Multiple Agents Prove Useful in RET-Mutated Thyroid Cancer
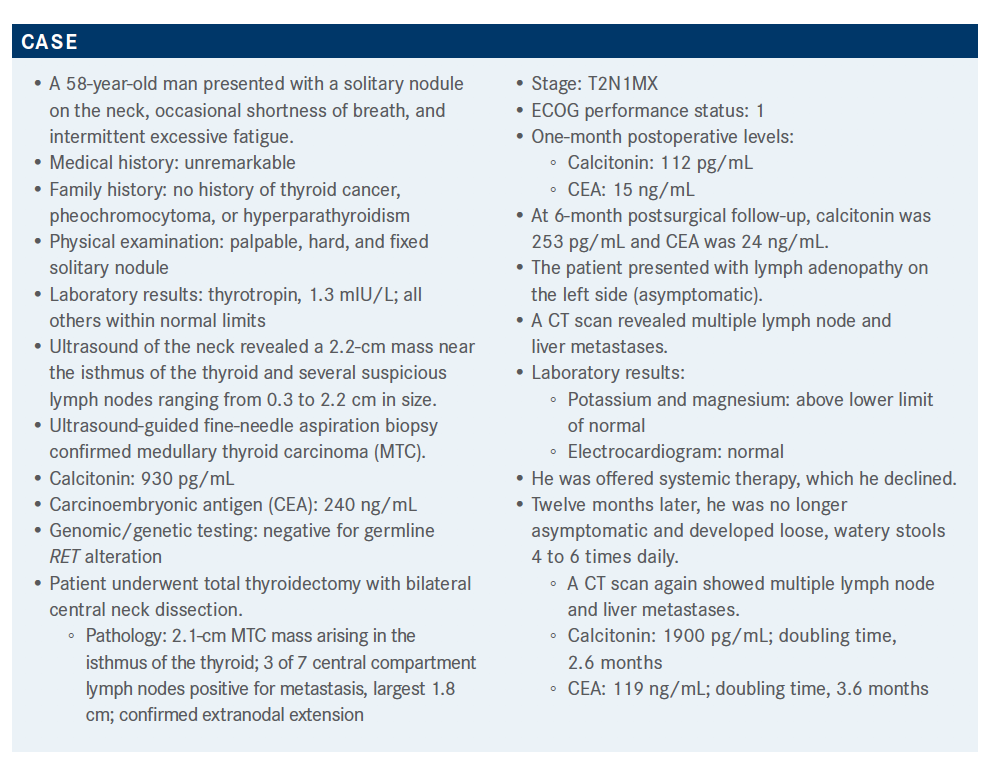
Many options are available for the treatment of RET-mutated thyroid cancer. During a Targeted Oncology Case-Based Roundtable event, Francis Paul Worden, MD, discussed the case of a 58-year-old patients who first presented with solitary nodule on the neck, occasional shortness of breath, and intermittent excessive fatigue.
Francis Paul Worden, MD
Many options are available for the treatment of RET-mutated thyroid cancer. During a Targeted Oncology Case-Based Roundtable event, Francis Paul Worden, MD, discussed the case of a 58-year-old patients who first presented with solitary nodule on the neck, occasional shortness of breath, and intermittent excessive fatigue.
Targeted OncologyTM: What are the available systemic treatment options for a patient with recurrent or persistent thyroid cancer with distant metastases?
WORDEN: According to current NCCN [National Comprehensive Cancer Network] guidelines, for asymptomatic [patients—unlike the patient we are considering here]—consider disease monitoring.1 I think that’s important. We know some of the multikinase inhibitors are quite toxic. So for someone who is asymptomatic with a low disease burden, there’s nothing wrong with monitoring them closely. There’s an online calculator for calcitonin doubling time, which you can incorporate into your charting. I think it’s important that we don’t rush into treatment, especially when someone has metastatic disease.
The preferred regimens are the multikinase inhibitors vandetanib [Caprelsa] and cabozantinib [Cabometyx]2 and the [RET] inhibitors selpercatinib [Retevmo] and pralsetinib [Gavreto].3 With symptomatic disease progression, these same therapies can be offered, and probably should be offered, to help disease control and improve quality of life.1
We would never offer chemotherapy for such patients, even though dacarbazine [DTIC-Dome] is listed. Other small molecule inhibitors, like sorafenib [Nexavar] or lenvatinib [Lenvima], can also be considered. Those would be considered much [later in disease progression than] the drugs [mentioned above]. Rarely would you see a tumor mutation burden so high that pembrolizumab [Keytruda] should be offered.
What efficacy have vandetanib and cabozantinib demonstrated? How do the responses differ in patients with and without M918T-positive RET mutations?
In the ZETA trial [NCT00410761] for vandetanib, the patients did not have to have disease progression by RECIST to go on this study. The objective response ate [ORR] was much higher for the vandetanib-treated patients than for those who were treated with placebo [45% vs 13%; odds ratio [OR], 5.48; 95% CI, 2.99-10.79; P < .001].4 Placebo was considered the comparator arm because essentially that’s [all] we had for treatment of the disease.
Dacarbazine, although it is listed on the guidelines, is not approved by the FDA for the treatment of thyroid cancer.5 That’s why placebo was [used in] both this study and the EXAM study [NCT00704730].6,7 The biochemical response [rate] was also improved. [The response rate for calcitonin was 69% versus 3%. For CEA, the response rate was 52% versus 2%].4
In the EXAM trial, cabozantinib likewise conferred an improvement over placebo. [The ORR was 28% in the group that received cabozantinib and 0% in the placebo group (P < .001). Estimated median progression-free survival (PFS) was 11.2 versus 4.0 in the respective groups (HR, 0.28; 95% CI, 0.19-0.40; P < .001)].6
[Similar to vandetanib], the benefit [of cabozantinib treatment] was also seen in the subpopulation of patients [whose samples bore the] RET mutation [that confers the M918T amino acid substitution]. The ORR was 34% among patients with M918T-positive RET [mutations] and 20% in the group with M918T-negative RET [mutations]. Median overall survival [OS] in the group with M918T-positive RET was 44.3 months [HR, 0.60; 95% CI, 0.38-0.94; P = .03]; median PFS was 13.9 months [HR, 0.15; 95% CI, 0.08- 0.28; P < .0001]. In the group with M918T-negative RET, median OS was 20.2 months [HR, 1.12; 95% CI, 0.70-1.82; P = .63] and median PFS was 5.7 months [HR, 0.67; 95% CI, 0.37-1.23; P = .19].7
What do you recommend for patients with M918T-negative RET mutations?
For patients with M918T-negative RET [mutations], vandetanib and cabozantinib are available and those are the drugs that should be used. Unfortunately, we can’t use [RET mutation–targeting drugs] in such patients. They often have a very dismal prognosis and develop bony metastases and extensive amounts of spinal cord compressions. You have to monitor them quite closely and take pain very seriously in such patients.
In general, what influences you to initiate systemic therapy?
In the EXAM study, patients had to demonstrate disease progression.6 I think that’s important. People always ask, “When do you offer treatment?” I think it make[s] sense that patients should have some progression of disease.
Now, if someone has symptoms, that could be a different story. But the important point is that we could give people treatment, and if there isn’t response, or the response is stable disease, we’d be subjecting them to adverse events [AEs] while not really garnering a benefit= from reduction in tumor burden.
What toxicities are most concerning?
AEs of vandetanib included hypertension and [long QT syndrome]. Patients need close monitoring for blood pressure and heart function [irregularities], diarrhea, and weight loss.4
Cabozantinib, in general, is a much more difficult drug. In this study, the dose was 140 mg,7 and that’s what has been registered with the FDA.8 Most patients can’t tolerate a dose of 140 mg of cabozantinib [because of] the AEs. The amount of fatigue, the hand-foot syndrome [palmar plantar erythrodysesthesia], the weight loss, the diarrhea can be substantial.7
Most patients start [cabozantinib] at 80 mg, sometimes 100 mg or 120 mg, but rarely do people start at 140 mg. If you start at 140 mg, it’s important that these patients aren’t given a prescription and told, “I’ll see you in a month,” [but rather] that they come back weekly for reassessments, or the staff, nurse practitioner, or physician’s assistant calls the patient regularly to make sure that their blood pressure is fine [and] they’re tolerating the medications OK.
The majority of patients in the EXAM study discontinued treatment because of disease progression. However, it wasn’t uncommon for patients to discontinue because of AEs or serious AEs [22% in the cabozantinib arm, 9% in the placebo arm].7 Again, close follow-up and monitoring are warranted with these patients.
Can you summarize your thoughts on choosing between vandetanib and cabozantinib?
We often tell patients that both drugs will be used. Based on my clinical experience, if someone has a large tumor burden and you want to try to shrink the cancer, cabozantinib is probably the drug to try, as long as their performance status is good and you believe they can tolerate the drug. Vandetanib is a little easier to tolerate, although close monitoring for [long QT syndrome] and electrolyte [imbalance] need to be done.
How do the RET-mutation–targeting drugs selpercatinib and pralsetinib compare?
The LIBRETTO-001 study [NCT03157128] examined selpercatinib, which inhibits mutant RET.3 This analysis incorporated patients with RET fusion–positive, [differentiated] thyroid cancer either radioactive iodine–refractory [or of a type not treated with radioactive iodine] as well as patients with RET-mutant MTC. Patients had been treated with either cabozantinib or vandetanib, neither, or both.9
The majority of the patients [entered the study with ECOG scores of 0 or 1]. Of the patients with RET-mutant cancer, brain metastases were present at baseline in 7% of those who had received cabozantinib and/or vandetanib and in 2% of those who had received neither drug. [Brain metastases were present in 32% of those with RET fusion–positive cancer.] Brain metastases are not a big issue with MTC, although it can occur with those who have the differentiated thyroid cancers. Among the RET-mutant cancers, the M918T alteration was the most common.9
There were strikingly high response rates compared to what we would see with those other agents we talked about. [The ORR for patients with previously treated RET-mutant cancer was 69% (95% CI, 55%-81%); for patients whose RET-mutant cancer had not been previously treated, the ORR was 73% (95% CI, 62%-82%). Finally, for patients with RET fusion–positive cancer, the ORR was 79% (95% CI, 54%-94%)].9 I have patients who started treatment on these studies over 2 years ago, who remain on study, and are doing quite well.
Almost all patients in all subgroups had some degree of response while on treatment with selpercatinib. Strikingly, there are some people who attained complete responses when treated with selpercatinib.9
[The percentage of patients with previously treated RET-mutant cancer who had PFS at 1 year was 82% (95% CI, 69%-90%). Among patients with previously untreated RET-mutant cancer, the 1-year PFS percentage was 92% (95% CI, 82%-97%), and among patients with RET fusion–positive cancer, the percentage was 64% (95% CI, 37%-82%)]. The majority of these patients do quite well and have remained on treatment.10
The data from the ARROW trial [NCT03037385] of pralsetinib are very similar [to those from the LIBRETTO-001 study of selpercatinib]. The data were presented at the [European Society for Medical Oncology 2020 Congress]. These patients had RET-mutated cancer with prior cabozantinib and/or vandetanib treatment, other systemic treatment, or no prior systemic treatments.10 Overall, these 2 drugs [selpercatinib and pralsetinib] are almost identical.9,10
What are the AE profiles of selpercatinib and pralsetinib?
[Treatment-related] hypertension [of any grade occurred in 30% of all patients treated with selpercatinib]. [Treatment-related] elevation in aspartate and alanine aminotransferase levels, of any grade, [occurred in 28% and 26% of all patients, respectively]. [These were among the most common AEs.] I did have 1 patient who developed acute drug-related hepatitis; after he stopped treatment, his enzymes went back to normal. Only [28%] of people experienced a grade 3, treatment-related AE.9
The hypertension…profiles are very similar [between the 2 drugs].9,10
The FDA has approved pralsetinib for RET-altered thyroid cancers11; and previously, selpercatinib was approved for RET-altered thyroid cancers.12 I think the important takehome point I would like to make is not only do these drugs work, but [during use of any] of these drugs, whether the RET-targeted drugs or the multitargeted inhibitors, the patients require close monitoring. Because what you don’t want is to have the patients come off drug, [because] then it’s going to be harder to garner a long-term response, especially in those patients who are on the multitargeted drugs.
What are the next questions that need to be answered about these drugs?
We don’t know how long the benefit of these agents will last. Also, perhaps the next study could [investigate whether] the dosage could be dropped. Someone talked about [drastically] reducing the dosage because of liver dysfunction. I’ve had patients in [that] situation and they continue to maintain a response.
Fatigue can be an issue, as it is with most oncology medications; dropping the dosage does seem to help. So, it would be interesting to ask whether patients’ dosage can [be reduced] and still [confer] the same benefit.
References:
1. NCCN. Clinical Practice Guidelines in Oncology. Thyroid carcinoma, version 1.2021. Accessed May 21, 2021. https://bit.ly/3z6hUHl
2. Drilon A, Hu ZI, Lai GGY, Tan DSW. Targeting RET-driven cancers: lessons from evolving preclinical and clinical landscapes. Nat Rev Clin Oncol. 2018;15(3):151-167. doi:10.1038/nrclinonc.2017.175
3. Drusbosky LM, Rodriguez E, Dawar R, Ikpeazu CV. Therapeutic strategies in RET gene rearranged non–small cell lung cancer. J Hematol Oncol. 2021;14(1):50. doi:10.1186/s13045-021-01063-9
4. Wells SA Jr, Robinson BG, Gagel RF, et al. Vandetanib in patients with locally advanced or metastatic medullary thyroid cancer: a randomized, double-blind phase III trial. J Clin Oncol. 2012;30(2):134-141. doi:10.1200/JCO.2011.35.5040
5. Dacarbazine. Prescribing information. Hospira; 2021. Accessed May 25, 2021. https://bit.ly/3fJSDuH
6. Elisei R, Schlumberger MJ, Müller SP, et al. Cabozantinib in progressive medullary thyroid cancer. J Clin Oncol. 2013;31(29):3639-3646. doi:10.1200/JCO.2012.48.4659
7. Schlumberger M, Elisei R, Müller S, et al. Overall survival analysis of EXAM, a phase III trial of cabozantinib in patients with radiographically progressive medullary thyroid carcinoma. Ann Oncol. 2017;28(11):2813-2819. doi:10.1093/annonc/mdx479
8. Cometriq. Prescribing information. Exelixis; 2020. Accessed May 25, 2021. https://bit.ly/3canFtG
9. Wirth LJ, Sherman E, Robinson B, et al. Efficacy of selpercatinib in RET-altered thyroid cancers. N Engl J Med. 2020;383(9):825-835. doi:10.1056/NEJMoa2005651
10. Hu M, Subbiah V, Wirth LJ, et al. 1913O Results from the registrational phase I/II ARROW trial of pralsetinib (BLU-667) in patients (pts) with advanced RET mutation-positive medullary thyroid cancer (RET+ MTC). Ann Oncol. 2020;31(suppl 4):S1084. doi:10.1016/j.annonc.2020.08.1401
11. FDA approves pralsetinib for RET-altered thyroid cancers. FDA. December 1, 2020. Accessed May 25, 2021. https://bit.ly/2NLNRl4
12. Retevmo. Prescribing information. Loxo Oncology; 2020. Accessed May 25, 2021. https://bit.ly/2SSiQOR
Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More
Anticipating Novel Options for the RAI-Refractory DTC Armamentarium
May 15th 2023In season 4, episode 6 of Targeted Talks, Warren Swegal, MD, takes a multidisciplinary look at the RAI-refractory differentiated thyroid cancer treatment landscape, including the research behind 2 promising systemic therapy options.
Listen