Data From the RESPONSE Studies Drive Ruxolitinib Use in Polycythemia Vera
The way I practice, personally, is that if they are older than 60 years, they are automatically high risk, and I will start hydroxyurea. In PV, being over 60 years and/or prior thrombosis automatically makes the patient high risk, so you should probably be starting a cytoreductive therapy.
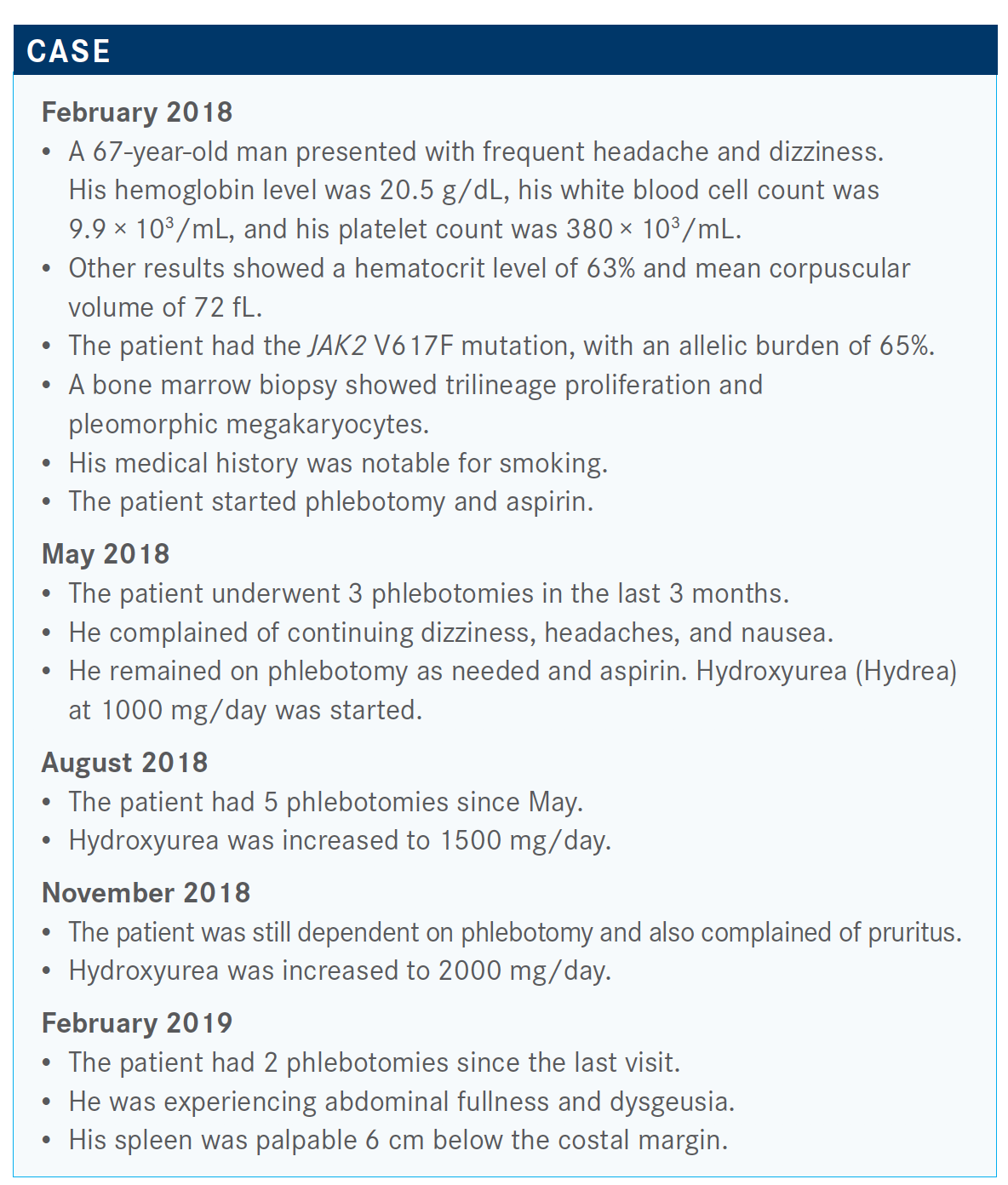
During a Targeted Oncology Case-Based Peer Perspectives Roundtable event, Prithviraj Bose, MD, associate professor, Department of Leukemia, Division of Cancer Medicine, The University of Texas MD Anderson Cancer Center, discussion the use of ruxolitinib (Jakafi) as treatment of polycythemia vera (PV).
Targeted OncologyTM: How do you assess risk and likeliness of response in patients with PV?
BOSE: The way I practice, personally, is that if they are older than 60 years, they are automatically high risk, and I will start hydroxyurea. In PV, being over 60 years and/or [having] prior thrombosis automatically makes the patient high risk, so you should probably be starting a cytoreductive therapy. Whether you like hydroxyurea or interferon doesn’t matter because they have been shown to be equivalent in a randomized comparative trial [NCT01259856]. Cytoreductive therapy should probably be started in anybody who is high risk, either by age or by thrombosis history.
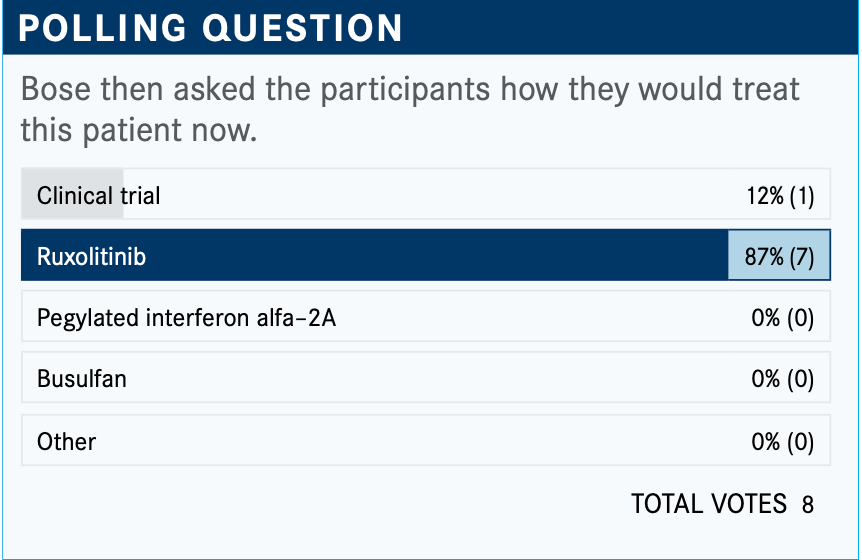
What do you think of the responses to this poll?
So 88% would do ruxolitinib and clinical trial is always an appropriate answer—13% would go for a clinical trial. Now, that space in PV is difficult because, for example, the MDM2 inhibitors were being developed for PV but they were too toxic, and [those trials] have been closed. So it’s hard to find a clinical trial for hydroxyurea-resistant or intolerant PV. You’re mainly left with ruxolitinib and interferon.
What drives your decision-making in this hydroxyurea-failure setting? Also, do you consider the National Comprehensive Cancer Network (NCCN) guidelines?
[In the NCCN guidelines, patients] who are over 60 years or have had a clot are automatically high risk.1 You start with cytoreductive therapy for those patients. For the low-risk population, you do phlebotomy and aspirin. But then, as you monitor them, there are certain things that may tell you that somebody needs cytoreductive therapy. [If] somebody is on phlebotomy and aspirin— let’s say they are 50 years old—they may still need cytoreductive therapy, even if they have not had a clot. If...they are intolerant of or resistant to hydroxyurea, you need to change to ruxolitinib or interferon; [so, for example,] if they have a new clot, disease- related bleeding, frequent phlebotomies, if they don’t tolerate the phlebotomy well, they are complaining about it, if the spleen is enlarging, or they have a high platelet count causing symptoms.
Platelet count elevation alone is not a problem unless that patient is above 1.5 million mL and they acquired von Willebrand disease, in which case there can be bleeding. But other than that scenario, [elevated] platelets alone are not a problem unless the patient is symptomatic. They can complain of migraines, headaches, or blurry vision from platelets. That can be a problem. If they have progressive leukocytosis, you’re not controlling the white blood cell count. You may be controlling the hematocrit, but you are not controlling the white count.
There are several goals in PV. The hematocrit needs to be under 45%; that is set in stone from the CYTO-PV trial [NCT01645124].2 Beyond that, there’s also white blood cell count control.
Which data support ruxolitinib in this setting?
The RESPONSE data [NCT01243944] resulted in a ruxolitinib approval.3 It’s been almost 5 years since it was approved. The RESPONSE trial [evaluated] ruxolitinib versus best available therapy. The patients were hydroxyurea resistant or intolerant. About 222 patients were randomized equally.
The composite primary end point was a combination of 2 things. Ruxolitinib versus standard therapy was about 21% versus 1% [for hematocrit control/spleen response]. But when you break up the composite primary end point into its 2 components—spleen and hematocrit control—there were differences there as well. Hematocrit control was 60% versus 20% and spleen was about 38% versus 1%.
Symptoms were controlled in about 49% versus 5% [of patients. For] individual symptoms, cytokine symptom clusters are things like muscle aches, itching, night sweats, weight loss, fever, hyperviscosities, headaches, blurry vision, shortness of breath, and chest pain. Splenomegaly is your early satiety, abdominal pain, et cetera.
All symptom [relief] favored ruxolitinib. Now, one interesting point about this study is that the standard therapy that most patients received was hydroxyurea, even though they were by definition hydroxyurea failures, because at the time there was nothing other than hydroxyurea, or at least there was nothing very good. So the majority, even in that setting of hydroxyurea failure, still got hydroxyurea as the standard therapy.
From the 5-year follow-up...at 224 weeks, which is around that 4 to 5 years, the probability of maintaining hematocrit control and spleen volume reduction was good, at 73% and 72%, [respectively].4
The probability of maintaining the complete hematologic response [CHR] at 5 years was 55%. CHR meant normal hemoglobin, normal platelets...hematocrit under 45%, controlled platelets, and controlled white [blood cell] count.
How does the RESPONSE trial compare with the RESPONSE-2 trial?
The RESPONSE-2 trial [NCT02038036] was conducted in Europe [and other locations around the world] and was identical to RESPONSE, except that splenomegaly was not a requirement [for patients’ participation].5 In fact, they could not have splenomegaly, so RESPONSE-2 was conducted in patients without splenomegaly. RESPONSE was conducted in patients with splenomegaly.
The numbers are strikingly similar. The hematocrit control was 60% versus 20% [for ruxolitinib vs best available therapy], roughly, in both trials. The symptom [control was] 45% versus 23% in RESPONSE-2 and 49% versus 5% in RESPONSE. So there’s a difference between standard therapy in the comparator arms, but the ruxolitinib arms are similar.
The CHR rate was 23% versus 5%, and 24% versus 9%, so, very similar. And of course, the spleen is not applicable in RESPONSE-2.
What were the toxicities in the RESPONSE trials?
What we care about in these patients—particularly with PV, which has a long median survival of about 19 years—are the adverse effects [AEs]. They have to be able to tolerate [ruxolitinib]. [Regarding] the anemia and thrombocytopenia, these patients have much better counts than patients with myelofibrosis, so they don’t get as anemic and thrombocytopenic. It’s not that much of a problem.4
Herpes zoster infection is important; these patients can [have their herpes] reactivate. In our practice, we give every patient on drugs the Shingrix vaccine [or killed vaccine], every patient. The earlier [vaccine] was the light attenuated one. You don’t want to give that to somebody on JAK inhibition. But the killed vaccine, we give all our patients 2 doses, 6 months apart because of this reason.
Now, the other thing to remember is nonmelanoma skin cancer; it’s a problem with hydroxyurea, and it’s a problem with ruxolitinib. If you have a patient who has a history of basal cell carcinoma or squamous cell carcinoma, they are at a higher risk of having a recurrence on ruxolitinib. Is that a reason not to do ruxolitinib? No, it’s not, but something to be aware of.
Finally...if you ask me what’s the most important end point in a trial in PV, I will say it’s clotting, because that’s what patients may die of, or that’s what you’re really trying to prevent. [The study results] showed that clotting was numerically better for ruxolitinib, but not statistically significant. Patients on ruxolitinib had [fewer] clots than the patients on standard therapy, but they did not reach statistical significance yet.
How have you been using ruxolitinib in PV?
I’ve never [used] it in front line, just because it’s not approved and there are no data. It’s not very common, especially if you have a general oncology practice, to run into a hydroxyurea-resistant intolerant PV, because it’s about 20% [of patients]. And again, if PV is not a big part of your practice, then that’s completely understandable.
Have patients been asking you what to do about their ruxolitinib or fedratinib (Inrebic) because of coronavirus disease 2019 (COVID-19)? Are they concerned about it?
I’ve been asked a couple of times. I say, “No, it should not impact our management.” But ruxolitinib is immunosuppressive in both JAK1 and JAK2. So JAK1 particularly is more important for immunosuppression. It’s an immunosuppressive drug. There can be opportunistic infections. But on the flip side, the JAK inhibitors are being studied as treatments for COVID-19, because they can calm down the inflammatory cascade and suppress the cytokine storm that often kills these patients. I think it can go both ways. I generally give patients both that warning and the reassurance. But I do not change anything.
The dosage of ruxolitinib for PV would be adjusted to get a hematocrit around 45%. Do you adjust it to get a spleen size reduction?
In PV, spleen [size reduction] is less important. It’s not that common. First of all, it’s not that common to have splenomegaly, which is why [investigators] conducted the RESPONSE-2 trial, because they wanted data in both settings. And we don’t have data [indicating] that spleen volume reduction means anything in PV the way it does in myelofibrosis. So no, I don’t target it for spleen volume reduction in PV. In PV, my goal is to get the hematocrit under 45% and keep it under 45%, control the white [blood] cells, and control the symptoms. In PV, the label says always start at 10 mg twice daily. I will go up as needed for those things, but not for spleen reduction.
REFERENCES
1. NCCN. Clinical Practice Guidelines in Oncology. Myeloproliferative neoplasms, version 1.2020. Accessed December 11, 2020. https://bit.ly/3gYt5at
2. Marchioli R, Finazzi G, Specchia G, Masciulli A, Mennitto MR, Barbui T. The CYTO-PV: a large- scale trial testing the intensity of CYTOreductive therapy to prevent cardiovascular events in patients with polycythemia vera. Thrombosis. 2011;2011:794240. doi:10.1155/2011/794240
3. Vannucchi AM, Kiladjian JJ, Griesshammer M, et al. Ruxolitinib versus standard therapy for the treatment of polycythemia vera. N Engl J Med. 2015;372(5):426-435. doi:10.1056/NEJMoa1409002
4. Kiladjian JJ, Zachee P, Hino M, et al. Long-term efficacy and safety of ruxolitinib versus best available therapy in polycythaemia vera (RESPONSE): 5-year follow up of a phase 3 study. Lancet Haematol. 2020;7(3):e226-e237. doi:10.1016/S2352-3026(19)30207-8
5. Passamonti F, Griesshammer M, Palandri F, et al. Ruxolitinib for the treatment of inadequately controlled polycythaemia vera without splenomegaly (RESPONSE-2): a randomised, open-label, phase 3b study. Lancet Oncol. 2017;18(1):88-99. doi:10.1016/S1470-2045(16)30558-7












