Yu Highlights Possible Sequencing Strategies in mCRPC
In a presentation delivered at the 2022 Large Urology Group Practice Association Annual Meeting, Evan Y. Yu, MD, discussed different sequencing strategies that can be utilized for patients with mCRPC and the data that support each approach.
With several novel hormonal agents (NHAs) approved for use in metastatic castration-resistant prostate cancer (mCRPC), sequencing strategies are increasingly being used to consider whether these agents can be switched at progression or whether other agents would be better.
“Combination therapy for mCRPC has generally been unremarkable, [although we have seen] early hits for combining NHAs with PARP inhibitors,” said Evan Y. Yu, MD, a professor in the Clinical Research Division and the clinical research director of genitourinary medical oncology at Fred Hutchinson Cancer Center. “There are many options for patients who progress on an NHA, but [several factors go] into the equation [of what to do next].... There is no definitive pathway. Patient individualization, comorbidities, and clinical judgement need to be applied to every situation.”
In a presentation delivered at the 2022 Large Urology Group Practice Association (LUGPA) Annual Meeting, Yu, who is also medical director of clinical research support of the Fred Hutchinson Cancer Research Consortium, discussed different sequencing strategies that can be utilized for patients with mCRPC and the data that support each approach.1
Pathway for Patients Who Receive Frontline NHAs and Progress
For patients with mCRPC who received NHAs such as abiraterone acetate (Zytiga) or enzalutamide (Xtandi) in the first-line setting, Yu said the top second-line options are docetaxel or radium Ra 223 dichloride (Xofigo). This is in cases where the patient has bone metastases, does not have visceral metastases, and is symptomatic.
“If you have patients who have mismatch-repair alterations, hypermutation, or microsatellite instability, pembrolizumab [Keytruda] can be used here,” Yu noted. “If you have patients with DNA repair deficiency, like BRCA2 [mutations], olaparib [Lynparza] could be used. But generally speaking, I go with docetaxel or radium-223. A novel hormonal therapy switch is just not preferred.”
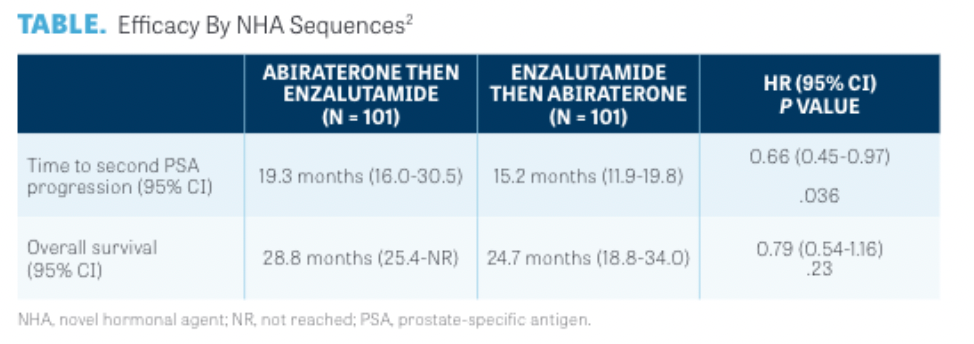
A multicenter, randomized, open-label, phase 2 trial (NCT02125357) conducted at 6 cancer centers throughout British Columbia, Canada, was designed to determine the optimal sequencing of enzalutamide and abiraterone in patients with mCRPC.2 Those enrolled to group A (n = 101) received abiraterone followed by enzalutamide, and those in group B (n = 101) received the reverse sequence.
Data indicated that at a median follow-up of 22.8 months, the time to second prostate-specific antigen (PSA) progression was longer in group A vs group B, at a median of 19.3 months (95% CI, 16.0-30.5) vs 15.2 months (95% CI, 11.9-19.8), respectively (HR, 0.66; 95% CI, 0.45-0.97; P = .036) (TABLE2). PSA responses to second-line treatment were observed in 36% and 4% of patients, respectively.
“With that being said and done, if you’re going to go with back-to-back hormone agents, in terms of sequencing, abiraterone followed by enzalutamide is most ideal,” Yu noted. “But back-to-back NHAs yield poor results.”
Timing for Radium-223: Before or After Chemotherapy?
The use of radium-223 comes with several considerations, Yu said. The agent can be administered to those with bone metastases and symptoms, but it cannot be given to those with visceral metastases. There are other stringent eligibility requirements for the agent regarding “hemoglobin, platelet count, and white blood cell count or ANC [absolute neutrophil count],” Yu added.
Previous treatment with docetaxel is known to increase the likelihood of challenges with neutropenia and/or thrombocytopenia. Radium-223 requires preauthorization whereas docetaxel does not. However, there is a higher likelihood of being able to administer all 6 doses of radium-223 in the prechemotherapy setting than in the postchemotherapy setting.
“For pragmatic reasons, I like the idea of trying to use radium-223 before chemotherapy if you can do it and the patient meets the criteria,” Yu noted.
“Precision therapy [should be used for these patients] when possible, not back-to-back NHAs because [they] yield poor results. If you have to do it, it’s better to go with abiraterone and then enzalutamide rather than [the reverse],” he said. “Radium-223 can be administered before docetaxel; there’s a survival benefit either before or after docetaxel, but the patient has to [meet the requirements]. However, if your patient has rapidly progressing disease, a PSA that is shooting up really fast, [and] you restage them and their disease is really exploding on the scans, docetaxel is your best shot at a response; it should be the most frequently relied upon pathway.”
Pathway for Patients With M0 CRPC Who Progress on Frontline NHAs
Considerations differ depending on how a patient enters into resistance to NHAs, Yu added. If a patient has M0 CRPC and receives an androgen receptor (AR) antagonist, the FDA-approved options are apalutamide (Erleada), enzalutamide, or darolutamide (Nubeqa).
“Although many of the options are the same, I think about things a little differently. Again, [I would go with] precision therapy when possible. The difference here is, I would never do back-to-back hormonal therapies. I’ll never go to abiraterone in this situation just because the response rates are abysmal after an AR-targeted therapy,” Yu explained.
Pathway for Patients With Metastatic Hormone-Sensitive Prostate Cancer (mHSPC) Following Frontline NHAs
For patients with metastatic hormone-sensitive prostate cancer (mHSPC) who received an NHA in the first-line setting, but not a triplet regimen, second-line treatment options are similar, according to Yu. Again, he will use precision therapy when possible. Radium-223 is preferable before docetaxel in eligible patients, and docetaxel should be the most relied upon pathway to increase chances of response. An NHA switch is more acceptable for these patients if they have started with abiraterone rather than apalutamide or enzalutamide. Those who received abiraterone can switch to another AR-targeted therapy.
“The reason to switch them is if you think about how patients progress, they have hormone-sensitive disease and now they are starting to progress to castration resistance. They are coming in every 3 to 4 months for their leuprorelin shots, for example, and you are checking their PSA [level],” Yu explained. “The vast majority of these patients are going to progress asymptomatically, and a lot of them do not want to move on to chemotherapy or intravenous therapies. As such, I do this switch a little bit more often from abiraterone to enzalutamide.”
Pathway for Patients With mHSPC Who Progress on Androgen Deprivation Therapy, Docetaxel With or Without NHAs
For patients with mHSPC who have high-volume de novo metastases and received androgen deprivation therapy (ADT) and either abiraterone or docetaxel, or ADT and darolutamide or docetaxel, the following options can be considered:
• Docetaxel retreatment if the patient had an outstanding response during the initial 6 cycles of treatment and their time to castration-resistant disease was over 2 years
• Cabazitaxel (Jevtana) for those without an outstanding response to docetaxel or who experienced many adverse effects previously
• Radium-223 for those with bone metastases, no visceral metastases, and symptoms
• 177Lutetium-PSMA-617
Combination Regimens of NHAs and PARP Inhibitors Show Early Promise
A combination of niraparib (Zejula) plus abiraterone acetate and prednisone (AAP) is under exploration as a frontline treat-ment for patients with mCRPC with and without homologous recombination repair (HRR) gene alterations, as part of the phase 3 biomarker-selected MAGNITUDE trial (NCT03748641).3
To participate, patients needed to have an ECOG performance status of 0 or 1 and a Brief Pain Inventory-Short Form worst pain score of up to 3. Patients were split into 2 cohorts: those who were positive for HRR gene alterations and those who were negative. Within those cohorts, patients were randomly assigned 1:1 to receive niraparib plus AAP or placebo plus AAP. Radiographic progression-free survival (rPFS) by central review served as the primary end point of the research.
In the subset of patients with BRCA1/2 mutations, the combination of niraparib and AAP resulted in a significant 47% reduction in the risk of progression or death. The median rPFS by central review in the investigative and control arms was 16.6 months vs 10.9 months, respectively (HR, 0.53; 95% CI, 0.36-0.79; P = .0014). In all patients positive for HRR, niraparib plus AAP reduced the risk of progression or death by 27%. The median rPFS by central review was 16.5 months in the investigative arm vs 13.7 months in the control arm (HR, 0.73; 95% CI, 0.56-0.96; P = .0217).
“That showed a PFS benefit for the bio-marker-selected population—not overall, and not for the negative population,” Yu noted.
In the phase 3 PROpel Study (NCT03732820), the combination of olaparib at 300 mg and abiraterone at 1000 mg (n = 399) was compared with placebo and abiraterone (n = 397) at the same dose as a frontline treatment for patients with mCRPC.4 Investigator-assessed rPFS served as the primary end point of the trial.
Data showed that the combination of olaparib and abiraterone significantly improved investigator-assessed rPFS over abiraterone alone, with a median of 24.8 months vs 16.6 months, respectively (HR, 0.66; 95% CI, 0.54-0.81; P < .0001). This translated to a 34% reduction in risk of disease progression or death and a median rPFS improvement of 8.2 months with the olaparib combination. The 12-month rPFS rates in the investigative and control arms were 71.8% and 63.4%, respectively; at 24 months, these rates were 51.4% and 33.6%, respectively.
“The subgroup analyses also look positive for both the biomarker-positive and -nega-tive populations, which is very interesting,” Yu noted.
Lastly, as part of the phase 3 TRITON3 trial (NCT02975934), investigators are examining the safety and effi cacy of rucaparib (Rubraca) monotherapy vs physician’s choice of docetaxel, abiraterone acetate, or enzalutamide in patients with mCRPC with mutations in BRCA or ATM.5
In a recently issued press release,5 it was reported that single-agent rucaparib significantly improved rPFS by independent radiology review compared with the physician’s choice of treatment. Notably, benefit was observed in both primary efficacy analyses of patients with chemotherapy-naïve metastatic disease, in those whose tumors harbored BRCA mutations as well as in the overall intention-to-treat (ITT) population.
In the BRCA-positive subgroup, the median rPFS in the rucaparib arm was 11.2 months vs 6.4 months in the control arm. In the ITT population, the median rPFS was 10.2 months with single-agent rucaparib vs 6.4 months with physician’s choice of treatment.
“That being said, we haven’t seen the breakdown of biomarker-positive vs -negative [patients],” Yu noted. “Growing data support these kinds of combinations of PARP inhibitors and abiraterone or enzalutamide, even potentially in the DNA repair–proficient population. Overall survival data are not mature yet, so we have to wait and see.”
REFERENCES
1. Yu E. Metastatic castration-resistant prostate cancer: combining and sequencing. Presented at: 2022 LUGPA Annual Meeting; November 10-12, 2022; Chicago, IL. Accessed November 11, 2022.
2. Khalaf DJ, Annala M, Taavitsainen S, et al. Optimal sequencing of enzalutamide and abiraterone acetate plus prednisone in metastatic castration-resistant prostate can-cer: a multicentre, randomised, open-label, phase 2, cross-over trial. Lancet Oncol. 2019;20(12):1730-1739. doi:10.1016/S1470-2045(19)30688-6
3. Chi KN, Rathkopf DE, Smith MR, et al. Phase 3 MAG-NITUDE study: first results of niraparib (NIRA) with abiraterone acetate and prednisone (AAP) as first-line therapy in patients (pts) with metastatic castration-resistant prostate cancer (mCRPC) with and without homologous recombination repair (HRR) gene alterations. J Clin Oncol. 2022;40(suppl 6):12. doi:10/1200/JCO.2022.40.6_suppl.012
4. Saad F, Armstrong AJ, Thiery-Vuillemin A, et al. PROpel: phase III trial of olaparib (ola) and abiraterone (abi) versus placebo (pbo) and abi as first-line (1L) therapy for patients (pts) with metastatic castration-resistant prostate cancer (mCRPC). J Clin Oncol. 2022;40(suppl 6):11. doi:10.1200/JCO.2022.40.6_suppl.011
5. TRITON3 phase 3 trial of Rubraca (rucaparib) achieves primary endpoint in men with metastatic castration-resis-tant prostate cancer with BRCA or ATM mutations. News release. Clovis Oncology, Inc. October 3, 2022. Accessed November 11, 2022. http://bit.ly/3hphW8z

Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More