Tarlatamab Shows Antitumor Activity, Safety in Small Cell Lung Cancer
The DeLLphi-300 trial of a bispecific T-cell engager showed favorable outcomes in patients with previously treated small cell lung cancer.
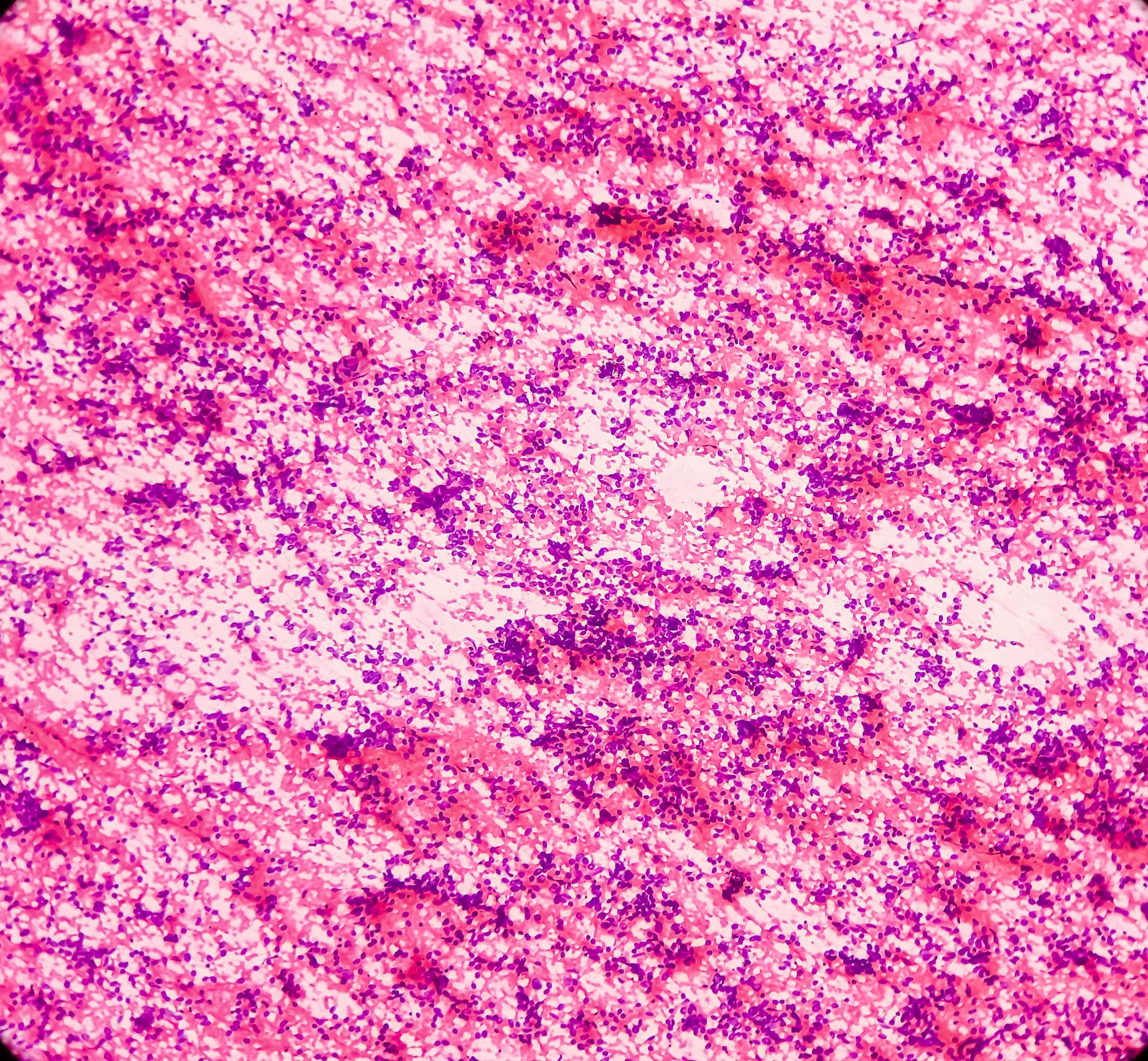
Image credit: © MdBabul via Adobe Stock
Tarlatamab, a bispecific T-cell engager, demonstrated manageable safety and response durability in the phase 1 DeLLphi-300 trial (NCT03319940) of patients with relapsed/refractory small cell lung cancer (SCLC).1
DeLLphi-300 investigators did not reach a maximum tolerated dose of tarlatamab. The objective response rate (ORR) was 23.4% (95% CI, 15.7-32.5), and exploratory analysis suggested that patients with increased DLL3 expression could have increased clinical benefit from this treatment. Cytokine release syndrome (CRS) was the most common adverse event, occurring in 52% of patients.
The half-life extended bispecific T-cell engager molecule tarlatamab binds both DLL3 and CD3, leading to T-cell–mediated tumor lysis. It is the first DLL3-targeted immune therapy to be evaluated clinically in patients with SCLC. Given the poor outcomes for patients with relapsed/refractory SCLC, there is a pressing need for new treatments in this setting, investigators stated in the report.
The first-in-human, multicenter, open-label phase 1 trial’s primary end point was safety and secondary end points included pharmacokinetics, pharmacodynamics, ORR per RECIST 1.1 criteria, duration of response (DOR), and progression-free survival and overall survival rates.
Patients were required to have cytologically or histologically confirmed relapsed/refractory SCLC following a platinum-based regimen and must have had ECOG performance score of 0 to 2. Patients with treated brain metastases were permitted to enroll if they met defined criteria.
Between December 26, 2017, and April 28, 2022, 107 total patients had been treated, 73 of which were treated in dose exploration cohorts ranging from 0.003 mg to 100 mg every 2 weeks intravenously. Starting from the 3-mg dose cohort, there was a day-1 run-in dose of 1 mg followed by the target dose on day 8, day 15, and every 2 weeks afterward. An additional 34 patients received the 100-mg dose in a dose expansion cohort. The patient population had a median of 2 prior lines of therapy (range, 1-6); anti–PD-1/PD-L1 therapy was previously received in 49.5% and prior radiotherapy in 79%. Thirty-six percent had brain metastases at baseline.
The median age was 63 years (range, 58-69). Former smokers made up 76% of the patients, with 13% being current smokers, 9% being never-smokers, and 2% missing data. The ECOG performance status was 0 in 37%, 1 in 62%, and 2 in 1%.
The confirmed ORR of 23.4% included 2 complete responses and 23 partial responses per investigator assessment. The disease control rate was 51.4% (95% CI, 41.5-61.2). Responses were observed with doses as low as 0.3 mg and higher rates of response were generally seen with doses of 3 mg and above. Tumor shrinkage of at least 30% in target lesions was observed in 39 patients (36.4%).
The median time to response was 1.8 months (range, 1.2-7.4) and the median DOR was 12.3 months (95% CI, 6.6-14.9). There were 11 patients who had an ongoing tumor response at the data cut-off of July 19, 2022. The median PFS was 3.7 months (95% CI, 2.1-5.4), and the median OS was 13.2 months (95% CI, 10.5–not estimable).
Retrospective DLL3 immunohistochemistry analysis found that 85 out of 90 evaluable patients expressed DLL3, with median tumor cell positivity of 95%. An exploratory analysis of 77 patients who received between 1 mg and 100 mg of tarlatamab suggested that increased DLL3 expression was correlated with greater clinical benefit.
Dose-limiting toxicities occurred in 6 patients, these being pneumonitis, CRS, encephalopathy, increased alanine aminotransferase, neutropenia, and pyrexia. Four patients discontinued treatment because of treatment-related adverse events (TRAEs): 2 of which were pneumonitis, 1 was encephalopathy, and 1 being immune effector-cell associated neurotoxicity syndrome (ICANS). One patient, aged 70, had a fatal case of pneumonitis at day 18 at a dose of 0.3 mg, but this was confounded by issues related to disease progression. There was 1 occurrence of grade 3 and 2 occurrences of grade 2 pneumonitis for 4.7 overall incidence rate.
Although 56 patients (52.3%) reported CRS, only 1 patient had CRS of grade 3. Tocilizumab (Actemra) was used to treat CRS in eight of 107 patients (7.5%). Other common treatment-emergent AEs included pyrexia in 43 patient (40.2%) and constipation in 33 patients (30.8%). Grade 3 or higher TEAEs occurred in 61 patients (57.0%) and serious AEs in 55 patients (51.4%). Nine patients (8.4%) required dose reduction, 4 of which were related to CRS. Twenty patients (18.7%) required dose interruption.
Neurologic events and neutropenia were considered to be of interest based on prior safety data on tarlatamab: there were 46 patients with grade 1 or 2, and 6 with grade 3, and 1 with grade 4 neurologic TRAEs. These included dysgeusia, headache, and dizziness. Grade 3 or higher neutropenia occurred in 11 patients (10.3%) and 10 patients (9.3%) received granulocyte colony-stimulating factor.
The mean terminal elimination half-life of tarlatamab in 101 evaluable patients was 5.7 days, which was consistent with the half-life extender platform’s aims in comparison to other bispecific T-cell engagers. An immunogenicitiy analysis showed that 10 out of 97 patients (10.3%) had developed anti-tarlatamab antibodies. Two patients had anti-tarlatamab antibodies at baseline; there was no apparent impact on exposure or safety.
Only 26.2% of patients went on to receive subsequent therapies after progression. The investigators noted limitations including the duration of follow-up of 8.7 months, the pooled efficacy measures of different dose levels, and the limited selection of patients eligible for a first-in-human trial. However, they noted that the strong median DOR and OS appeared favorable when considering outcomes in other clinical trials in relapsed/refractory SCLC, though direct comparisons between trials cannot be made.
The trial is still enrolling patients in the dose expansion cohort. Tarlatamab is also under investigation as monotherapy in SCLC and other neuroendocrine cancers in a phase 2 study (NCT05060016); in neuroendocrine prostate cancer in a phase 1b study (NCT04702737), and in in combination with carboplatin, etoposide, and PD-L1 inhibitor in a phase 1 study of previously untreated extensive-stage SCLC (NCT05361395).
Reference:
Paz-Ares L, Champiat S, Lai WV, et al. Tarlatamab, a First-in-class DLL3-targeted bispecific T-Cell engager, in recurrent small-cell lung cancer: An open-label, phase I study. J Clin Oncol. 2023;41(16):2893-2903. doi:10.1200/JCO.22.02823