Roundtable Discussion: Ailawadhi Compares Therapies in Newly Diagnosed Multiple Myeloma
During a Targeted Oncology™ Case-Based Roundtable™ event, Sikander Ailawadhi, MD, discussed with participants the choice of regimen for a patient with transplant-eligible newly diagnosed multiple myeloma.
Sikander Ailawadhi, MD
Professor of Medicine
Lead, International Cancer Center Division of Hematology/Oncology Mayo Clinic
Jacksonville, FL

CASE SUMMARY
A 54-year-old woman presented with Revised International Staging System stage II multiple myeloma.
- Status:
- Hemoglobin, 7.0 g/dL; β2-microglobulin, 6 mg/L; albumin, 3.2 g/dL
- Calcium 11.3 mg/dL; lactate dehydrogenase, 200 U/L; creatinine clearance, 45 mL/min
- Bone marrow: 22% clonal plasma cells
- Serum κ free light chains: 24 mg/dL
- Serum monoclonal protein: 5 g/dL
- Cytogenetic (fluorescence in situ hybridization and karyotyping) abnormalities: None
- ECOG performance status: 1
- PET-CT scan: multiple bone lesions in vertebrae
There was no extramedullary disease, and she received a diagnosis of IgG-κ multiple myeloma. She was told she was transplant eligible.
DISCUSSION QUESTION
What would make you choose between a quadruplet and a triplet regimen for patients with transplant-eligible newly diagnosed myeloma?
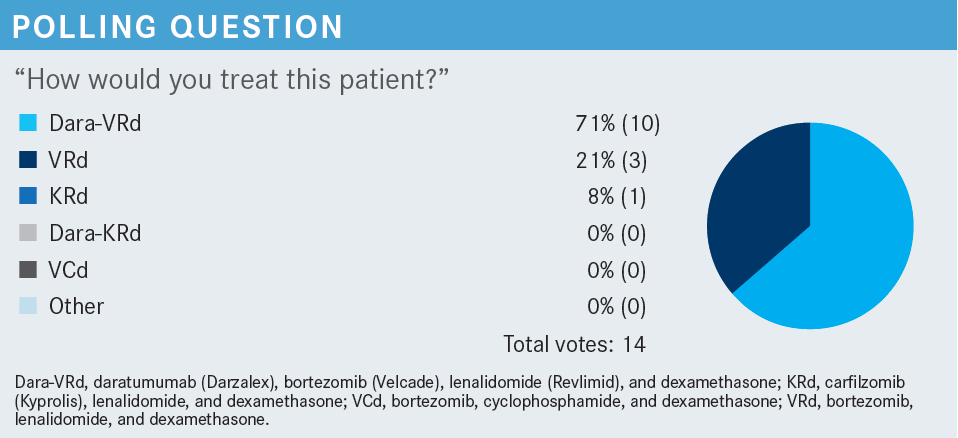
ZAIDEN: We know that getting the best response up front, for a lot of these patients, is typically one of the best shots they have. We have had a lot of studies recently, such as the MAIA trial [NCT02252172] or ALCYONE [NCT02195479] trial, that showed benefit from quadruplets, especially with Dara-VRd [daratumumab (Darzalex), bortezomib (Velcade), lenalidomide (Revlimid), and dexamethasone].1,2 I didn’t see anything in the patient’s presentation that would preclude being aggressive up front, and that’s why I went with Dara-VRd.
AILAWADHI: Any other thought, somebody who thought that a triplet would be appropriate? I don’t think there’s any wrong or right answer.
DANDAMUDI: Although there are data for 4-drug regimens, we need more data to make sure that they have overall survival [OS] benefit compared with the 3-drug regimens. That’s the reason I chose the triplet.
AILAWADHI: I was on a separate call where we’re looking at developing some content, and this was a question asked by a clinician who does not focus on myeloma but is on the panel of advisers for American Society of Clinical Oncology: “If you don’t have an OS benefit, is progression-free survival [PFS] benefit good enough?” I don’t think there’s any certain answer, but that is a good point.
However, I’ll add a caveat to that. I’ve heard this every now and then from counterparts, clinicians, and sometimes patients: “Well, let’s start with 3 drugs, and if in 2 cycles I don’t see a good enough response, I’ll add the fourth,” or “Let me start with 4; I’ll get a couple of cycles in; if the patient has any issues with tolerability, then I’ll go down to 3.”
Keep in mind that when we have a triplet regimen in a clinical trial, a patient who starts on a triplet stays on a triplet. If it’s a quadruplet regimen and they have an adverse event, there are dose-reduction guidelines for what to reduce at what time, rather than take away one of the drugs.
Would you start with a triplet and add a fourth drug if needed? Or vice versa: Would you start with a triplet, commit to a triplet; or start with a quadruplet, commit to a quadruplet?
GROSSET: I don’t do that, but I don’t think that there’s anything wrong with that strategy—although what exactly defines a “good enough response” is always arguable, I suppose. I personally don’t use the strategy, but just because the trials didn’t do it, I don’t think that means that it’s wrong.
AILAWADHI: I think that’s a reasonable point....Frankly, most of that is being done based on minimal residual disease [MRD] testing.
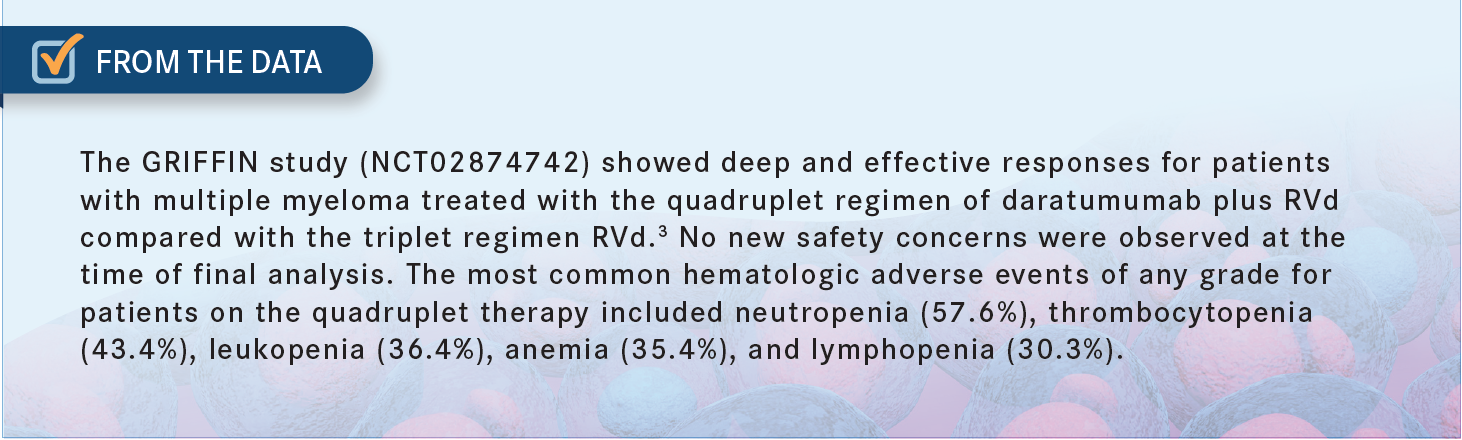
ZAIDEN: I would add that we know quadruplets give you a better and deeper response, from the GRIFFIN study [NCT02874742].3 If I’m looking to get somebody to transplant, that is my initial rationale for starting with a quadruplet, assuming that there are no toxicity or intolerability signals [From the Data3].
AILAWADHI: One other question that I would ask is, what do you consider an adequate or successful treatment response in your patients following induction therapy?
The point that I would like to clarify, or gain some insight into, is: Should everybody get 4 cycles of induction and go to transplant, if they are going to transplant? Or do they have to achieve VGPR [very good partial response] or better? Do they have to achieve a complete response? Do they have to achieve MRD-negative status? What is your deciding factor?
I have also seen, every now and then, that a patient will start on a regimen and 2 cycles later they are told, “Well, your response is not good enough, let’s switch,” let’s say, hypothetically, “the VRd to KRd [carfilzomib (Kyprolis), lenalidomide, and dexamethasone].” I’m just throwing it out as a random point. What do you think is the best response for induction: Is it time, or is it depth? And, if it is depth, what would you be looking for?
DOSHI: It depends on the transplant center, too; we are usually in touch with them. We mostly do the related blood tests, like serum protein electrophoresis, light chains, etc. And if the patient is responding nicely, M-spike has gone down, they go to the transplant [team] for reevaluation. Most of the time, they end up doing the bone marrow biopsy, and then they either decide to take the patient to transplant or say, “We are not happy with this, give this drug,” and then the patient comes back to us.
KATOCH: The concept of MRD is difficult to evaluate in the community setting. I’ve done it on 1 patient, and it was so complicated, so I don’t know the answer to that, but I concur with the previous speaker that that’s what we’ve been doing. If the patient has some response or a VGPR, you let them see the transplant surgeon and take it from there.
AILAWADHI: Sounds good: VGPR or better. That’s fair, and hopefully the patient is seeing the transplant center sooner rather than later. Now, should we consider not transplanting, even if a patient is transplant eligible?
NGUYEN: Transplant, but it doesn’t have to be up front; it can be a delayed transplant.
AILAWADHI: Excellent thought. We must qualify that with a couple of things. When we talk about delayed transplant, the delay could mean the second line instead of the first line, or the delay could mean deferring to the future. There are data that show that delaying the transplant—to the future, significantly later—provides less benefit from the transplant. Those patients tend to do worse, when compared [with] transplanting up front.
We’ve looked at some of our own data at Mayo Clinic, where we compared first line and second line, and we didn’t see much of a difference in PFS or outcomes. It was a retrospective look, so we were able to extrapolate for [OS] also, and we didn’t see much of a difference.
Frankly speaking, in the literature there is nothing comparing first- and second-line transplant. It is first-line transplant compared with no transplant, or first-line transplant compared with much-delayed transplant, and in both those comparisons, the transplant arm does better.
NGUYEN: Right now, with the 4-drug combination—with which you can get MRD and sustain MRD—the question is, “Do we need to do transplant immediately?”
AILAWADHI: Excellent question, but I don’t think we have an answer. My colleague Dr Parrondo and I are debating this question. We’re trying to come up with a clinical trial design [that addresses the question]: If somebody goes into an MRD-negative state with induction, do they need to get a transplant right then, or can they defer it? I don’t believe anybody has the answer. Dr Parrondo, I know you’ve looked at these data. Any thoughts around that, or anything that you’ve come across that has tried to answer this question?
PARRONDO: Again, the question of the MRD [being] below the limit of detection—we don’t know if there is residual disease there. If you’re MRD 10–5, 10–6, what about 10–9, right? If they’re MRD negative after induction and you do the transplant, do you eradicate more disease? We don’t know the answer to that; we must do a trial to figure it out.
AILAWADHI: Again that’s a great question, but I don’t think anybody has a definitive answer. When patients come to us for a transplant discussion and they are in an MRD-negative state—at least over here at Mayo Clinic in Florida—we tell them, “I do not have an objective, incremental benefit that I can prove to you based on a study. We think you will benefit by getting a transplant right now, but I do not have a number that I can quote for you,” unlike somebody who is going to a transplant in an MRD-positive state.
That brings out this nuance that we don’t have an answer to: Should we be transplanting somebody who is MRD-negative with induction right away, or could we defer that? We don’t have the answer.
But short of that, what is your experience? You come from a different group of practices. It’s a very heterogeneous group that we have today. Any experience or thoughts about why a patient may or may not go to transplant? Do you tell a patient, “You should go to transplant” as a standard, but the patient doesn’t go? Or the patient doesn’t get the transplant eventually? Any thoughts around that?
We know from the Center for International Blood and Marrow Transplant Research data that in the [United States], only 20% to 25% of patients who are considered transplant eligible—based on data, not looking at an individual patient—end up going to a transplant center, even for the consult.
Out of those who get to the center, the majority get a transplant; but the majority [of eligible patients] don’t go to the center. Any experience around that?
YELLU: I discuss with all my patients whom I feel are transplant eligible that they might need to get a transplant at some point. If they’re young and have overall good performance status, usually they [like the idea of it], but we’ll have a detailed discussion—this transplant is not something super serious, like we do, like allogeneic. If you have a good discussion, usually most of the patients will accept it and see the transplant [team]. I haven’t had any issues.
KATOCH: I’ve had somewhat of a different experience. I think some of my patients, who are doing so well on their current therapy, feel like, “Why should I go through this when I’m doing so well?” I’ve had people who’ve gone and then have come back and said, “No, I’m going to reserve it for later.”
AILAWADHI: I think that’s a fair point. It’s important to have the discussion with the patient. We typically share with them that if they get the transplant now, vs not getting the transplant, that their [PFS may be longer]— and explaining that, and the benefit of that, is a little tricky, because then the patient asks, “Oh, so it’s going to make me live longer?” [I say,] “No, that’s not the case. We don’t know that, but at least, hopefully, it will make you live longer before the disease comes back.”
When the patients ask that question about second-line transplant, again, that is not a definitively answered question in trials. We’re hoping that we’ll be able to do some studies to prove it.
REFERENCES
1. Facon T, Kumar S, Plesner T, et al; MAIA Trial Investigators. Daratumumab plus lenalidomide and dexamethasone for untreated myeloma. N Engl J Med. 2019;380(22):2104-2115. doi:10.1056/NEJMoa1817249
2. Mateos MV, Dimopoulos MA, Cavo M, et al; ALCYONE Trial Investigators. Daratumumab plus bortezomib, melphalan, and prednisone for untreated myeloma. N Engl J Med. 2018;378(6):518-528. doi:10.1056/ NEJMoa1714678
3. Voorhees PM, Kaufman JL, Laubach J, et al. Daratumumab, lenalidomide, bortezomib, and dexamethasone for transplant-eligible newly diagnosed multiple myeloma: the GRIFFIN trial. Blood. 2020;136(8):936-945. doi:10.1182/ blood.2020005288

Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More