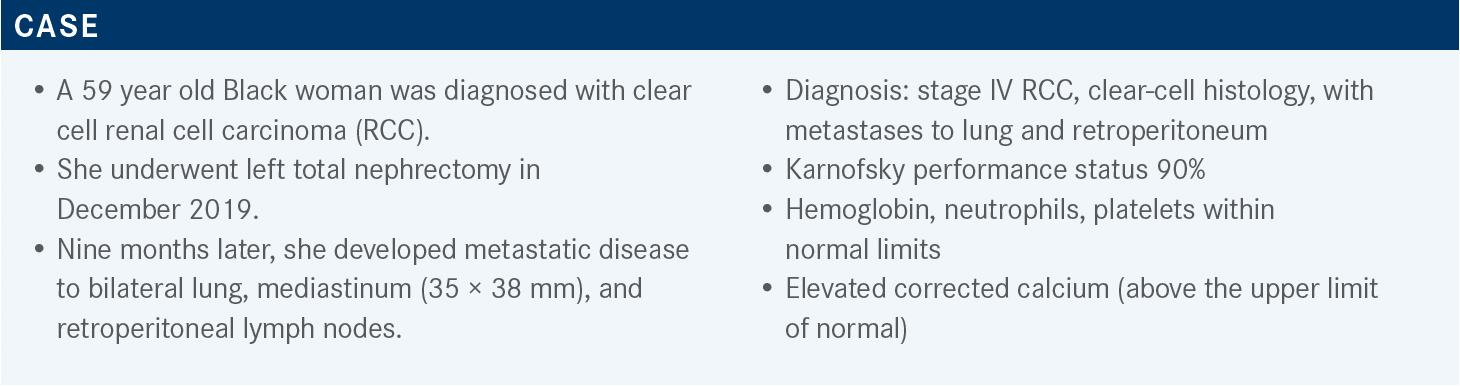
Motzer Examines First-Line Combination Regimens for Clear-Cell RCC
During a Targeted Oncology case-based roundtable event, Robert J. Motzer, MD, discussed the results of several major trials of drug combinations in patients with renal cell carcinoma.
Robert J. Motzer, MD
Kidney Cancer Section Head, Genitourinary Oncology Service
Jack and Dorothy Byrne Chair in Clinical Oncology
Memorial Sloan Kettering Cancer Center
New York, NY
Targeted OncologyTM: What are the options for a patient such as this?
MOTZER: In the [National Comprehensive Cancer Network] guidelines for recommendations for first-line systemic therapy for patients with clear-cell RCC, the patients are stratified, separated according to favorable vs poor and intermediate risk.1 The reason for that is the [results for the] ipilimumab [Yervoy] plus nivolumab [Opdivo] combination [were compelling in] the poor- or intermediate-risk groups, [and this is] where its label is cited, but not in the favorable-risk groups. In contrast, the axitinib [Inlyta] plus pembrolizumab [Keytruda], cabozantinib [Cabometyx] plus nivolumab, and lenvatinib [Lenvima] plus pembrolizumab [combinations] are all category 1 preferred regimens in favorable- and intermediate-risk groups.
Cabozantinib is also in there as a preferred regimen based on a phase 2 study, in which it was compared with sunitinib [Sutent].1 I’d say that ,likely, it falls into [use for] a special group of patients in whom you may want to avoid IO [immuno-oncology] therapy for other reasons. A number of other programs can be chosen as well, including ipilimumab/nivolumab, some TKI [tyrosine kinase inhibitor] single agents in some patients [in a] favorable risk group, and a couple of others. Ipilimumab/nivolumab didn’t meet the [standard of a] preferred regimen, because a survival benefit wasn’t shown with that combination of a TKI plus a PD-L1 inhibitor.
What relevant trials have been published in RCC recently?
The big phase 3 trials that have read out in the last couple of years were [the CheckMate 214 trial (NCT02231749), the KEYNOTE-426 trial (NCT02853331), the CheckMate 9ER trial (NCT03141177), and the CLEAR trial (NCT02811861)].2-6 Sunitinib was the standard of care for first-line treatment for RCC for many years, beginning in 2006 when it was approved, and so as these new IO combinations were brought forward, they were compared with sunitinib in these big phase 3 trials.
The standard arm of each of these was sunitinib.2-6 None of these programs have been compared with each other, and for the most part, most of the studies were run at the same time, or at slightly different time periods.
How did patients with RCC do on ipilimumab/nivolumab?
For the CheckMate 214 trial, which is [investigating] ipilimumab/nivolumab, there is a longer median follow-up.2 It’s now a minimum follow-up of more than 5 years for ipilimumab/nivolumab, with a survival benefit shown for ipilimumab/nivolumab compared with sunitinib.
Now, there is a longer PFS [progression-free survival].2 Initially, there wasn’t. Response rate was about 40%, with about 12% CR [complete response] across the board, and in the intermediate–poor-risk group, it’s 42% vs 27% and 11% CR, so in terms of that program, the benefit is mostly in the intermediate- and poor-risk patients; that’s the [group] it’s approved for. It does have the longest follow-up with a flattening of the curve for PFS as you get out, and durability response, which are the strong points of that program. Response rate is a little lower than with the TKI/IOs, and the CR rate, until recently, with lenvatinib/pembrolizumab, was considered to be the highest of any program.2,5,6
Please describe the axitinib/ pembrolizumab study data.
The first of the TKI IO [trials] to read out was KEYNOTE- 426, [a trial] of axitinib/pembrolizumab. The strengths of this were a very high response rate and a survival benefit right off the bat, and the outcomes were benefits in PFS, survival, and response. Also, another outcome was [seeing benefits] regardless of which risk group [you were in], or whether you were PD-L1 positive or negative—so, a one-size-fits-all for our patients.3
The CheckMate 9ER trial and the CLEAR trial followed that axitinib/pembrolizumab trial, but we will go through those data in a more granular fashion.2-6 So, these are the big trials that have defined first-line treatment in clear cell now; they really represented a tremendous advantage in our therapeutic options for these patients, and they all showed a survival benefit as well. As we mentioned, the first trials were ipilimumab/nivolumab, and then axitinib/pembrolizumab; [those regimens] became established in practice, and then more recently, cabozantinib plus nivolumab and lenvatinib plus pembrolizumab were approved and are now being used for first-line therapy as standard-of-care treatment.7,8
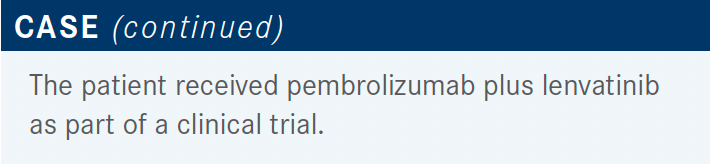
Which data support this regimen for the patient being discussed?
This patient received pembrolizumab plus lenvatinib— the CLEAR study regimen5,6—as part of a clinical trial. It was a randomized phase 3 trial, first-line [treatment], and patients could not have received prior systemic therapy but there was no ineligibility based on risk factor—all risk groups [could participate].
That was a 3-arm trial, with lenvatinib/pembrolizumab, compared with sunitinib, and lenvatinib/everolimus, compared with sunitinib.5,6 Lenvatinib/everolimus is a standard second-line treatment for patients who have progressed on a TKI, and this was part of the full registration packet, to do a large phase 3 trial. In that phase 3, at the time, there was a lot of excitement around TKI/ IO treatments, so that’s why lenvatinib/pembrolizumab was included.
The primary end point was PFS, and the secondary end points included OS [overall survival].5 The dose of lenvatinib in the lenvatinib/pembrolizumab combination was different than the dose of lenvatinib in the everolimus combination. So, the primary end point was reached here. In a trial like this, the comparisons were for each of the [combination regimens to be] compared with sunitinib. No formal comparison of lenvatinib plus pembrolizumab with lenvatinib plus everolimus was done. I do believe that was an exploratory end point, but the formal comparisons were the 2 lenvatinib [regimens] vs sunitinib, and each arm met the primary end point by showing a benefit over sunitinib, but the results with lenvatinib/pembrolizumab were of a greater magnitude.
What was the efficacy in the CLEAR trial?
The HR [hazard ratio] was 0.39, and the P value was statistically significant [95% CI, 0.32-0.49; P <.001].5 The median PFS for lenvatinib/pembrolizumab was almost 24 months, which is the longest that we’ve seen in any phase 3 trial of RCC [95% CI, 20.8-27.7]. This was compared with sunitinib, [which had a PFS of] 9.2 months [95% CI, 6.0-11.0]. Lenvatinib plus everolimus also met the primary end point, showing a benefit in PFS compared with sunitinib, but the median PFS was 14.7 months compared with 9.2 months, so it was not the same degree of magnitude. The strength of the lenvatinib plus pembrolizumab was the efficacy that was seen in this primary end point.
The idea for a phase 3 trial [is that] the trial is powered or has sufficient statistical worth to show a benefit. The primary end point group was the entire population, but subpopulations were set up. They’re always set up around the stratification factors, and several other [factors of interest] are chosen. The thing is, the trial isn’t powered to show a specific benefit in these small subgroups, so the idea is, we like to see the HR, or the trend, going in favor of the combination.5 The HR favored lenvatinib plus pembrolizumab, For the most part, all subgroups are favoring lenvatinib plus pembrolizumab regardless of age, sex, geographic region, [Memorial Sloan Kettering Cancer Center] risk group, PD-L1 status, or what have you.
Have longer-term findings been reported for this group of patients?
Just recently the researchers reported at [European Society for Medical Oncology] a more granular look, and updated some of the forest plots for some of the subsets that were felt to be of particular interest. These include the groups that have sarcomatoid histology, bone metastasis, and prior nephrectomy,5 and they all showed a benefit going in the right way for lenvatinib plus pembrolizumab.
The OS outcome results showed a statistically significant improvement in OS for lenvatinib plus pembrolizumab.5 Now, the median follow-up for this was about 27 months, and so from a statistical standpoint, you can only really look at the curves to the left of the median. Now, what was also interesting was, in contrast, there was no survival benefit for lenvatinib plus everolimus. As a matter of fact, the survival is trending in the wrong direction for lenvatinib plus everolimus here. Based on the lack of OS benefit with lenvatinib plus everolimus, despite the fact that both programs met their primary end point, the winner of the trial was really lenvatinib plus pembrolizumab, moving forward for patients.
This is the response rate for lenvatinib plus pembrolizumab vs lenvatinib plus everolimus vs sunitinib, and the response rate of more than 70% was the first time that we broke the 70% bar rate for response for first-line treatment in a phase 3 trial [95% CI, 66.3%-75.7%].5,6 The 16% CR rate was notable as well, and the median duration of response was very long; it was almost 26 months with lenvatinib plus pembrolizumab, and so this was clearly better than with sunitinib. With lenvatinib plus everolimus, although the response rate was higher with lenvatinib plus everolimus compared with sunitinib, it wasn’t the same magnitude, so the winner for most patients was lenvatinib plus pembrolizumab, from this particular trial.
In terms of treatment exposure and safety, the median duration of treatment on this trial for lenvatinib plus pembrolizumab was 17 months, which was more than double that of sunitinib [7.8 months].5 The longer that patients are on a trial, the more likely it is that they will experience adverse events [AEs]. And you have to take that into consideration when you’re looking at the incidence of AEs, if a patient has been on treatment for more than twice as long on one regimen compared with another.
How were patients affected by AEs on the CLEAR study?
The takeaways from here are that most people had an AE, very often a grade 3 AE, on this particular program, with any of the treatment regimens, and a large number of people had dose reductions across the board with the regimens.5 The idea behind lenvatinib in these programs has been to dose high with the idea of treating for maximal efficacy, and then backing off on the dose for patients who have AEs, and so that is reflected by the relatively high rate of dose reduction with lenvatinib plus pembrolizumab and lenvatinib plus everolimus in this program. But in terms of patients coming off study or discontinuing for AEs, for both regimens it was relatively low. Only about 13% of people had lenvatinib plus pembrolizumab discontinued as a regimen because of AEs.
Let’s discuss treatment-related AEs that occurred with greater than 20% frequency with lenvatinib plus pembrolizumab compared with sunitinib.5 For lenvatinib plus pembrolizumab, many of the patients had all-grade AEs, but the percent with grade 3 or 4 AEs was relatively well distributed among the toxicities. Most of the toxicities in this program were defined by the TKI. Very few, about 10%, were immune-related AEs. The most common one was hypothyroidism, and about 10% of patients wind up on high-dose steroids for immune-related AEs, so most of the AEs are TKI related.
How do you sequence therapies in this setting?
These programs with TKI/IOs have left us a little bit in the dark in terms of what is second- or third-line therapy, because these combinations do utilize the main mechanisms of action for our compounds with IO and TKI. One of the advantages of ipilimumab/nivolumab is that if patients progress, they haven’t seen a TKI, and they generally respond quite well. So it has left us in a little bit of a quandary in terms of what’s the best second- or third-line treatment for our patients, and also whether IO has a role in second- or third-line combination with TKI. I think some of the big trials that are underway are addressing that, but the landscape has changed so quickly that it is really an area that needs to be further defined.
What dose of lenvatinib and pembrolizumab do you use for patients?
For the most part, the proponents of the program and the sponsor feel that the efficacy is directly [related] to dose intensity up front.9,10 However, I think if you’re dealing with a patient with a poor performance status, and you’re concerned about the full dose, you can always use a lower dose. We all do that, particularly in second- or third-line therapy, but in patients who are fit, I think it is better to go with the full dose and dose reduce. I’ve found it’s harder to go the other way, to start out with a lower dose and go up, because most people are experiencing some AEs.
What was the design of the cabozantinib/nivolumab trial for patients with RCC?
Now [let’s do a] little review of the cabozantinib/ nivolumab data. This was the CheckMate 9ER trial.4 It had very similar criteria to the CLEAR trial: Patients had to have a clear-cell component, and they were treatment naive. This was a 1:1 comparison of cabozantinib plus nivolumab vs sunitinib, and one of the points in terms of dosing for this regimen is that the cabozantinib is at a lower dose than that which is recommended in single-agent therapy, according to the previous approval and following TKI.4,11 Here, it’s cabozantinib 40 mg plus nivolumab, given every 2 weeks.4 The primary end point was PFS, and OS was a secondary end point.
What did CheckMate 9ER demonstrate in these patients?
The trial met the primary end point, showing a benefit in PFS with cabozantinib plus nivolumab. Again, [there was] a nice HR of 0.51, showing a benefit across the study for PFS for cabozantinib plus nivolumab vs sunitinib [95% CI, 0.41-0.64; P < .0001].4 The magnitude of the median PFS was a little less than we saw with the CLEAR study, but in terms of the benefit, cabozantinib plus nivolumab was quite good, [at 17 months], over sunitinib, which had a median of 8.3 months.
For all of the subgroups, basically, there was a benefit for this combination compared with sunitinib.4 Highlights of this are for [the categories of] favorable, intermediate, and poor; it’s all trending in the right direction for cabozantinib plus nivolumab, although the HR that showed the strongest benefit was actually in the poor-risk patients. There was a benefit regardless of PD-L1 status, and also, another point for cabozantinib was that there was a fairly strong benefit for patients who had bone metastasis, since this has always been brought up as a particular area of efficacy for cabozantinib.
Also, an OS benefit was seen in this. The median follow-up was fairly short, only 18 months, but there was a benefit in survival.4 We’re expecting an update of this through a median follow-up of about 2 years, to be reported in 2022, so it will be updated at some point fairly soon. So [there is a] survival benefit for cabozantinib plus nivolumab over sunitinib, which seems to be the gold standard now for choosing these regimens as standard of care.
The objective response rate for cabozantinib plus nivolumab was 55% to 56%, double that of sunitinib, which was 27.1% [P < .0001].4 And there were complete responders (although the number was a little lower than that seen in a prior trial) and the responses as well were quite durable: The median was 20 months compared with 11 months with sunitinib. So again, a very active, powerful regimen that clearly beats sunitinib in all comers.
The safety and the median duration of therapy was longer with cabozantinib plus nivolumab vs sunitinib, 14 months compared with 9.2 months.4 Most of the patients had a dose reduction with cabozantinib, and again, this was not cabozantinib 60 mg, this was 40 mg, so patients were reduced down to 20 mg, or 20 mg every other day. Very [few] went off study because of toxicity. Only 3% of people had both drugs discontinued for toxicity on this [regimen]. So while we saw a fairly high [rate of] dose reduction with a starting dose, that’s lower than the monotherapy dose. Patients [were able to continue] on it and adhere to therapy for a long time.
What was the toxicity with this combination? How does it compare to the other combinations discussed?
The safety profile for cabozantinib plus nivolumab compared with sunitinib showed that most of the safety [issues are] driven by the TKI, and not the IO, in these programs.4 I think the combination does seem to have higher incidence of some of the TKI toxicities. For example, hand-foot syndrome was a little bit higher in this program with the combinations of the IO and the TKI, and there was some increase in liver function tests with this particular regimen.
The lenvatinib/pembrolizumab regimen has virtually no liver toxicity, but it has others, like hypertension. The one to note with cabozantinib/nivolumab, as well as with axitinib/ pembrolizumab, has really been a liver toxicity, which needs to be monitored fairly closely and managed. But in general, again, cabozantinib/nivolumab a fairly well-tolerated regimen, and efficacy is driving its use.
REFERENCES
1. NCCN. Clinical Practice Guidelines in Oncology. Kidney cancer, version 4.2022. Accessed January 11, 2022. https://bit.ly/3qqkYLP
2. Albiges L, Tannir NM, Burotto M, et al. Nivolumab plus ipilimumab vs sunitinib for first-line treatment of advanced renal cell carcinoma: extended 4-year follow-up of the phase III CheckMate 214 trial. ESMO Open. 2020;5(6):e001079. doi:10.1136/esmoopen-2020-001079
3. Rini BI, Plimack ER, Stus V, et al; KEYNOTE-426 Investigators. Pembrolizumab plus axitinib vs sunitinib for advanced renal-cell carcinoma. N Engl J Med. 2019;380(12):1116-1127. doi:10.1056/NEJMoa1816714
4. Choueiri TK, Powles T, Burotto M, et al; CheckMate 9ER Investigators. Nivolumab plus cabozantinib vs sunitinib for advanced renal-cell carcinoma. N Engl J Med. 2021;384(9):829-841. doi:10.1056/NEJMoa2026982
5. Motzer R, Alekseev B, Rha SY, et al; CLEAR Trial Investigators. Lenvatinib plus pembrolizumab or everolimus for advanced renal cell carcinoma. N Engl J Med. 2021;384(14):1289-1300. doi:10.1056/NEJMoa2035716
6. Grünwald V, Powles T, Choueiri TK, et al. Lenvatinib plus everolimus or pembrolizumab versus sunitinib in advanced renal cell carcinoma: study design and rationale. Future Oncol. 2019;15(9):929-941. doi:10.2217/fon-2018-0745
7. FDA approves nivolumab plus cabozantinib for advanced renal cell carcinoma. FDA. January 22, 2021. Accessed January 11, 2022. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-nivolumab-plus-cabozantinib-advanced-renal-cell-carcinoma
8. FDA approves lenvatinib plus pembrolizumab for advanced renal cell carcinoma. FDA. August 11, 2021. Accessed January 11, 2022. https://bit.ly/3tvYJGx
9. Lenvima. Prescribing information. Eisai; 2021. Accessed January 11, 2022. https://bit.ly/3222B6M
10. Keytruda. Prescribing information. Merck Sharpe & Dohme; 2021. Accessed January 11, 2022. https://bit.ly/33icwpk
11. Cabometyx. Prescribing information. Exelixis, Inc; 2021. Accessed January 11, 2022. https://bit.ly/3qqlf1j

Enhancing Precision in Immunotherapy: CD8 PET-Avidity in RCC
March 1st 2024In this episode of Emerging Experts, Peter Zang, MD, highlights research on baseline CD8 lymph node avidity with 89-Zr-crefmirlimab for the treatment of patients with metastatic renal cell carcinoma and response to immunotherapy.
Listen
Beyond the First-Line: Economides on Advancing Therapies in RCC
February 1st 2024In our 4th episode of Emerging Experts, Minas P. Economides, MD, unveils the challenges and opportunities for renal cell carcinoma treatment, focusing on the lack of therapies available in the second-line setting.
Listen