Atezolizumab Is Linked to Improvement in DFS in Early-Stage NSCLC
Adjuvant treatment with atezolizumab led to a significant improvement in disease-free survival versus supportive care in patients with PD-L1–positive non–small cell lung cancer.
Heather A. Wakelee, MD

Adjuvant treatment with atezolizumab (Tecentriq) led to a significant improvement in disease-free survival (DFS) vs supportive care in patients with PD-L1–positive non–small cell lung cancer (NSCLC). Findings from the phase 3 IMpower010 trial (NCT02486718) were presented at the 2021 American Society of Clinical Oncology Annual Meeting.
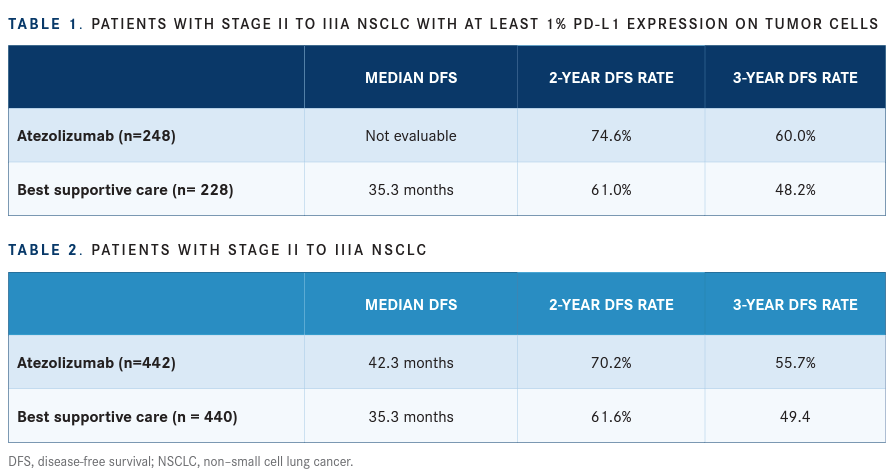
In patients with stage II to IIIA NSCLC with at least 1% PD-L1 expression on tumor cells, the median DFS was not evaluable ([NE]; 95% CI, 36.1-NE) with atezolizumab (n = 248) vs 35.3 months with best supportive care (n = 228; 95% CI, 29.0-NE; HR, 0.66; 95% CI, 0.50-0.88; P = .004). The 2-year DFS rate was 74.6% with atezolizumab vs 61.0% with best supportive care, and 3-year rates were 60.0% and 48.2%, respectively (TABLE 1).
In patients with stage II to IIIA NSCLC, the median DFS was 42.3 months with atezolizumab (n = 442; 95% CI, 36.0-NE) vs 35.3 months with best supportive care (n = 440; 95% CI, 30.4-46.4; HR, 0.79; 95% CI, 0.64-0.96; P = .02). The 2-year DFS rate was 70.2% with atezolizumab vs 61.6% with best supportive care, and 3-year rates were 55.7% and 49.4%, respectively (TABLE 2).
“Though surgery can cure some patients with early- stage lung cancer, disease recurrence is still very common,” said lead study author Heather A. Wakelee, MD, a thoracic specialist, professor of medicine, and chief of the Division of Oncology at Stanford University Medical Center, and deputy director of the Stanford Cancer Institute. “Until this trial, the only treatment that was known to help reduce that risk for most patients was chemotherapy, or osimertinib [Tagrisso] for the small group of patients with tumors with an EGFR mutation. These data show that personalized medicine with atezolizumab can reduce the chance of NSCLC returning after surgery for patients who have a tumor that expresses the biomarker PD-L1.”
Despite the progress that has been made for patients with early-stage disease who harbor EGFR sensitizing mutations, the standard of care remains platinum-based chemotherapy for most patients with resected NSCLC.
To be eligible for enrollment in the IMpower010 trial, patients had to have completely resected stage IB to IIIA NSCLC. Stage IB tumors had to be at least 4 cm. Additionally, patients had to have an ECOG performance status of 0 or 1, a lobectomy or pneumonectomy, and tumor tissue for PD-L1 analysis.
Following 1 to 4 cycles of cisplatin plus pemetrexed, gemcitabine, docetaxel, or vinorelbine (n = 1280), patients were randomized 1:1 to 1200 mg of atezolizumab every 21 days for 16 cycles (n = 1005) or best supportive care (n = 1005). No crossover was allowed.
Investigator-assessed DFS in patients with stage II to IIIA disease and PD-L1 expression of at least 1% on tumor cells per the SP263 assay, all randomized patients with stage II to IIIA disease, and the intention-to-treat (ITT) population with stage IB to IIIA disease served as the primary end point.
Key secondary end points included overall survival (OS) in the ITT population and DFS in the PD-L1high population.
Hierarchical statistical testing was organized such that positive DFS in the PD-L1–positive population would allow for DFS analysis in the stage II to IIIA population. This was followed by DFS analysis in the ITT population, which in turn was followed by OS analysis in the ITT population.
In patients with stage IB to IIIA NSCLC, the statistical significance boundary for DFS was not crossed with atezolizumab vs best supportive care. The median DFS was NE with atezolizumab (n = 507; 95% CI, 36.1-NE) vs 37.2 months with best supportive care (n = 498; 95% CI, 31.6-NE; HR, 0.81; 95% CI, 0.67-0.99; P = .04). The 2-year DFS rate was 71.4% with atezolizumab vs 63.6% with best supportive care. The 3-year DFS rates were 57.9% and 52.6%, respectively.
Regarding safety, all-grade adverse effects (AEs) occurred in 92.7% of patients in the atezolizumab arm (n = 495) vs 70.7% of patients in the best supportive care arm (n = 495). Of these AEs, 21.8% in the atezolizumab arm and 11.5% in the best supportive care arm were grade 3 or 4.
Grade 5 treatment-related AEs occurred in 0.8% and 0% of patients in the atezolizumab and best supportive care arms, respectively. AEs leading to treatment withdrawal occurred in 18.2% and 0% of patients, respectively.
Planned analyses of DFS and OS in the ITT population will continue with longer follow-up.
“For the first time, we are seeing that an immunotherapy is effective when used to treat early-stage lung cancer. The IMpower010 trial demonstrates that, for certain patients, atezolizumab can delay progression to advanced disease and perhaps even the need for more aggressive therapy. This could be an important advance in our understanding of immunotherapy and a step forward for many patients with lung cancer,” concluded Julie R. Gralow, MD, FACP, FASCO, chief medical officer and executive vice president at ASCO.
Reference
Wakelee HA, Altorki NK, Zhou C, et al. IMpower010: primary results of a phase III global study of atezolizumab versus best supportive care af-ter adjuvant chemotherapy in resected stage IB-IIIA non-small cell lung cancer (NSCLC). J Clin Oncol. 2021;39(suppl 15):8500. doi:10.1200/JCO.2021.39.15_suppl.8500