Roundtable Discussion: Defining How the JAVELIN Trial Changes Practice in Metastatic Bladder Cancer
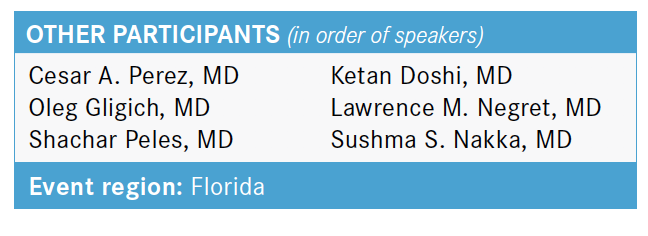
During a Targeted Oncology Case-Based Roundtable event, Daniel A. Landau, MD, moderated a discussion around the JAVELIN trial and how its results were practice changing for oncologists treating for bladder cancer.
Daniel A. Landau, MD

During a Targeted Oncology Case-Based Roundtable event, Daniel A. Landau, MD of the Medical Oncology/Hematology Department at Orlando Health Cancer Institute in Orlando, FL. moderated a discussion around the JAVELIN trial and how its results were practice changing for oncologists treating for bladder cancer.
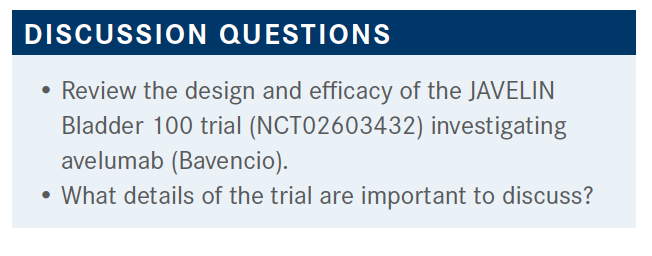
LANDAU: [Enrolled patients] had a urothelial malignancy that was either locally advanced or metastatic and had a complete response [CR], partial response [PR], or stable disease with first-line platinum-containing chemotherapy, which included carboplatin.1 They had 4 to 6 cycles of treatment; if they did not progress, then [they] went on to avelumab pretty quickly after the scans that showed the stability or response. The primary end point was overall survival [OS], but there were a number of other end points that were looked at. This was not a crossover design study. The avelumab dose was 10 mg/kg every other week [with best supportive care (BSC)] versus BSC alone.
When defining PD-L1, it was not just any PD-L1 positivity; it had to be greater than 25%, which is a little on the high side. But it seems as [though] both groups responded.
If patients have some response or stability and go on to avelumab, they are going to do better than if they go on to BSC alone. The split [in Kaplan-Meier curves] occurs early on and is maintained. Median OS was about 21.5 months vs 14 months [HR, 0.69; 95% CI, 0.56-0.86; P < .001].
In terms of the other outcomes, did they get substantially more response with addition of the avelumab? If [the patient was positive for] PD-L1, they were more likely to bump up into a CR. But, for the most part, patients maintained stability that translated to the OS difference. There wasn’t a ton of objective response. More with PD-L1, but across the board [it was stable disease].
Every one of the [subgroups favored avelumab]. You always have to be careful [with analyses because] a number of the subgroups are not going to be adequately represented to draw broad conclusions. But you can at least see that it appears that cisplatin versus carboplatin still benefits with early avelumab; whether it was a CR, PR, or stable disease, the benefits were very similar. Creatinine clearance did not make a big difference. PD-L1 [subgroups had a better hazard ratio] for positivity…but overall it appears there is benefit, regardless of the PD-L1 expression [positive PD-L1 HR, 0.56; negative PD-L1 HR, 0.86].
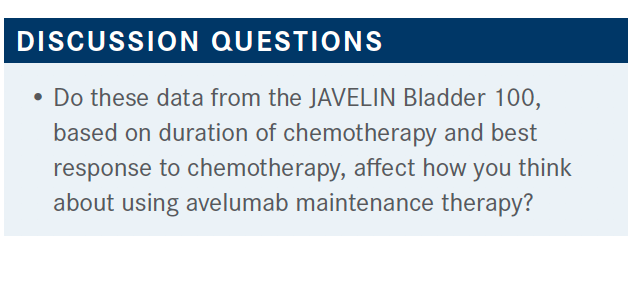
PEREZ: Regarding the PD-L1, I like to have…the information. If somebody [is on] chemotherapy, has a response, and [is] PD-L1 negative, then maybe you want to go to 6 cycles. But if patients are struggling with chemotherapy, and they are PD-L1 positive, then maybe you want to cut chemotherapy short and switch them to maintenance earlier. So I think it’s good to have the information, the PD-L1 status, knowing that the chance of a patient having a benefit is probably more if they are positive.
LANDAU: Yes, that’s a great point. The studies weren’t stratified that way; it would be very difficult to do that. But your logic does make sense, that you did see more [benefit] in the subgroup with PD-L1 positivity, so maybe you want to slant toward the avelumab a bit earlier in that setting. It stands to reason. I think where my issue comes in is that I have so much trouble getting [patients] through 6 cycles of platinum therapy, regardless, that sometimes the decision’s made for me.
PEREZ: I agree, definitely.
LANDAU: Looking at the visceral disease [liver lesions, and lung lesions], [I found that] liver lesions…was the most in the middle [of decidiing between favoring avelumab vs BSC alone]. Lung lesions were also a bit slanted [toward BSC alone], but I think most of this stands to reason for what we expect.
For the patient flow, [patients first received] chemotherapy based on response, then went on to avelumab plus BSC or BSC alone….There were a couple of patients who went on to different PD-L1 inhibitors [6.3% after avelumab vs 43.7% after BSC alone]. [Some received] FGFR inhibitors [2.6% vs 2.3%]; a very small segment of the population [have FGFR mutations], but sometimes you do catch that patient. A lot of patients did not receive any subsequent drug therapy. Nearly one-third of patients received no subsequent drug therapy [33.4% vs 30.9%].
That caught my attention, and I’m curious what everybody else’s opinion on this is. We didn’t have the Nectin-4 inhibitor available at the time, but to me that seems like a very high number of patients [who] did not go on to subsequent drug therapy. I think the other take-home is [that] this was not a crossover study, so patients were on BSC, eventually progressed, and most of them went on to a PD-L1 inhibitor at a certain point. Does that skew the data, knowing that they eventually went on to PD-L1 inhibitors? Anybody want to offer a thought about that?
GLIGICH: It definitely makes the data look so much better.
LANDAU: To me, what I think this answered is the timing of therapy. Because you always have the PD-L1 inhibitor in your back pocket, but it appears that, for the patients in this population, there was more benefit by early initiation— continuing that maintenance, rather than waiting for there to have been some kind of progression and then going on to the PD-L1 inhibitor. It makes sense that you’re extending the duration of treatment rather than delaying treatment and waiting for something to happen.
PELES: I’m going to play devil’s advocate, and I’m going to say you could also make the argument that in one-third or so of patients you were comparing 1 line of therapy to 2 lines of therapy.
LANDAU: It’s a very valid point. The FDA has approved avelumab for urothelial carcinoma maintenance therapy.2 This is now in the National Comprehensive Cancer Network for both platinum-eligible and platinum-ineligible patients.3 Even if you look at the preferred regimen, gemcitabine and carboplatin, gemcitabine and cisplatin, or even dose-dense [methotrexate, vinblastine, doxorubicin, and cisplatin] all followed by avelumab is a category 1 recommendation. So, there’s agreement that this is what we should be offering these patients.
The duration of first-line treatment—we don’t think it made a big difference; we think that the benefit was seen across the board, even with fewer cycles [of chemotherapy]. 4 [Regarding] the CR or PR versus stable disease, the more treatments you’re able to get into a patient, the more likely they are to have at least a PR. But there are benefits both ways. The PD-L1 positivity/negativity was reported, which, to me, always looked kind of high; it looked [as though] there were more PD-L1 positive patients than I would have expected for this population, but it’s hundreds of patients and it’s just the way it worked out.
In the post hoc analysis, does the duration or number of cycles make a difference prior to going on to the maintenance therapy? The answer is probably not. You tend to see the benefit whether it was 4 cycles, 5 cycles, 6 cycles. For the timing of therapy, as long as they went on within that 4- to 10-week time span, there was benefit across the board.
LANDAU: Are these new data [to you]? Do you think that this is a game changer?
DOSHI: I didn’t remember the data. I knew about the FDA approval, but lately I haven’t had metastatic [bladder cases]. I had whole bunch of neoadjuvant patients, but I haven’t had anybody with metastatic cancer, so I haven’t used it yet.
NEGRET: I’ve been incorporating it into my practice, and patients are asking about immunotherapy. They come in, they ask about immunotherapy, they like the idea of being put on what they see as a short course of chemotherapy. [They think], “I only have to do 3 months of it and then I get to be on this immunotherapy.” So I think most patients are for it, and I pretty much offer it to most of my patients.
LANDAU: Are you using the avelumab indefinitely or using it for a predetermined amount of time?
NEGRET: [I use it until] progression, mostly.
LANDAU: Yes, I’m doing the same thing, but I do hear some physicians off-protocol, saying, “I like to stop it after a year; I like to stop it after 2 years.” I don’t think we have those data in urothelial cancer, but I do hear that from time to time.
PEREZ: [Sometimes] I see a patient who had platinum chemotherapy first, and then when the next-generation sequencing comes back, they have an FGFR mutation. When you finish the chemotherapy, if PD-L1 is positive, what exactly do you do? These patients were included in the trial, but are you going to put them on an FGFR inhibitor? In lung cancer, it’s very straightforward, you put them on the inhibitor. But are you doing it the same way here [as we are with lung cancer]?
LANDAU: In my practice, no. I’ll use the maintenance PD-L1 inhibitor the way we’re discussing it here. I have used the FGFR inhibitors in urothelial cancer. They’re not benign; they have a fair adverse event profile. I’ve also not had a lot of patients who’ve had long-term responses, or very deep responses, to FGFR inhibition. I’m not sure if anybody has had a different experience, but my experience has not been that those are going to be a better option than PD-L1 inhibition.
NAKKA: Are you routinely checking PD-L1 in these patients up front? How are you using the PD-L1 information?
LANDAU: I don’t use it for early decision-making. There was the point earlier about maybe using it to determine how many cycles of chemotherapy you were going to offer, or should you go on to maintenance a bit earlier. In my practice, I’ve not been doing that a lot because I’m offering this maintenance to everybody who’s a candidate for it. I tend to do the testing more when I’m looking beyond the immunotherapies, when I’m looking at the FGFR inhibitors or maybe the Nectin-4 inhibitor. For the Nectin-4, you don’t\ need to do any testing in advance, but that’s around the time that I start doing it.
NAKKA: Was PD-L1 checked in this JAVELIN trial, and how did that affect [outcomes]?
LANDAU: The objective responses were more with a PD-L1 positive, but there’s benefit in the folks who were negative as well.
NEGRET: I think you also have to remember, as you mentioned earlier, they defined PD-L1 negative as less than 25%. If [a patient has PD-L1 expression] at 10%, in other studies we’d consider those [patients to be] positive, and so maybe that’s why you’re seeing some more benefit in these patients who are PD-L1 negative.
LANDAU: I thought that was a very ambitious number when I saw that they went for 25%. Are there any particular cons to the use of immunotherapy in this setting?
PEREZ: I think the way many [clinicians] were already using immunotherapy after the patient got a couple of cycles, [it was what] we call second line so it will be approved by the insurance. That’s just my thought.
LANDAU: I agree. I treated several patients off-protocol for whatever reason. There was some reason that they didn’t fit the protocol definition, and these were patients you’re worried about. You know that they’re going to have early relapse, so you want to do something. I think I did the same thing and treated patients off-protocol, but I mirrored the study design. I have patients who are going years strong with that, so it can work very well.
REFERENCES:
1. Powles T, Park SH, Voog E, et al. Avelumab maintenance therapy for advanced or metastatic urothelial carcinoma. N Engl J Med. 2020;383(13):1218-1230. doi:10.1056/NEJMoa2002788
2. FDA approves avelumab for urothelial carcinoma maintenance treatment. News release. FDA. June 30, 2020. Accessed May 19, 2021. https://bit.ly/3jaforD
3. NCCN. Clinical Practice Guidelines in Oncology. Bladder cancer, version 3.2021. Accessed May 19, 2021. https://bit.ly/3lold5s
4. Loriot Y, Powles T, Durán MAC, et al. Avelumab (Ave) first-line (1L) maintenance plus best supportive care (BSC) versus BSC alone for advanced urothelial carcinoma (UC): JAVELIN Bladder 100 subgroup analysis based on duration and cycles of 1L chemotherapy. J Clin Oncol. 2021;39(suppl 6):438. doi:10.1200/JCO.2021.39.6_suppl.438
Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More