Campbell Discusses Choices for Patients With Favorable- and Intermediate-Risk RCC
During a Targeted Oncology™ Case-Based Roundtable™ event, Matthew T. Campbell, MD, MS, discussed data supporting frontline combination therapies for patients with favorable- and intermediate-risk clear cell renal cell carcinoma.
Matthew T. Campbell, MD, MS
Associate Professor
Associate Medical Director
Department of Genitourinary Medical Oncology
Division of Cancer Medicine
The University of Texas MD Anderson Cancer Center
Houston, TX

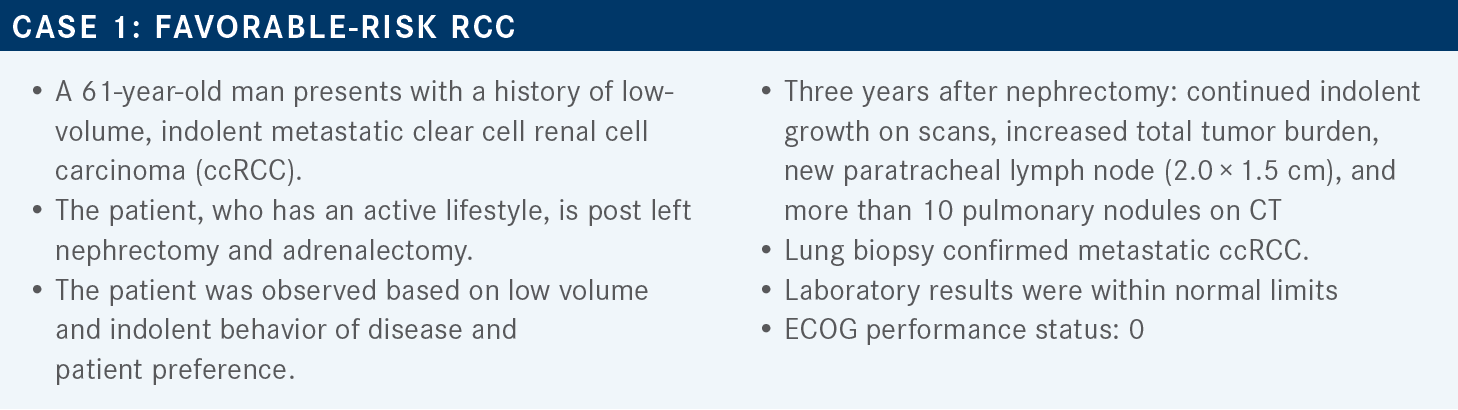
Targeted OncologyTM: What are the recommended first-line therapies for ccRCC based on the National Comprehensive Cancer Network (NCCN) guidelines?
CAMPBELL: [The NCCN guidelines split therapies based] on favorable risk and poor or intermediate risk.1 In the favorable-risk category, the 3 preferred regimens are axitinib [Inlyta] plus pembrolizumab [Keytruda], cabozantinib [Cabometyx] plus nivolumab [Opdivo], and lenvatinib [Lenvima] plus pembrolizumab.
Other recommended regimens are cabozantinib as a single agent, which is category 2B based on the CABOSUN study [NCT01835158].2 Then there is ipilimumab [Yervoy] plus nivolumab; and axitinib plus avelumab [Bavencio], as well as the older pazopanib [Votrient] and sunitinib [Sutent]. Under certain circumstances, one can use high-dose IL-2.
[I will summarize] the frontline combinations, when they were FDA approved, and the breakdown of use in favorable-, intermediate-, and poor-risk categories. I am going to go through each of the studies in more detail.
Percentage wise, the most favorable-risk patients were on axitinib/pembrolizumab followed by lenvatinib/pembrolizumab compared with [those in] the other studies. Both the CheckMate 214 [NCT02231749] with ipilimumab/nivolumab and the CheckMate 9ER [NCT03141177] with cabozantinib/nivolumab [had more] intermediate- and poor-risk patients. Very few poor-risk patients were on the CLEAR study [NCT02811861] with lenvatinib/pembrolizumab, which can have some influence on the outcome.
By far, CheckMate 214 has the most mature data, followed closely by KEYNOTE-426 [NCT02853331], and then more recently the CheckMate 9ER and the CLEAR studies. For overall survival [OS], the HRs are very similar across the studies. The CheckMate 9ER and CLEAR studies, I would say, are still unsettled in terms of median OS, and as these studies mature, these data are likely going to continue to shift.
Which data support the use of cabozantinib/ nivolumab as first-line therapy for patients with favorable-risk ccRCC?
The CheckMate 9ER trial was a randomized phase 3 trial. Patients had to have a clear cell component for participation. They allowed any IMDC [International Metastatic RCC Database Consortium] risk group.
They stratified based on IMDC risk score, tumor PD-L1 expression, and then geographic region. Geographic region is always important because of availability of agents at the time of progression. Patients were randomly assigned 1:1 to receive cabozantinib/nivolumab compared with sunitinib, which was dosed as it always is on these trials at 50 mg daily, 4 weeks on, 2 weeks off.
They were treated until progressive disease [PD] or unacceptable toxicity. The primary end point of the study was progression-free survival [PFS], and key secondary end points included OS, overall response rate [ORR], and safety.3 Nivolumab/cabozantinib satisfied the PFS at 16.6 months compared with 8.3 months with sunitinib [HR, 0.56; 95% CI, 0.46-0.68]. As the data have matured to date, the Kaplan-Meier curves remain separated.4 The OS with a 33-month median follow-up showed continued separation of the curves.
There was a tremendous amount of censoring after 24 months and so the farthest part of the curve was still a little bit murky, but it’s going to be an interesting follow-up. In this study, all subgroups were consistent with the overall effect.3
The ORR was 56% vs 28% [with nivolumab/cabozantinib vs sunitinib, respectively]. The complete response [CR] rate was 12% vs 5%, and the PD rate 6% vs 14%. When I normally look at the PD rate, I add the unable to determine group to it because a lot of these patients are progressing or are having some incident that happens prior to their initial restaging. When added together, it was about 12% vs 30% for sunitinib.4
What were the results of the post hoc and safety analyses in CheckMate 9ER?
The post hoc analyses looked at sites of metastases including liver, bone, and lung. The lungs are known to be a site that is less risky, except if one had a high burden of disease causing a lot of symptoms. Bone and liver metastases are known to be negative prognostic factors.
The PFS for liver metastases with cabozantinib/ nivolumab is 10.9 months vs 5.6 months for sunitinib. The HR is maintained, but you can tell it’s a negative prognostic site because both are worse than [those of] the overall group.
They were able to overcome, at least in the subgroup, that negative prognostic site in patients with bone metastasis, and they did substantially better than patients treated with sunitinib, with a PFS of 18.2 months vs 4.4 months. For lung metastases, it’s what you’d anticipate with the general population, a PFS of around 16.8 months vs 8.2 months, respectively.5
The safety profile is what you would anticipate with an immuno-oncology [(IO) drug] plus a tyrosine kinase inhibitor [TKI]. There is diarrhea with cabozantinib—majority grade 1 and 2—hand-foot syndrome, hypertension, and fatigue. For the treatments leading to discontinuation, 11% of patients discontinued nivolumab, 9% discontinued cabozantinib, and then around 8% discontinued both.
In the sunitinib arm, the discontinuation rate was 10%. Approximately half the patients in each arm had at least 1 dose reduction, which tells you that a good portion of patients who start off on cabozantinib 40 mg had to go down to 20 mg.4
How do the CheckMate 9ER data compare with those of the previous studies you mentioned?
For the efficacy overview between all these different trials, there is a CR difference between the combinations vs sunitinib. The ORR is basically numerically similar for ipilimumab/nivolumab vs sunitinib, a significant 20% improvement with axitinib/pembrolizumab, and then a doubling with the CheckMate 9ER and CLEAR trials.3,6-8
As one would anticipate with any targeted agent, you’re going to have some treatment-related adverse events [TRAEs]. Nearly all patients had a TRAE. Numerically, ipilimumab/nivolumab had the lowest number of high-grade toxicities, as IO therapies are a bit different compared with TKIs. The CLEAR study had 72% with grade 3 toxicities or higher. The lowest discontinuations numerically were with the cabozantinib/nivolumab. High-dose corticosteroid use was not reported in the CLEAR study. In the CheckMate 214 study, 30% of patients required steroids at some point.6,8
The quality-of-life surveys that were completed were somewhat different between groups. All the 3 TKI/IO studies did the EQ-5D-3L survey. Cabozantinib had an improvement compared with sunitinib, whereas the other studies’ [data showed] a very similar quality of life between the combination and sunitinib.
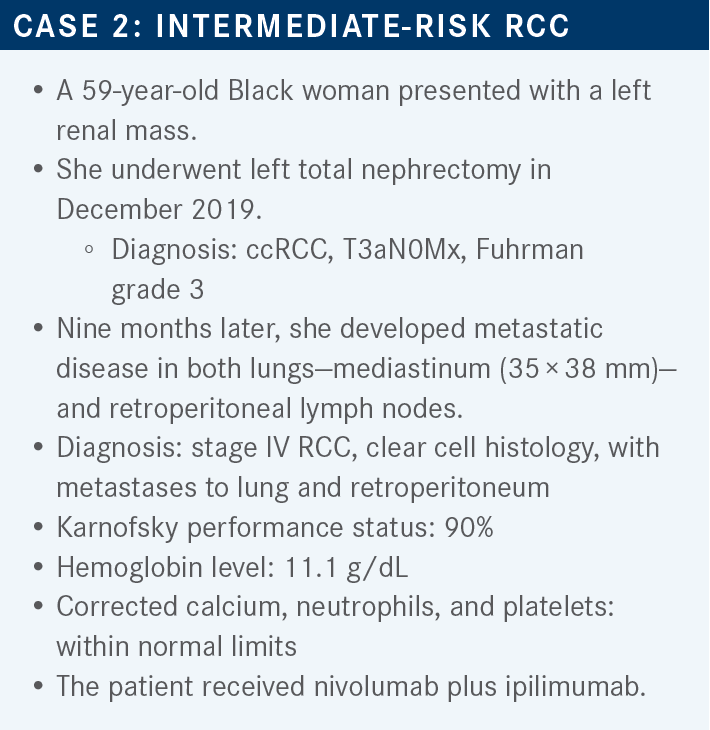
Which data support the use of nivolumab/ ipilimumab as first-line therapy for patients with intermediate-risk ccRCC?
In the CheckMate 214 trial design, patients had to be treatment naïve, have a clear cell component, measurabledisease, and acceptable ECOG performance status. They were stratified based on IMDC score and region. They were [randomly assigned] to either 4 doses of nivolumab 3 mg/kg plus ipilimumab 1 mg/kg every 3 weeks followed by maintenance nivolumab 3 mg/kg every 2 weeks, or the usual sunitinib dosing.
The primary end points were ORR, PFS, and OS in the intermediate- or poor-risk groups. The secondary end points were the ORR, PFS, and OS in any risk group. Patients were treated until PD or unacceptable toxicity and were allowed to discontinue maintenance nivolumab past 2 years of the study.6
The data available are after 67.7 months of follow-up. For the OS in the intermediate- and poor-risk group, 43% of patients who received ipilimumab/nivolumab were still alive at 5 years vs 31% of those who received sunitinib. The median OS was 47.0 months vs 26.6 months, respectively.
For the PFS, there was a near flattening of the curve that happened right around the 30- to 36-month mark, with around 31% of patients not having experienced progression at 5 years with nivolumab/ipilimumab, and 11% of patients in the sunitinib group. The ORR was 41% vs 34% with the intermediate- and poor-risk groups.6
What were the responses among the different subgroups in CheckMate 214?
In the subgroups, the ORR is numerically lower in the favorable-risk group with nivolumab plus ipilimumab, though there is still a 13% CR and 17% partial response rate. The favorable-risk group ORR was impressive, with sunitinib at 52%. There’s been a lot of work in this area, and there is a high angiogenic score for patients in this favorable category compared with the intermediate- or poor-risk groups where it’s more of an immunogenic signature.
There is clearly something interesting in this subgroup. The intermediate- and poor-risk groups had a lower response rate at 27% for sunitinib vs 42% for the combination.6 Some studies have looked at this, and every study uses different signatures, which makes it complicated.
There’s been this recurring theme where an angiogenic signature predicts a longer response to a TKI, and a good portion of these patients are in the favorable-risk category. So a TKI-based strategy for favorable-risk groups can be a good option.
The studies that are all intention-to-treat population are not splitting out their favorable-risk population as much. But TKIs have performed very well in that subgroup compared with the combinations in the different trials. These patients tend to be sensitive to TKI-based treatment. The more aggressive the disease is, the more it tends to have an immunogenic signature where immunotherapy may play a more important role.
How did patients do in terms of toxicity with nivolumab/ipilimumab?
As you would anticipate with ipilimumab-based treatment, there is diarrhea, which is different from the diarrhea that you experience with sunitinib. Patients clearly require work-up to make sure they’re not experiencing immune-induced diarrhea. Diarrhea with sunitinib typically resolves quickly with dose holds and adjustments, and fatigue was seen in 37.8% of patients in the combination arm.
In my experience, pruritis and skin rash are extraordinarily common with IO-based treatment, as well as hypothyroidism. The longer one is on these treatments, the more likely they are to have thyroid issues. In the study, 31% of patients had to discontinue nivolumab/ipilimumab, and 54% of patients required at least a dose break or interruption for an adverse reaction.
What are the data behind a triplet IO/IO/TKI combination vs a doublet IO combination?
[Data from] the COSMIC-313 trial [NCT03937219] were presented at the 2022 ESMO [European Society for Medical Oncology] conference. This was the first time we’ve had a randomized trial with one of the new combinations as the comparator. Patients had to have a clear cell component, be intermediate or poor risk, and have measurable disease.
They were randomly assigned to a triplet of cabozantinib 40 mg, nivolumab 3 mg/kg, and ipilimumab 1 mg/kg for 4 cycles, and then they continued on cabozantinib plus nivolumab, vs nivolumab/ipilimumab plus placebo at the standard RCC dosing followed by maintenance nivolumab with a placebo pill.9 The PFS was the primary end point and the key secondary end point was OS. About 75% of patients had intermediate-risk disease, the median age was 61, and two-thirds had a prior nephrectomy, which tends to mean that this was a more ill population. The triplet had not reached PFS, [whereas] nivolumab/ipilimumab/placebo hit 11.3 months [HR, 0.73; 95% CI, 0.57-0.94; P = .013]. The CR rate was 3% in each arm, and PD 8% in the triplet and 20% with nivolumab/ipilimumab only.
The disease control rate was 14 percentage points higher with the triplet. The rate of grade 3 and 4 TRAEs was numerically higher with the addition of a TKI. There was a higher rate of elevated liver transaminases, diarrhea, and TKI-associated toxicities. In both arms, 1% of patients had a grade 5 event and [died]. Corticosteroid use was 58% in the triplet arm vs 35% with the placebo/nivolumab/ipilimumab.
REFERENCES
1. NCCN. Clinical Practice Guidelines in Oncology. Kidney cancer, version 4.2023. January 18, 2023. Accessed January 25, 2023. https://bit.ly/3RbPK6X
2. Choueiri TK, Halabi S, Sanford BL, et al. Cabozantinib versus sunitinib as initial targeted therapy for patients with metastatic renal cell carcinoma of poor or intermediate risk: the Alliance A031203 CABOSUN trial. J Clin Oncol. 2017;35(6):591-597. doi:10.1200/JCO.2016.70.7398
3. Choueiri TK, Powles T, Burotto M, et al; CheckMate 9ER Investigators. Nivolumab plus cabozantinib versus sunitinib for advanced renal-cell carcinoma. N Engl J Med. 2021;384(9):829-841. doi:10.1056/NEJMoa2026982
4. Powles T, Choueiri TK, Burotto M, et al. Final overall survival analysis and organ-specific target lesion assessments with two-year follow-up in CheckMate 9ER: nivolumab plus cabozantinib versus sunitinib for patients with advanced renal cell carcinoma. Poster presented at: 2022 American Society of Clinical Oncology Genitourinary Cancers Symposium; February 17-19, 2022; San Franscico, CA. Accessed February 2, 2023. https://bit.ly/3XRuNAR
5. Apolo AB, Powles T, Burotto M, et al. Nivolumab plus cabozantinib (N+C) versus sunitinib (S) for advanced renal cell carcinoma (aRCC): outcomes by baseline disease characteristics in the phase 3 CheckMate 9ER trial. J Clin Oncol. 2021;39(suppl 15):4553. doi:10.1200/JCO.2021.39.15_suppl.4553
6. Motzer RJ, Tannir NM, McDermott DF, et al. Conditional survival and 5-year follow-up in CheckMate 214: first-line nivolumab + ipilimumab (N + I) versus sunitinib (S) in advanced renal cell carcinoma (aRCC). Ann Oncol. 2021;32(suppl 5):S678-S724. doi:10.1016/annonc/annonc675
7. Rini BI, Plimack ER, Stus V, et al. Pembrolizumab (pembro) plus axitinib (axi) versus sunitinib as first-line therapy for advanced clear cell renal cell carcinoma (ccRCC): results from 42-month follow-up of KEYNOTE-426. J Clin Oncol. 2021;39(suppl 15):4500. doi:10.1200/JCO.2021.39.15_suppl.4500
8. Motzer R, Alekseev B, Rha SY, et al; CLEAR Trial Investigators. Lenvatinib plus pembrolizumab or everolimus for advanced renal cell carcinoma. N Engl J Med. 2021;384(14):1289-1300. doi:10.1056/NEJMoa2035716
9. Choueiri TK, Powles TB, Albiges L, et al. Phase III study of cabozantinib (C) in combination with nivolumab (N) and ipilimumab (I) in previously untreated advanced renal cell carcinoma (aRCC) of IMDC intermediate or poor risk (COSMIC-313). Ann Oncol. 2022;33(suppl 7):S808-S869. doi:10.1016/annonc/annonc1089

Enhancing Precision in Immunotherapy: CD8 PET-Avidity in RCC
March 1st 2024In this episode of Emerging Experts, Peter Zang, MD, highlights research on baseline CD8 lymph node avidity with 89-Zr-crefmirlimab for the treatment of patients with metastatic renal cell carcinoma and response to immunotherapy.
Listen
Beyond the First-Line: Economides on Advancing Therapies in RCC
February 1st 2024In our 4th episode of Emerging Experts, Minas P. Economides, MD, unveils the challenges and opportunities for renal cell carcinoma treatment, focusing on the lack of therapies available in the second-line setting.
Listen