Lunning Discusses Second-Line Treatments in Diffuse Large B-Cell Lymphoma
During a Targeted Oncology case-based roundtable event, Matthew A. Lunning, DO, discussed the results of the L-MIND study of tafasitamab and lenalidomide in patients with diffuse large B-cell lymphoma.
Matthew A. Lunning, DO
Associate Vice Chair of Research
Associate Professor, Internal Medicine
Division of Oncology and Hematology
Department of Internal Medicine
UNMC College of Medicine
Omaha, NE

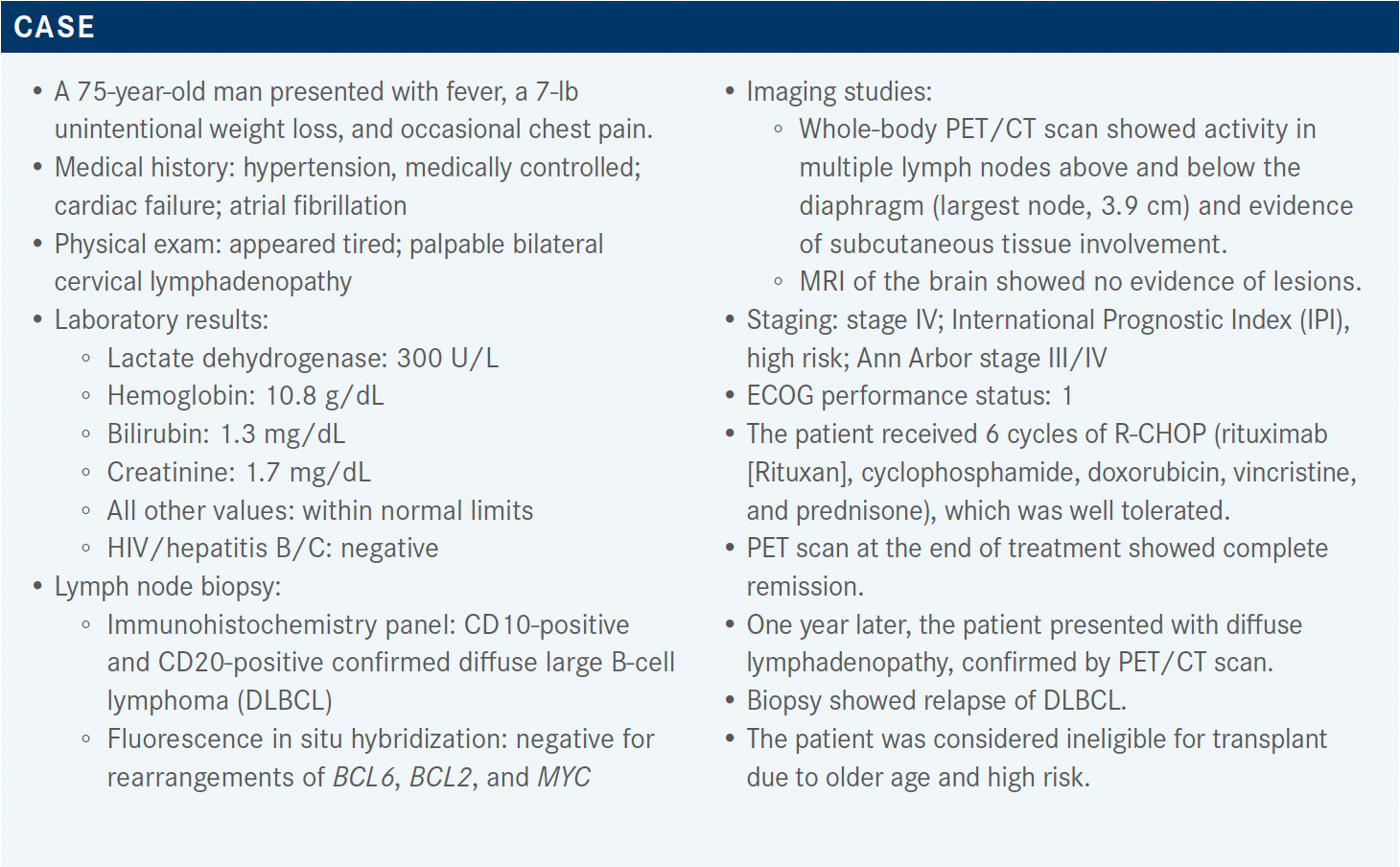
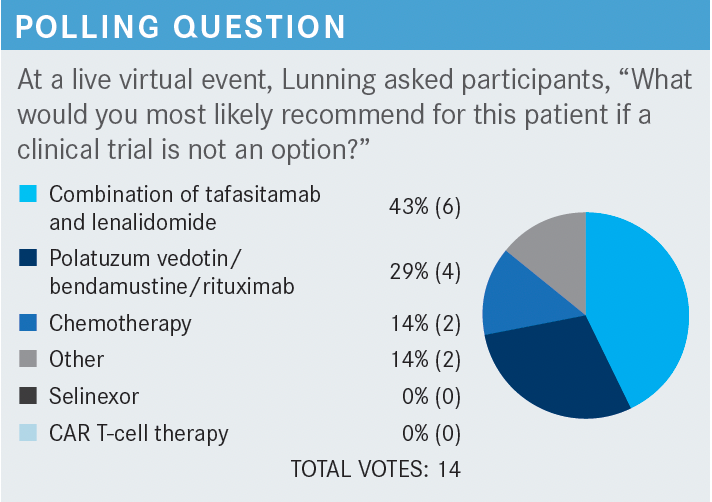
Targeted Oncology™: What second-line and subsequent therapies does the National Comprehensive Cancer Network (NCCN) recommend for DLBCL patients who are not transplant candidates?
LUNNING: One of the preferred regimens is the combination of gemcitabine [Infugem] and oxaliplatin [Eloxatin], with or without rituximab. The other is polatuzumab vedotin-piiq [Polivy], with or without bendamustine [Belrapzo], and with or without rituximab.1 I think [individuals] are getting creative, using this regimen as a bridging option toward chimeric antigen receptor [CAR] T-cell therapy; this regimen was approved to treat DLBCL in adults who have progressed after 2 or more prior therapies.2 Polatuzumab is an antibody-drug conjugate that targets CD79b and carries a monomethyl auristatin E warhead.3
Other recommended regimens include tafasitamab-cxix [Monjuvi] plus lenalidomide [Revlimid],1 which was approved by the FDA to treat adults with relapsed/refractory DLBCL who are not eligible for autologous stem cell transplant [ASCT].4 Tafasitamab is a monoclonal antibody that targets CD19.5
What follow-up strategy does the NCCN recommend for patients who achieve a metabolic complete remission?
The recommendations include a physical examination and laboratory [testing every 3 to 6 months for 5 years and then annually], plus imaging [to be performed] no more than every 6 months for 2 years. [Follow-up beyond these specified time frames should only be pursued for cause], for instance, if you detect something [during] a physical exam.1
For patients who have relapsed twice or more, CAR T-cell therapy is commercially approved. The most recent approval was for lisocabtagene maraleucel [Breyanzi], following the approvals of tisagenlecleucel [Kymriah] and axicabtagene ciloleucel [Yescarta].1,6-8 The NCCN notes that it is unclear how tafasitamab and loncastuximab tesirine-lpyl [Zynlonta], both CD19 [antagonists],5,9 affect the efficacy of anti-CD19 CAR T-cell therapies [such as these].1,10-12
The NCCN also notes that bendamustine may negatively affect the [success of] CAR T-cell therapy. Other recommended options for patients who have relapsed at least twice are clinical trials, alternative second-line therapies, radiation therapy (useful in the palliative setting if the patient has a bothersome lesion), and other best supportive care.1
What have recent studies revealed about the action and efficacy of tafasitamab and lenalidomide?
Formerly known as MOR 208, tafasitamab is an anti-CD19 monoclonal antibody that has an Fc-enhanced design to encourage antibody-dependent cellular cytotoxicity and antibody-dependent cellular phagocytosis. It can lead directly to cell death.5,13 Lenalidomide can act via T-cell and natural killer–cell activation and expansion.14 It also can cause direct cell death.14 Lenalidomide has [activity in the settings of] multiple myeloma, follicular lymphoma, [relapsed/refractory] DLBCL, and mantle cell lymphoma.15,16
There has been encouraging [evidence of] single-agent activity [for both tafasitamab17-20 and lenalidomide21-24] as well as activity [of lenalidomide in combination] with tafasitamab.25-27
Additionally, data [from studies of cell line models] show that the combination of tafasitamab and lenalidomide works better than either single agent.28
The phase 2 L-MIND study [NCT02399085] was a single-arm, open-label, multicenter trial [of tafasitamab and lenalidomide] in relapsed/refractory DLBCL. In this study, patients received 1 to 3 prior lines of therapy and were not eligible for high-dose chemotherapy and ASCT. Primary refractory patients were excluded; however, the definition [of primary refractory] did evolve over the course of this study.26,29
Please explain the design of the L-MIND study.
Tafasitamab [12 mg/kg] was delivered weekly for cycles 1 through 3 [on days 1, 8, 15, and 22], with a loading dose on day 4, and lenalidomide [25 mg] was delivered on days 1 through 21. [During cycles 4 through 12], tafasitamab administration was reduced to every other week; in contrast, an attempt was made to maintain the initial lenalidomide dosage.
[Beyond week 12], for patients who achieved a complete response [CR], a partial response [PR], or stable disease, lenalidomide was discontinued and tafasitamab was continued every other week until progression, toxicity, or the patient’s decision to discontinue. The primary end point was overall response rate [ORR] based upon central review.26,29
Some people [may question this study’s use of a] 25-mg dosage of lenalidomide in the lymphoma setting. About half of the patients required at least 1 dose reduction; however, about 80% of the patients were able to continue receiving a lenalidomide dosage of at least 20 mg. Only 1 patient in 5 had permanent lenalidomide discontinuation due to toxicity.26
In this study, the median patient age was 72 years, and the study population comprised nearly equal numbers of patients with low [0-2] and high [3-5] IPI scores at the time of accrual. The median number of prior lines of therapy was 2, with a range of 1 to 4 with most patients; 50% had received 1 prior line of therapy and 40% had received 2 prior lines of therapy.26 Eighty-one percent of the patients did not have primary refractory disease, 19% had disease that was refractory to their initial therapy, and only 11% of the patients had had a prior ASCT and there were missing data on cell of origin.26
What were the results of the study?
The results were analyzed after a median follow-up of 13.2 months,26 and after a median follow-up of greater than or equal to 35.0 months.30,31 Between these time points, the rate of CR decreased slightly from 43% to 40%. The ORR changed from 60% to 57.5%. The median duration of response [DOR] increased from 21.7 months to 43.9 months [95% CI, 26.1 months-not reached (NR)].
The median progression-free survival [PFS] at 17.3 months of follow-up was 12.1 months26; after 33.9 months of follow-up, median PFS was 11.6 months [95% CI, 6.3-45.7 months].30 The median overall survival [OS] was NR at 19.6 months of follow-up; however, after a follow-up at 42.7 months, the median OS was 33.5 months [95% CI, 18.3 months-NR].
The results were analyzed according to the type of response (CR vs PR), and at a follow-up of greater than or equal to 35 months, the median DOR, median PFS, and median OS were NR for patients who had achieved a CR. For patients who had achieved only a PR, median DOR was 5.6 months [95% CI, 2.2 months-NR]; [median PFS was 7.4 months (95% CI, 5.3 months-NR) and median OS was 22.5 months (95% CI, 8.6 months-NR)].
The results were also analyzed according to the number of prior lines of therapy, 1 vs 2 or more. The CR rate was slightly higher in those individuals who had received 1 prior line of therapy vs those who had received 2 or more prior lines [47.5% vs 32.5%, respectively]. Similarly, the ORR was 67.5% [95% CI, 50.9%-81.4%] vs 47.5% [95% CI, 31.5%-63.9%], respectively. The median DOR was 43.9 months [95% CI, 9.1 months-NR] vs NR [95% CI, 15.0 months-NR], respectively. Finally, median OS was 45.7 months [95% CI, 24.6 months-NR] vs 15.5 months [95% CI, 8.6 months-NR], respectively.30
What did the L-MIND study reveal about the safety of the tafasitamab plus lenalidomide combination?
The hematologic adverse events [AEs] in this study were driven by the AE profile of lenalidomide. The AEs included lymphopenia [of grade 3 or 4, experienced by 3% of patients5,26]; for this reason, when I use this regimen, I put patients on acyclovir [Sitavig] prophylaxis. Other grade 3 or grade 4 AEs included neutropenia [48%], febrile neutropenia [12%], and thrombocytopenia [17%].
Growth factor use was allowed during this study.5,26 The nonhematologic AEs observed in this study were also typical of the AEs seen with lenalidomide use: rash, diarrhea, peripheral edema, joint aches, and infections, all mostly low grade.5,26
Serious AEs occurred in about 50% of patients. Discontinuation of combination therapy due to an AE occurred in 12% of patients. Treatment-emergent AEs leading to death occurred in 13% of patients. Most patients [77.5%] were able to receive a lenalidomide dose greater than or equal to 20 mg over the duration of treatment.5,26,30
Comparison was made between the AE profile of patients who received the tafasitamab plus lenalidomide combination (up to 12 cycles, with a median exposure of 6.5 months), and patients who continued tafasitamab monotherapy. Once the lenalidomide was stopped after 12 cycles, the hematologic toxicities decreased substantially, and some of the nonhematologic toxicities, including diarrhea, [decreased], but there were some continued risks of infection.29
Are there data that demonstrate the superior efficacy of tafasitamab plus lenalidomide relative to lenalidomide monotherapy?
The RE-MIND study [NCT04150328] was a propensity score– based, 1-to-1 matched comparison of the tafasitamab plus lenalidomide combination vs lenalidomide monotherapy in transplant-ineligible patients with relapsed/refractory DLBCL and 1 to 3 prior lines of therapy. This study compared the data from patients in the L-MIND study with real-world data from 490 lenalidomide monotherapy patients, and the primary end point was difference in ORR.32
After considering baseline covariates, 152 individuals were matched, 76 tafasitamab-lenalidomide patients and 76 monotherapy patients, respectively. The ORR, CR rate, and OS were all significantly better among the patients who had received the combination than among those who had received monotherapy.
Patients who had received the combination showed a CR rate of 39.5% and a PR rate of 27.6%. For patients who had received monotherapy, the CR rate was 13.2% and the PR rate was 21.1%.32
REFERENCES
1. NCCN. Clinical Practice Guidelines in Oncology. B-cell lymphomas, version 5.2021. Accessed January 4, 2022. https://www.nccn.org/professionals/physician_gls/pdf/b-cell.pdf
2. FDA approves polatuzumab vedotin-piiq for diffuse large B-cell lymphoma. FDA. June 10, 2019. Accessed January 4, 2022. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-polatuzumab-vedotin-piiq-diffuse-large-b-cell-lymphoma
3. Polivy. Prescribing information. Genentech; 2020. Accessed January 4, 2022. https://www.gene.com/download/pdf/polivy_prescribing.pdf
4. FDA grants accelerated approval to tafasitamab-cxix for diffuse large B-cell lymphoma. FDA. Updated August 3, 2020. Accessed January 4, 2022. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-grants-accelerated-approval-tafasitamab-cxix-diffuse-large-b-cell-lymphoma
5. Monjuvi. Prescribing information. Morphosys US; 2020. Accessed January 4, 2022. https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/761163s000lbl.pdf
6. FDA approves lisocabtagene maraleucel for relapsed or refractory large B-cell lymphoma. FDA. February 5, 2021. Accessed January 8, 2022. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-lisocabtagene-maraleucel-relapsed-or-refractory-large-b-cell-lymphoma
7. FDA approves tisagenlecleucel for adults with relapsed or refractory large B-cell lymphoma. FDA. May 3, 2018. Accessed January 8, 2021. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-tisagenlecleucel-adults-relapsed-or-refractory-large-b-cell-lymphoma
8. FDA approves axicabtagene ciloleucel for large B-cell lymphoma. FDA. Updated October 25, 2017. Accessed January 8, 2022. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-axicabtagene-ciloleucel-large-b-cell-lymphoma
9. Zynlonta. Prescribing information. ADC Therapeutics; 2021. Accessed January 9, 2022. https://www.adctherapeutics.com/wp-content/uploads/2021/12/ZYNLONTA-PI_8.5-x-11-Format_Download_093021.pdf
10. Breyanzi. Prescribing information. Bristol-Myers Squibb; 2021. Accessed January 8, 2022. https://packageinserts.bms.com/pi/pi_breyanzi.pdf
11. Kymriah. Prescribing information. Novartis; 2021. Accessed January 8, 2022. https://www.novartis.us/sites/www.novartis.us/files/kymriah.pdf
12. Yescarta. Prescribing information. Kite; 2021. Accessed January 8, 2022. https://www.gilead.com/-/media/files/pdfs/medicines/oncology/yescarta/yescarta-pi.pdf
13. Horton HM, Bernett MJ, Pong E, et al. Potent in vitro and in vivo activity of an Fc-engineered anti-CD19 monoclonal antibody against lymphoma and leukemia. Cancer Res. 2008;68(19):8049-8057. doi:10.1158/0008-5472.CAN-08-2268
14. Wu L, Adams M, Carter T, et al. Lenalidomide enhances natural killer cell and monocyte-mediated antibody-dependent cellular cytotoxicity of rituximab-treated CD20+ tumor cells. Clin Cancer Res. 2008;14(14):4650-4657. doi:10.1158/1078-0432.CCR-07-4405
15. Zhang LH, Kosek J, Wang M, Heise C, Schafer PH, Chopra R. Lenalidomide efficacy in activated B-cell-like subtype diffuse large B-cell lymphoma is dependent upon IRF4 and cereblon expression. Br J Haematol. 2013;160(4):487-502. doi:10.1111/bjh.12172
16. Revlimid. Prescribing information. Celgene; 2021. Accessed January 8, 2022. https://packageinserts.bms.com/pi/pi_revlimid.pdf
17. Awan FT, Lapalombella R, Trotta R, et al. CD19 targeting of chronic lymphocytic leukemia with a novel Fc-domain-engineered monoclonal antibody. Blood. 2010;115(6):1204-1213. doi:10.1182/blood-2009-06-229039
18. Parikh SA, Rabe KG, Call TG, et al. Diffuse large B-cell lymphoma (Richter syndrome) in patients with chronic lymphocytic leukaemia (CLL): a cohort study of newly diagnosed patients. Br J Haematol. 2013;162(6):774-782. doi:10.1111/bjh.12458
19. Jurczak W, Zinzani PL, Gaidano G, et al. Phase IIa study of the CD19 antibody MOR208 in patients with relapsed or refractory B-cell non-Hodgkin’s lymphoma. Ann Oncol. 2018;29(5):1266-1272. doi:10.1093/annonc/mdy056
20. Jurczak W, Zinzani PL, Hess G, et al. A phase IIa, open-label, multicenter study of single-agent tafasitamab (MOR208), an Fc-optimized anti-CD19 antibody, in patients with relapsed or refractory B-cell non-Hodgkin’s lymphoma: long-term follow-up, final analysis. Blood. 2019;134(suppl 1):4078. doi:10.1182/blood-2019-124297
21. Lapalombella R, Yu B, Triantafillou G, et al. Lenalidomide down-regulates the CD20 antigen and antagonizes direct and antibody-dependent cellular cytotoxicity of rituximab on primary chronic lymphocytic leukemia cells. Blood. 2008;112(13):5180-5189. Published correction appears in Blood. 2009;114(16):3506.
22. Wiernik PH, Lossos IS, Tuscano JM, et al. Lenalidomide monotherapy in relapsed or refractory aggressive non-Hodgkin’s lymphoma. J Clin Oncol. 2008;26(30):4952-4957. doi:10.1200/JCO.2007.15.3429
23. Witzig TE, Vose JM, Zinzani PL, et al. An international phase II trial of single-agent lenalidomide for relapsed or refractory aggressive B-cell non-Hodgkin’s lymphoma. Ann Oncol. 2011;22(7):1622-1627. doi:10.1093/annonc/mdq626
24. Czuczman MS, Trněný M, Davies A, et al. A phase 2/3 multicenter, randomized, open-label study to compare the efficacy and safety of lenalidomide vs investigator’s choice in patients with relapsed or refractory diffuse large B-cell lymphoma. Clin Cancer Res. 2017;23(15):4127-4137. doi:10.1158/1078-0432.CCR-16-2818
25. Salles G, Duell J, González Barca E, et al. Primary analysis results of the single-arm phase II study of MOR208 plus lenalidomide in patients with relapsed or refractory diffuse large B-cell lymphoma (L-MIND). Hematol Oncol. 2019;37(suppl 2):173-174. doi:10.1002/hon.130_2629
26. Salles G, Duell J, González Barca E, et al. Tafasitamab plus lenalidomide in relapsed or refractory diffuse large B-cell lymphoma (L-MIND): a multicentre, prospective, single-arm, phase 2 study. Lancet Oncol. 2020;21(7):978-988. doi:10.1016/S1470-2045(20)30225-4
27. Salles G, Duell J, González Barca E, et al. Long-term outcomes from the phase II L-MIND study of tafasitamab (MOR208) plus lenalidomide in patients with relapsed or refractory diffuse large B-cell lymphoma. Paper presented at: 25th European Hematology Association Annual Congress; June 11-21, 2020; virtual. Accessed January 6, 2022. https://library.ehaweb.org/eha/2020/eha25th/293691/gilles.salles.long-term.outcomes.from.the.phase.ii.l-mind.study.of.tafasitamab.html
28. Zinzani PL, Rodgers T, Marino D, et al. RE-MIND: Comparing Tafasitamab + Lenalidomide (L-MIND) with a Real-world Lenalidomide Monotherapy Cohort in Relapsed or Refractory Diffuse Large B-cell Lymphoma. Clin Cancer Res. 2021 Nov 15;27(22):6124-6134. doi: 10.1158/1078-0432.CCR-21-1471
29. Salles G, Duell J, Gonzalez Barca E, et al. Primary analysis results of the single-arm phase II study of MOR208 plus lenalidomide in patients with relapsed or refractory diffuse large B-cell lymphoma (L-MIND). Paper presented at: 15th International Conference on Malignant Lymphoma; June 18-22, 2019; Lugano, Switzerland. Accessed January 6, 2022. https://www.morphosys.de/sites/default/files/phone-conferences/downloads/190622_morphosys_icml_2019_presentation.pdf
30. Düll J, Maddocks KJ, Gonzalez-Barca E, et al. Long-term analyses from L-MIND, a phase II study of tafasitamab (MOR208) combined with lenalidomide (LEN) in patients with relapsed or refractory diffuse large B-cell lymphoma (R/R DLBCL). J Clin Oncol. 2021;39(suppl 15):7513. doi:10.1200/JCO.2021.39.15_suppl.7513
31. Duell J, Maddocks KJ, González-Barca E, et al. Long-term outcomes from the phase II L-MIND study of tafasitamab (MOR208) plus lenalidomide in patients with relapsed or refractory diffuse large B-cell lymphoma. Haematologica. 2021 Aug 19. doi: 10.3324/haematol.2021.279802
32. Nowakowski GS, Rodgers TD, Marino D, et al. RE-MIND study: a propensity score-based 1:1 matched comparison of tafasitamab + lenalidomide (L-MIND) vs lenalidomide monotherapy (real-world data) in transplant-ineligible patients with relapsed/refractory (R/R) diffuse large B-cell lymphoma (DLBCL). J Clin Oncol. 2020;38(suppl 15):8020. doi:10.1200/JCO.2020.38.15_suppl.8020
