PARTICIPANT LIST
Syed Abutalib, MD
Timothy Fenske, MD, MS
Neel Shah, MD
Gowri Ramadas, MD
Hongtao Liu, MD, PhD
Bety Ciobanu, MD
EVENT REGION Illinois, Indiana, and Wisconsin
During a Targeted Oncology™ Case-Based Roundtable™ event, Binod Dhakal, MD, MS, and participants discussed which treatment should come next for a patient with relapsed multiple myeloma depending on the patient's ability to travel for care.
Binod Dhakal, MD, MS (MODERATOR)
Associate Professor of Medicine
Division of Hematology
Medical College of Wisconsin
Milwaukee, WI
Syed Abutalib, MD
Timothy Fenske, MD, MS
Neel Shah, MD
Gowri Ramadas, MD
Hongtao Liu, MD, PhD
Bety Ciobanu, MD
EVENT REGION Illinois, Indiana, and Wisconsin
CASE SUMMARY
A 63-year-old man received a diagnosis of IgGκ multiple myeloma 8 years ago. He lives in a rural community and now presents with penta-refractory disease progression after 4 prior lines of therapy that included autologous stem cell transplant, 2 proteasome inhibitors (PIs), 2 immunomodulatory imide drugs, and 1 anti-CD38 antibody. His personal medical history includes hypertension controlled with lisinopril, and he now has an ECOG performance score of 1. The patient asked about chimeric antigen receptor (CAR) T-cell therapy, but after counseling, he opted to pursue an alternative therapeutic because of waiting lists at accessible institutions.
DISCUSSION QUESTION
DHAKAL: One can still use treatment locally. The patient doesn’t need to come to the academic center for the CAR T-cell therapy and bispecific antibody if you choose selinexor [Xpovio] plus dexamethasone, which is quite a reasonable option.1 Other options are alkylators, including bendamustine [Treanda] and cyclophosphamide [Cytoxan]. I have sometimes given the high-dose cyclophosphamide in some patients and [saw] decent response and disease control for some time. One can recycle whatever the patient has used in the past, for example, in somebody who has started on VRd [bortezomib (Velcade), lenalidomide (Revlimid), and dexamethasone] as an induction therapy but [has had] refractory [response] to other agents and had some toxicity using that kind of combination. So there are a lot of options we can still try locally.
ABUTALIB: Because this is a patient with penta-refractory [disease], let’s say the patient also had carfilzomib [Kyprolis]. What is the role of using carfilzomib and lenalidomide with bendamustine? Any use in doing that, or can we [use] bendamustine and dexamethasone?
DHAKAL: A couple of studies have been done, and we did one study ourselves where we combined bendamustine with a PI. And what we have found out is [that] patients [with disease] refractory to the PI had some response [when it was combined with bendamustine]. But I agree with you, and these responses are not going to be long-lasting responses. If you want to have long duration of responses, patients need to get CAR T-cell therapy or bispecific antibodies in clinical trials or commercially. Patients [with disease] refractory to bortezomib did respond to the combination with bendamustine, but maybe this is driven by bendamustine. We don’t know.
ABUTALIB: When they use single-agent bendamustine, I’ve seen responses. So we don’t know [whether] adding bortezomib has any utility in somebody who’s [not responded to] it. It might be bendamustine doing the work.
DHAKAL: Yes, that could be correct. Unfortunately, there [is] no randomized study that [has] been done with bendamustine. It’s all single-arm studies [with] either a single agent or in combination.
ABUTALIB: For the high-dose or fractionated cyclophosphamide, what dose do you use? What is the frequency?
DHAKAL: I have mainly done the dose that we use for mobilization. I have not [used] more than 3.5 g/m2. That is the highest I have done, and I have done that twice weekly 2 weeks apart. Most of the time, I’ve done intermediate-dose cyclophosphamide from 1.5 to 2 g/m2. Again, this is just 1 or 2 episodes. You don’t want to do that frequently for these patients. You just want to temporarily [reduce it] so they can control the disease for at least a month and get to the main treatment that you want to go for.
ABUTALIB: One thing that is missing is that we often do, in real practice, allogeneic transplant. I know I use it, but does it have any role after the BCMA [B-cell maturation antigen] therapy [teclistamab; Tecvayli] was approved?
DHAKAL: At this stage in late relapses, the role of allogeneic transplant is probably none. If there is a role, it is mainly in newly diagnosed myeloma, perhaps after autologous transplant, and in very young patients. But right now, a lot of trials are trying to move CAR T-cell therapy and bispecific antibodies to the early lines. So with these new therapies with high response rates emerging, I’m not sure what will happen to the allogeneic transplant as a modality.
FENSKE: What about the ultrahigh risk for plasma cell leukemia? Do we think these treatments are going to solve the problem for patients with plasma cell leukemia?
DHAKAL: I have given CAR T-cell therapy [to] some patients with plasma cell leukemia off label commercially, and I have seen good responses. Having said that, we don’t have any data, but a lot of trials using this highly effective immunotherapy in high-risk and ultrahigh-risk myeloma are already being developed. So until we have that trial, we cannot say. But if there are any agents likely to provide benefit, I think these are the ones. Because these are hard-to-treat patients, and we know for these patients [with] ultrahigh-risk [disease], whatever you do, they don’t [survive] long. You’re recycling the drug very fast in a short time, and even if they have a complete response, that lasts for a very short time. If there are some agents out there likely to provide a little longer benefit and potentially long-term benefit in these difficult-to-treat patients who are a population with an unmet need, they are perhaps immunotherapy [medications] using CAR T cells and bispecific antibodies.
FENSKE: I’m thinking that prior to the advent of CAR T cells and these BCMA-targeted agents, and this is anecdotal, the only time I can think of where somebody with bona fide primary or secondary plasma cell leukemia [experienced] long-term remission was with allogeneic transplant. Even tandem autologous transplants didn’t [treat] those patients well. Maybe these new drugs will change that. That would be exciting.
DHAKAL: Unfortunately, the real-world data, a lot [of which are] from the CIBMTR [Center for International Blood and Marrow Transplant Research] a few years ago, and [findings from] another paper around the same time showed autologous vs allogeneic transplant in plasma cell leukemia had no difference in the survival. We recently saw that more [patients] went to get transplant, perhaps because of better induction regimens than they used to get before 2015, but the survival of autologous vs allogeneic transplant was pretty much the same. In fact, [patients who underwent] allogeneic [transplant] did poorly compared [with those who underwent] autologous [transplant], though there was no direct head-to-head comparison because of the different patient populations. But survival was pretty much the same. These are the groups of patients who need all these new mechanisms of action with the immunotherapeutic targets.
DISCUSSION QUESTION
RAMADAS: The quick time that they start responding, at 1.2 months.2 I think that’s one. And it’s also durable.
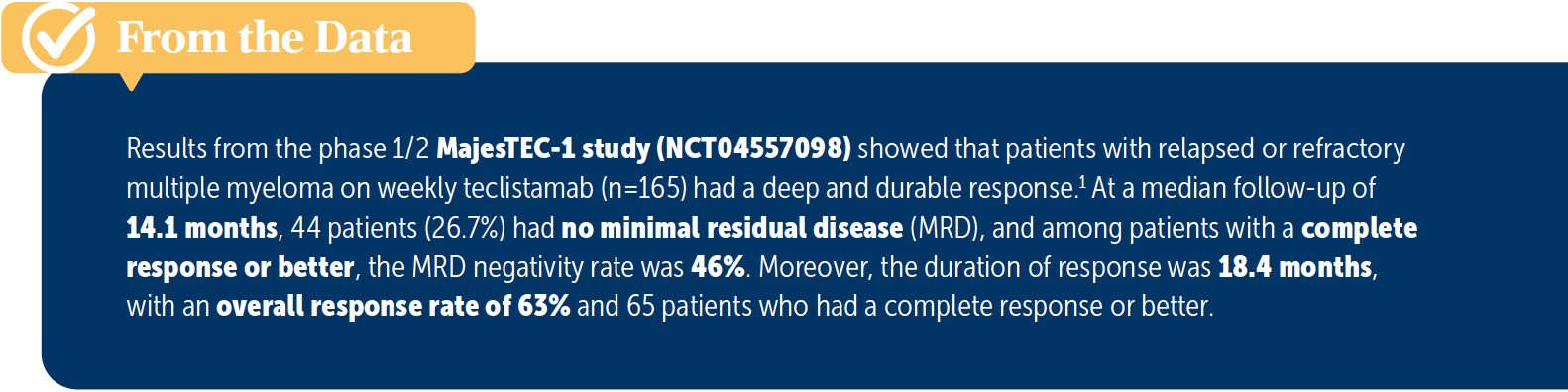
ABUTALIB: The response rate is good in these patients with highly refractory [disease], and MRD [minimal residual disease] negativity was achieved in 44 patients [From the Data1]. So I agree with my colleague about the rapid response. Also, we can use it in the older population.
CIOBANU: I have a question about administration. For this drug, patients must be inpatients?
DHAKAL: Yes, the FDA and the label say that you must hospitalize patients for the first step-up doses for 48 hours. For example, for your first dose, you must admit for 48 hours. The second dose, 48 hours. The final dose, which is the day 7 or 8 dose, 48 hours.
So admission is usually 7 to 10 days, depending on [whether] the patient develops CRS and you must delay it.3 So to answer your question, these patients will be hospitalized for the step-up doses. But after the step-up doses, then we do this at outpatient [care].
DISCUSSION QUESTION
What is your reaction to the safety data from the MajesTEC-1 trial, and how likely are you to administer teclistamab or refer the patient to another institution for it?
ABUTALIB: I’m comfortable with the safety data. The question I have, and maybe you can answer it, is that unless somebody is eligible for both CAR T cells and teclistamab and is not [older], how do you decide? From an efficacy standpoint, of course, they are not compared head-to-head. What about the cost of continuous therapy if they were to respond vs the 1-time cost of CAR T cells?
SHAH: I have a patient who just went for CAR T-cell evaluation. We’re [using cells from the] marrow, and she’s not responding, and we’ve got to figure out whether to do it or try teclistamab in the community setting. I don’t know [whether] someone would have to go to an academic center for teclistamab?
DHAKAL: That is a great question, and I don’t think we have an answer. Because as you already said, there are no head-to-head comparisons. Both products have pluses and minuses. CAR T-cell therapy, of course, is a one-and-done approach with a very high response rate, but that is if the patient received the CAR T cells.
Patients who couldn’t get it and progressed while they were waiting are not accounted for, so it probably depends on the patient preference and disease tempo. The disadvantage of treatment [such as] this, as with other myeloma treatments, is [that] it is continuous treatment [until] progression, so that adds to the quality-of-life issues, cost, and some long-term infections or other long-term adverse events.
If I have a patient who would meet the criteria for either of them, I discuss the pros and cons with the patient and see what the patient prefers. Some patients probably don’t want to travel and may not have good social support to stay near the CAR T-cell center for a month, so maybe [teclistamab] is a good option for them. The good thing is that both options are effective.
We didn’t have this kind of agent that can produce a single-agent response rate of [approximately] 70% in myeloma before. The [progression-free survival] of teclistamab is 11 months, which is comparable or maybe better than some of the CAR T cells that we have.1 So both are highly effective therapies, and I will have that discussion with the patient and see what the patient prefers.
REFERENCES
1. NCCN. Clinical Practice Guidelines in Oncology. Multiple myeloma, version 3.2023. Accessed April 21, 2023. https://bit. ly/41KZPMg
2. Moreau P, Garfall AL, van de Donk NWCJ, et al. Teclistamab in relapsed or refractory multiple myeloma. N Engl J Med. 2022;387(6):495-505. doi:10.1056/NEJMoa2203478
3. Tecvayli. Prescribing information. Janssen Biotech Inc; 2022. Accessed April 10, 2023. https://bit.ly/3KXhUzV
Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More