson Cancer Center
Houston, TX

TAWBI:The decision-making here was reasonable and appropriate. Either of those regimens technically would be appropriate for this patient. I would probably say the patient’s high LDH is the biggest [factor]. I also recognize that as you start using a new combination more consistently…people’s perception of the combination changes as they became more familiar with it.
In the National Comprehensive Cancer Network [NCCN] guidelines, they list nivolumab and relatlimab-rmbw [Opdualag] as a preferred regimen.1 They only added category 1 recently. I was [surprised] at the NCCN not adding category 1 evidence from the get-go because the randomized, phase 2/3, blind, independent review study [RELATIVITY-047; NCT03470922] hit its primary end point.2
That to me made it a category 1 regimen, so I’m happy [the NCCN recognizes] this is category 1 evidence. In the NCCN guidelines, you can technically choose any of those combination regimens or single-agent PD-1 inhibitors; that’s the current recommendation.
The low-dose ipilimumab [Yervoy]/pembrolizumab [Keytruda] was mentioned there. I’d be very careful because there have never been randomized studies for low-dose ipilimumab/pembrolizumab, and there's only been 1 nonrandomized phase 2 trial.
Allison Betof Warner,
MD, PhD
Assistant Professor, Department of Medicine
Director, Melanoma Medical Oncology
Director, Solid Tumor Cellular Therapy
Codirector, Pigmented Lesion
and Melanoma Program
Stanford Cancer Center
Palo Alto, CA

WARNER: The way I think about this, when I talk about this with my patients, is we now have 3 options. We have single-agent PD-1 inhibitors, we have nivolumab/relatlimab, and then we have ipilimumab plus nivolumab [Opdivo]. I don’t give a ton of low-dose ipilimumab plus PD-1 anymore because we have nivolumab/relatlimab, but that’s also a fourth option.
There’s a spectrum of increased response rates, but that correlates exactly with an increased rate of toxicity. So I think treatment is highly dependent on what your patient can tolerate and is willing to tolerate. I think there are times [when] it’s the wrong decision to give combination—[for example], in frail patients, [very old patients], someone who has a history of autoimmune disease, those types of things. I do think if they have low disease burden in not a dangerous place in their body that it’s probably the wrong decision to give them full-dose ipilimumab/nivolumab. But could you be faulted for doing it? No, it just wouldn’t be my clinical decision in that situation.
"What first-line therapy are you most likely to recommend for this patient with metastatic melanoma with no BRAF-activating mutation?"
REFERENCES:
NCCN. Clinical Practice Guidelines in Oncology. Melanoma: cutaneous, version 2.2023. Accessed June 19, 2023. https://bit.ly/3NivRJS
Tawbi HA, Schadendorf D, Lipson EJ, et al; RELATIVITY-047 Investigators. Relatlimab and nivolumab versus nivolumab in untreated advanced melanoma. N Engl J Med. 2022;386(1):24-34. doi:10.1056/NEJMoa2109970