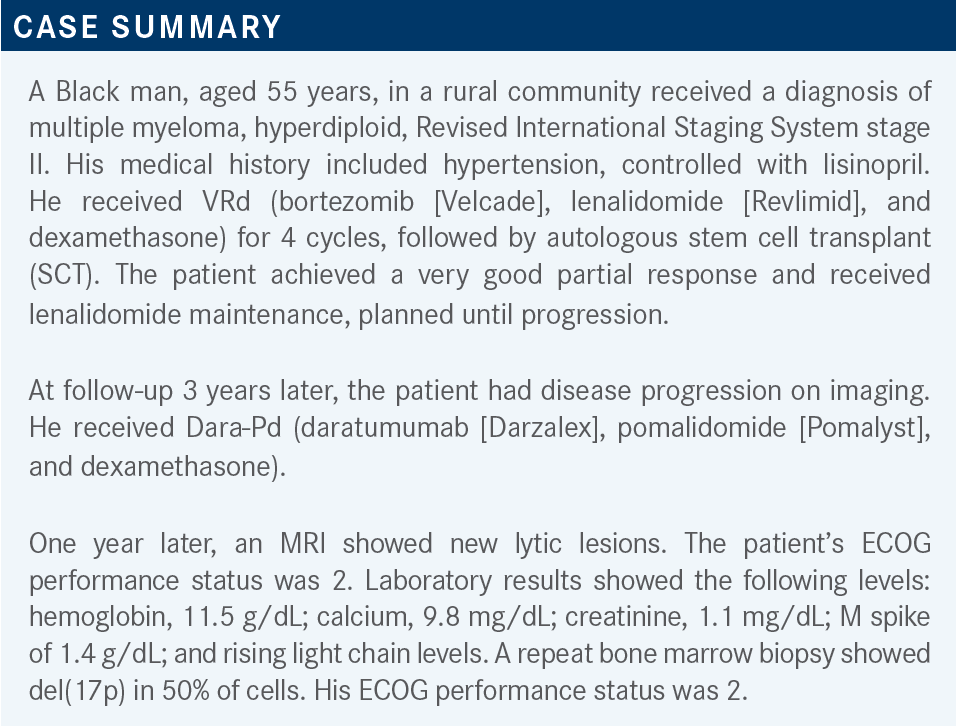
Roundtable Discussion: Zonder Reviews Choice of Therapy for R/R Multiple Myeloma
During a Targeted Oncology case-based roundtable event, Jeffrey Zonder, MD, discussed with participants the later-line therapy options for patients who have relapsed following several lines of treatment for multiple myeloma.
Jeffrey Zonder, MD (Moderator)
Hematologist, Barbara Ann Karmanos Cancer Institute
Clinical Professor, Hematology and Oncology
Wayne State University School of Medicine
Detroit, MI
DISCUSSION QUESTIONS
- What options would you recommend for this patient?
- What are the key factors influencing your decision-making for a patient like this?
- What are the challenges of treating a patient like this one?
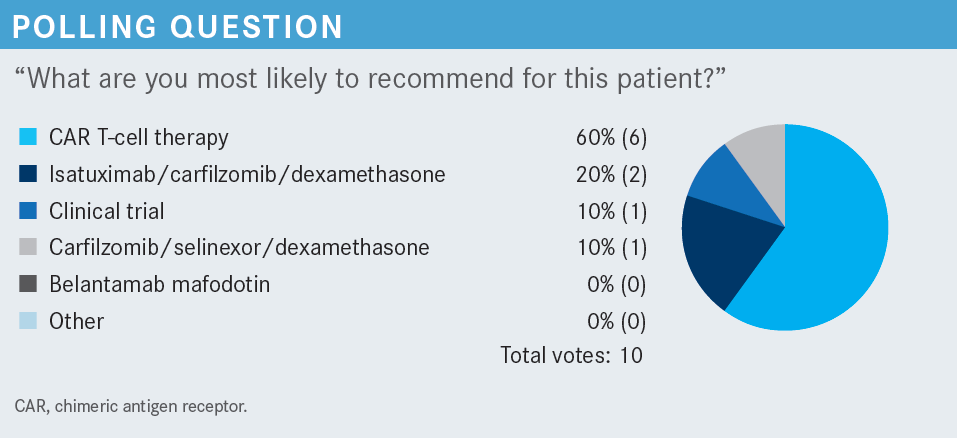
CHOWDHARY: I wanted to choose carfilzomib [Kyprolis] plus dexamethasone, but I chose carfilzomib, selinexor [Xpovio], and dexamethasone. I think chimeric antigen receptor [CAR] T-cell therapy is reasonable too, but usually you want them to be at least quad- [refractory] or penta-refractory before receiving the CAR T-cell therapy, and that is the reason I didn’t go toward it.1 But carfilzomib plus dexamethasone was not an option in the poll.
ZONDER: Was carfilzomib and dexamethasone the answer that anybody [else] wanted to give?
MATTOUR: Yes, I [would] pick it if it was an option. Not that CAR T-cell therapy is a bad option, but with this patient, the logistics of getting him to get the treatment safely is the issue.
ZONDER: There are some data related to carfilzomib and selinexor. It’s phase 2 data [from the STOMP trial; NCT02343042], and there is another randomized trial being conducted to parallel what we saw with the BOSTON trial [NCT03110562], which was low-dose selinexor with low-dose bortezomib [showing superiority to] the standard-dose bortezomib.2
SABAGH: For me [the key factor] was performance status. I looked at his age, 55 [years], which is young. He got an SCT. With recurrence, SCT was not reconsidered, and I was wondering why. So, now he has good performance status. I went for [CAR T-cell therapy], the 1 option that could be close to a second SCT.
ZONDER: “Other” was an option. I think [a second SCT] is a good other option that wasn’t chosen but it would have been very reasonable. This patient had 3 years before showing evidence of progression. A second SCT on the heels of some second-line induction therapy could have been an option here.
NARRA: I chose CAR T-cell therapy because I consider belantamab mafodotin [Blenrep] toxic.
ZONDER: It is interesting that two-thirds of participants picked BCMA [B-cell maturation antigen]–targeted therapy, but it was all CAR T-cell therapy and there was no belantamab. There is a perception among us about the strengths and weaknesses of each platform. Eye toxicity is a concern with belantamab.
NARRA: We have not had great success with selinexor, and [belantamab] has pitfalls. We didn’t have that much success in a couple of patients whom I tried isatuximab [Sarclisa] with, so CAR T-cell therapy was the choice.
ZONDER: There was a recent publication that showed that isatuximab therapy on the heels of prior daratumumab progression is not a particularly effective strategy.3 It is basically just another CD38-targeting antibody. So, use one or the other. One would think about isatuximab in the same context that you would think about [repeated] treatment with daratumumab. So, if you weren’t prepared to continue daratumumab in this patient, then an isatuximab-containing regimen probably wouldn’t work.
Did any other factors besides belantamab toxicity influence your decision? [Was] the toxicity of CAR T-cell therapy a discouragement?
MATTOUR: [Although] both are excellent options, I did not choose [either] of them because of the logistics of [monitoring] this patient who…lives in a rural area….The ideal patient would have easy access to monitoring and addressing toxicities for either [belantamab] or CAR T-cell therapy.
NARRA: The response rates [are a factor] too. With CAR T-cell therapy, you’d have [approximately] a 70% response rate, right?
ZONDER: With both approved CAR T-cell therapies, you have response rates upwards of 70%.4,5 That is correct. One [ciltacabtagene autoleucel; Carvykti] is a bit higher than that.5 Were the differences in response rates a major factor in the decision-making between [belantamab and CAR T-cell therapy]?
NARRA: Yes, definitely.
ZONDER: What about others who voted for CAR T-cell therapy?
FRONTIERA: I voted for CAR T-cell therapy [for] 2 reasons. One, the patient seems like he is declining quickly, and if he is ever going to get CAR T-cell therapy, this is the window that he might have, because it seems like his performance status declined a lot over a short period. Second, a lot of patients like the idea of CAR T-cell therapy as 1-and-done. If one gets through it, survives, and gets through the toxicities, then they are off treatment, at least for a while. Belantamab is a continuous therapy. Sometimes that’s harder.
ZONDER: Right. I think that’s a commonly cited reason.
MARINELLA: I agree…1-and-done is what I was thinking. The other thing is that from a practical standpoint, belantamab is not easy. They have to see an optometrist or an ophthalmologist whom you must educate, unless you are in a big tertiary center. It’s inconvenient. I have not used it for some of those reasons, and when I’ve offered it, it’s been a hard sell because it does take a lot of dedication for patients.
ZONDER: I’ve found, schedule-wise, if you think about the number of clinic visits, wherever those clinic visits are, it’s not very different [from] many of the regimens we use. It’s [fewer visits] than a bortezomib-based regimen with weekly therapy. But one of the difficulties we run into at our medical center [Barbara Ann Karmanos Cancer Center in Detroit, Michigan], where we have a lot of patients who have unreliable transportation, is that the consequences of missing the eye exam are not the same as those of missing a week of bortezomib. If one misses their eye exam, they’re stuck. They must delay the next dose until you find a way to get the patient to the eye exam. One needs that information to proceed. So, logistically, it is sometimes challenging because that eye exam is so important for this drug.
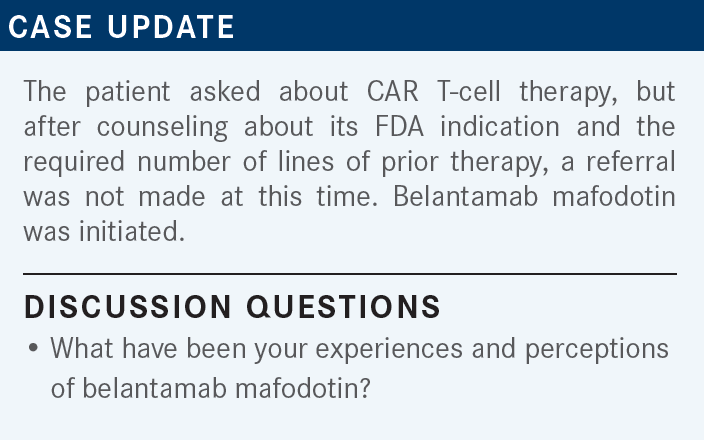
BALLOUZ: I prescribed it for a patient. It was a young man in his late 50s who had failed everything, and he was dispirited. So, I tried it. He probably got 2 doses, then he [died]. So, I did not see a response. But that was a last option for me.
ZONDER: So, this was a drug that you used when all else failed. He received 2 doses total, 3 weeks apart?
BALLOUZ: Yes.
FRONTIERA: I think the ocular toxicity and the requirements for ophthalmology evaluation for each dose have been an inhibitory experience, and we haven’t coordinated it well with our optometrists or ophthalmologists.
ZONDER: It does take work coordinating the evaluations and sending patients. We send our patients over the eye exam form they need to have filled out, and then have the ophthalmologist send it back to us. Occasionally the patients bring it back with them, but usually it is sent to us. But it takes coordination. Is that the main issue? Is it more a concern about the eye toxicity, or is it more about the inconvenience of monitoring the eye toxicity? Or is it a bit of both?
BALLOUZ: A little bit of both, but [more] the monitoring.
LANG: I almost used [belantamab]. Our practice offers CAR T-cell therapy, and I feel like we have the option readily available. Of course, it’s challenging because there is a waiting list, right now. I almost used [belantamab], but my transplant physician said no. He prefers the selinexor-based treatment.
MARINELLA: I only used selinexor once. I used it about 1 year ago with a regimen that was published in Blood.6 I think it was with bortezomib and dexamethasone. It was tough because of the nausea. I know there is a lot of preemptive [management] that you are supposed to do such as dose titration, hydration, and antiemetics, and I’m liberal with those. That has been my only experience. But it was in combination.
ZONDER: I can’t overemphasize how important the antiemetics are, at least on the day of [treatment], and the day after. We use a lot of ondansetron [Zofran], a lot of olanzapine [Zyprexa], and other things on hand at home, if necessary. We tell patients to extend the duration of those antiemetics if needed, because it is not easy. It is much easier to use as a once-weekly agent, so when I use it with bortezomib, or with carfilzomib, I do once weekly, and I will generally do a lower dose. I won’t use 80 mg twice weekly. I’ll use 60 mg or 80 mg once weekly, and that’s often much more tolerable. So, I am much more inclined to use it with other agents, especially if the patient is not refractory to any of the ones I just named.
What about GI [gastrointestinal] toxicity? I guess the things I’ve heard cited in the past as reasons not to use selinexor are the toxicity, mostly GI, and then [the lack of] efficacy. Which is the bigger issue from your standpoint: the efficacy, the toxicity, or both?
KNAPP: For me it has primarily been the toxicity. I also thought there were some issues with cytopenia. I’ve spoken with the drug representatives, as I did just last month; they basically are saying to not even think of using this as a twice-weekly drug. They are saying just use it once weekly.
ZONDER: [Twice weekly] is still on the label. But it is more toxic when you use it twice weekly than when you use it once weekly. So, for patients you are already a little bit worried about, who have a poor appetite, anorexia, and are already struggling heading into the therapy, even as monotherapy, I will sometimes start it once weekly just to make sure they can tolerate even that. But when used by itself, technically on label, it’s twice a week, and the dose reduction is to rapidly move to once weekly to mitigate toxicity.
ZONDER: It sounds like for both drugs, toxicity concerns were the main issue. Response rates were less commonly cited among the participants in this meeting. Just for comparison, selinexor plus dexamethasone has a response rate in the 20% to 25% range compared with the 30% to 35% response range seen with belantamab [From the Data7,8]. So, they have similar response rates, but different adverse effect [AE] profiles. We have the eye toxicity and some myelosuppression with belantamab, and we have the GI toxicity, myelosuppression, and sometimes hyponatremia with selinexor.
The goals of therapy for patients who have been heavily pretreated include getting a response. But I think what I am hearing everybody say is that quality of life is a major factor in the selection of therapy. Did I adequately summarize what participants have expressed in our discussions so far?
MATTOUR: I think there is no other way to describe it. At the same time, patients do not have many attractive options at these [later] lines of therapy. Everything is relative, and the toxicity must be individualized per person. My concern is getting the right patient with the right support so that we can produce results. Selinexor becomes more attractive because it appears the toxicity is on the other side of the coin.
ZONDER: When I think about these drugs, most participants have not prescribed either of them. For the patient population for whom these drugs are approved, by the time they are at this line of therapy, are they at tertiary centers? Are they on a clinical trial, typically? Or are you just selecting other agents? I am curious to know what happens in practice with these patients when they have had 4 or 5 lines of therapy.
MATTOUR: They should be on a clinical trial, ideally, [assuming that they are in] a location where they have easy access to a center that has a clinical trial, or they accept being on a trial, after accumulating toxicities. A lot of patients say, “Give me something that is approved; why should I go on a trial?”
FRONTIERA: The other option you didn’t bring up was hospice.
ZONDER: I agree with you. Hospice, at any point after somebody has relapsed multiple times, is certainly a consideration.
FRONTIERA: These patients are beaten up by that time. A lot of these patients are elderly, too. There are not a lot of patients who could tolerate the intensity of some of these fifth and sixth lines of therapies. Some go to the tertiary clinical trials or something else.
ZONDER: Some of the patients on both the DREAMM-2 trial [of belantamab; NCT03525678] and in some of the selinexor trials were older. So, I think there is a patient selection factor. Just as we do routinely with bortezomib with dexamethasone, and particularly with lenalidomide, I think there is perhaps a dose reduction strategy that might be employed to help make these drugs more feasible. I am not advocating any one strategy, necessarily, but I often will start with once-weekly selinexor-based therapy.
With belantamab, I have spoken with [many] colleagues around the country, and I think a lot of physicians, especially after the second dose, just spread out the interval between the doses a bit to reduce the chances of developing eye toxicity. That is off-label, so I am not saying that this is an International Myeloma Working Group recommendation or anything like that. But it might be a toxicity mitigation strategy that could make it more feasible in patients you feel are vulnerable to the particular AEs.
REFERENCES
1. NCCN. Clinical Practice Guidelines in Oncology. Multiple myeloma, version 1.2023. Accessed September 28, 2022. https://bit.ly/2T0mDYS
2. Grosicki S, Simonova M, Spicka I, et al. Once-per-week selinexor, bortezomib, and dexamethasone versus twice-per-week bortezomib and dexamethasone in patients with multiple myeloma (BOSTON): a randomised, open-label, phase 3 trial. Lancet. 2020;396(10262):1563-1573. doi:10.1016/S0140-6736(20)32292-3
3. Mikhael J, Belhadj-Merzoug K, Hulin C, et al. A phase 2 study of isatuximab monotherapy in patients with multiple myeloma who are refractory to daratumumab. Blood Cancer J. 2021;11(5):89. doi:10.1038/s41408-021-00478-4
4. Munshi NC, Anderson LD Jr, Shah N, et al. Idecabtagene vicleucel in relapsed and refractory multiple myeloma. N Engl J Med. 2021;384(8):705-716. doi:10.1056/NEJMoa2024850
5. Berdeja JG, Madduri D, Usmani SZ, et al. Ciltacabtagene autoleucel, a B-cell maturation antigen-directed chimeric antigen receptor T-cell therapy in patients with relapsed or refractory multiple myeloma (CARTITUDE-1): a phase 1b/2 open-label study. Lancet. 2021;398(10297):314-324. doi:10.1016/S0140-6736(21)00933-8
6. Bahlis NJ, Sutherland H, White D, et al. Selinexor plus low-dose bortezomib and dexamethasone for patients with relapsed or refractory multiple myeloma. Blood. 2018;132(24):2546-2554. doi:10.1182/blood-2018-06-858852
7. Lonial S, Lee HC, Badros A, et al. Longer term outcomes with single-agent belantamab mafodotin in patients with relapsed or refractory multiple myeloma: 13-month follow-up from the pivotal DREAMM-2 study. Cancer. 2021;127(22):4198-4212. doi:10.1002/cncr.33809
8. Chari A, Vogl DT, Gavriatopoulou M, et al. Oral selinexor-dexamethasone for triple-class refractory multiple myeloma. N Engl J Med. 2019;381(8):727-738. doi:10.1056/NEJMoa1903455