And the Award for Most Inspiring Lecture at ASH Goes to…
Ongoing and future trials will attempt to demonstrate the benefi t of NK cell therapies in lymphomas, multiple myeloma, sarcomas, and glioblastoma multiforme, among others.
John M. Burke, MD
Hematologist and Medical Oncologist
Rocky Mountain Cancer Centers
Associate Chair
US Oncology Hematology
Research Program
Aurora, CO

In December, I spent time in beautiful San Diego at the annual meeting of the American Society of Hematology (ASH). During the meeting, but from a different city in Southern California, the nominees for the 81st annual Golden Globe Awards were announced, with Barbie and Oppenheimer each scoring many nominations. With Hollywood’s awards season approaching, I ask myself, “Who should win the award for the most inspiring lecture given at ASH?” And I know immediately who would get my vote.
The award for the most inspiring lecture at ASH goes to…Katy Rezvani, MD, PhD, who gave a lecture entitled “Natural Killer Cells: A New Frontier for Cancer Immunotherapy,” as she accepted the E. Donnall Thomas Lecture and Prize. Dr Rezvani provided a masterful explanation of how her current work to develop natural killer (NK) cell therapies evolved from decades of research into bone marrow transplantation, graft-vs-leukemia effect, chimeric antigen receptor (CAR) T-cell therapy, and NK cell biology.
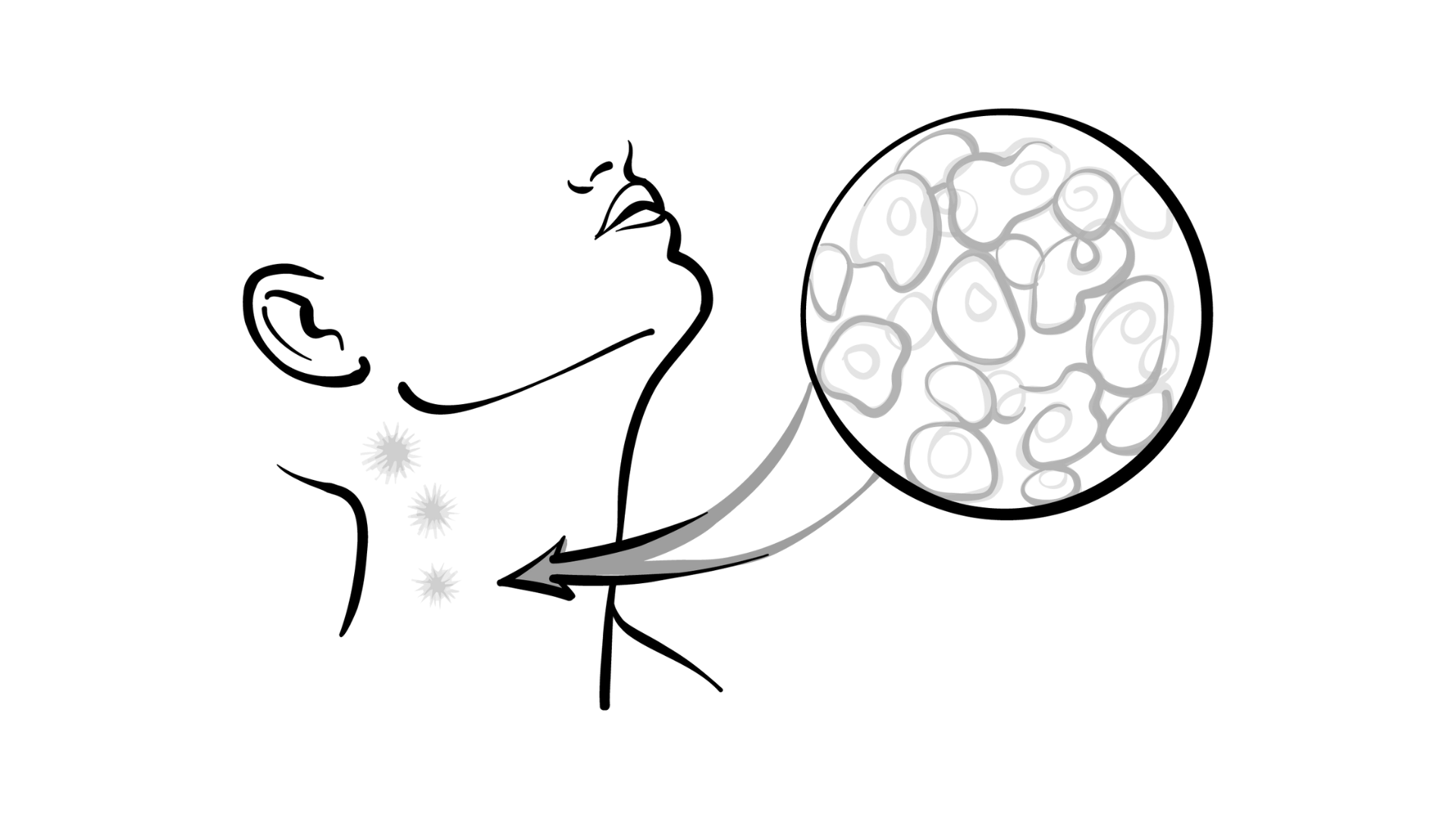
NK cell therapies have tremendous promise to treat cancer, both liquid and solid. They have on their surfaces receptors that permit differentiation of normal from abnormal cells. NK cells offer several potential advantages over T cells as therapies for cancer. The killing of target cells can be mediated not only by the transduced CAR but also by endogenous receptors on the NK cell surface. The presence of CD16 on their surface is critical for antibody-dependent cellular cytotoxicity. Allogeneic NK cells do not cause graft-vs-host disease. Many therapeutic doses can be manufactured from a single donor, thereby lowering cost and permitting “off the shelf” availability. NK cells have a favorable adverse effect profile, as they do not cause cytokine release syndrome or neurological toxicity.
Development of NK cell therapies has not been without challenges, of course. NK cells survive for only about a week if given without exogenous support. The quality of NK cells from different donors can vary. How best to modify NK cells to permit maximum killing of target tumor cells remains a work in progress; success will require determining the most effective combination of CARs and endogenous antigens on the surface of the NK cells.
Ongoing and future trials will attempt to demonstrate the benefi t of NK cell therapies in lymphomas, multiple myeloma, sarcomas, and glioblastoma multiforme, among others.