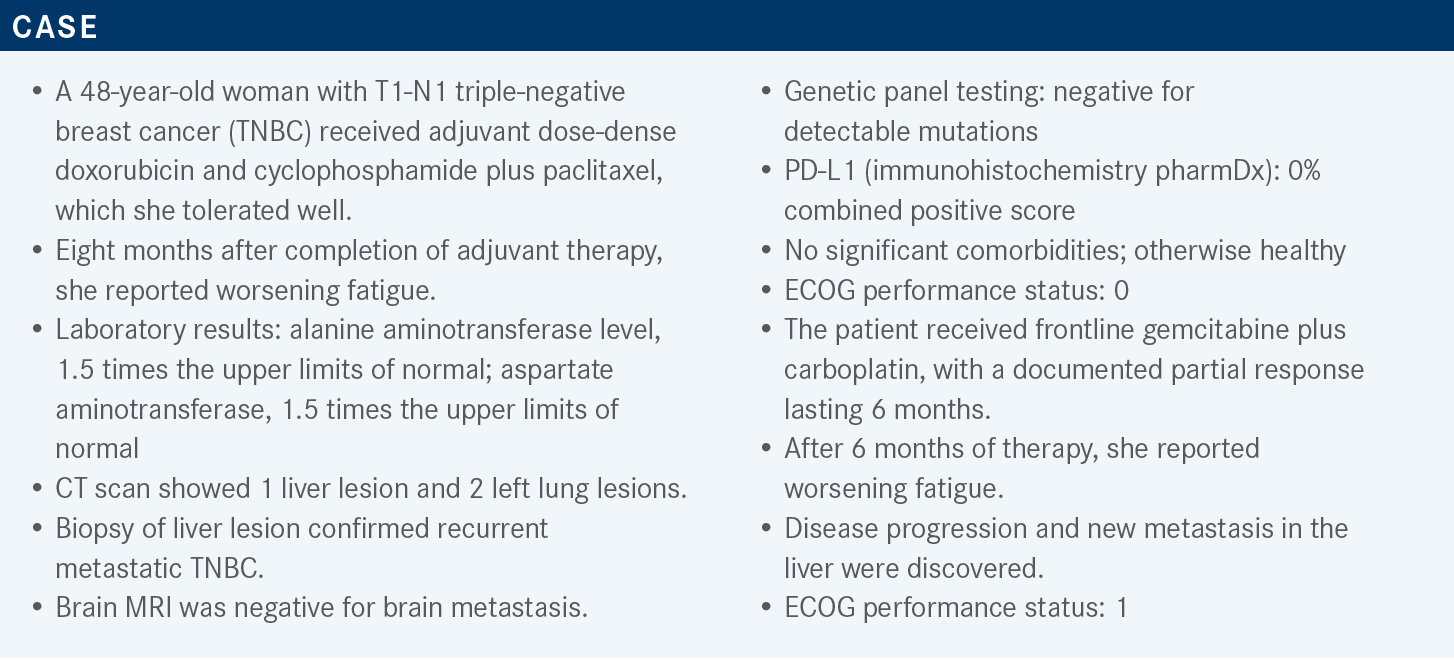
Jankowitz Discusses Use of Sacituzumab Govitecan in Metastatic TNBC
During a Targeted Oncology case-based roundtable event, Rachel C. Jankowitz, MD, discusses the result of treatment with sacituzumab govitecan in the ASCENT trial of patients with triple-negative breast cancer.
Rachel C. Jankowitz, MD
Director, Rena Rowan Breast Center
Associate Professor of Clinical Medicine
Perelman Center for Advanced Medicine
Abramson Cancer Center
Hospital of the University of Pennsylvania
Philadelphia, PA

Targeted OncologyTM: When is sacituzumab govitecan (Trodelvy) used in TNBC? Which data support this?
JANKOWITZ: Sacituzumab govitecan is incorporated into the [National Comprehensive Cancer Network] guidelines as an option for patients with metastatic TNBC who have received at least 2 prior therapies, with at least 1 of them being for metastatic disease.1
The study that led to its full FDA approval in April 2021 was the phase 3 ASCENT trial [NCT02574455], which was a randomized comparison of physician’s choice chemotherapy [with] sacituzumab govitecan for patients with previously treated metastatic TNBC.2 The patients included in the study had to have had 2 [or more] chemotherapies for advanced disease. One of the prior regimens could be for progression that occurred within a 12-month period after completion of their neoadjuvant or adjuvant therapy.3
What is the background for conducting the ASCENT trial?
It is compelling to keep in mind that the standard-of-care chemotherapy for TNBC is not very good, with response rates being [approximately] 10% and the median progression-free survival [PFS] approximately 2 months.
Clinically, there is a great unmet need for better therapies for this patient population. Sacituzumab govitecan is a novel Trop-2–directed antibody-drug conjugate [ADC], so it targets Trop-2, which is overexpressed in most TNBC. The antibody is conjugated via a hydrolysable linker, which means it breaks apart in solution to topoisomerase-I inhibitor [SN-38], an active metabolite of irinotecan [Camptosar].
Sacituzumab govitecan has 3 unique properties as an ADC: it’s highly specific in targeting Trop-2; it has a high drug-antibody ratio of 7.6:1; and the hydrolysis of the linker releases the SN-38 extracellularly, as well, in the tumor microenvironment. So, it has somewhat of a bystander effect, and it can affect cells that have low or no expression of Trop- 2 [because of] that bystander effect.
The phase 1 and 2 trials had shown activity for patients with metastatic TNBC with a response rate of [approximately] 33%, which led to an accelerated approval by the FDA. So, the ASCENT study was a confirmatory phase 3 trial.
How was this phase 3 study designed for patients with metastatic TNBC?
There were 529 patients randomly assigned 1:1 to sacituzumab govitecan or treatment of physician’s choice [TPC].3
The primary end point for the study was PFS in patients without brain metastasis. PFS for the entire patient population was a secondary end point, as was overall survival [OS]. The TPC choices were: eribulin [Halaven], which 54% of patients got; vinorelbine [Navelbine], which 20% of patients [got]; capecitabine [Xeloda], which 13% of patients got; and gemcitabine [Gemzar], which 12% of patients got.
The main patient group, which is termed the efficacy population, are patients in the study who did not have brain metastases, which was most patients. Only 61 patients had brain metastases and were not included in the primary end point PFS analysis.
The baseline characteristics of the efficacy population, made up of 468 patients, were well balanced. The median age was 54, [and approximately] 7% of patients in each arm had germline BRCA1 and BRCA2 mutations.
Interestingly, [approximately] one-third of patients in each arm did not have TNBC at initial diagnosis. In other words, their primary tumor was not triple negative. I know we’ve seen this come up a lot, where a patient had a different phenotype with their primary, but then their metastatic sample was triple negative. So, that was not a low number in this trial. The median time from diagnosis to metastatic disease was [approximately] 15 months, and it was well balanced in both arms.
The patients had visceral disease. Importantly, bone-only disease was not allowed [for] this trial, so they had to have disease elsewhere. [Approximately] 100% of them had prior taxanes, 82% had prior anthracyclines, and 66% had prior carboplatin at some point. Interestingly, 29% had prior immunotherapy with PD-1 or PD-L1 inhibitors.
What was the efficacy observed in the ASCENT trial?
The sacituzumab govitecan arm had a very statistically significant improvement in PFS of 5.6 months compared with only 1.7 months in the TPC arm [HR, 0.41; 95% CI, 0.32-0.52; P < .0001]. The trial was stopped early due to the efficacy via a unanimous recommendation of the Data and Safety Monitoring [Board].
The median OS nearly doubled in the sacituzumab govitecan arm at 12.1 months vs 6.7 months for TPC [HR, 0.48; 95% CI, 0.38-0.59; P < .0001], which was also statistically significant.3 The benefit of the drug compared with standard chemotherapy was seen across subtypes irrespective of age, race, previous therapies, and previous use of PD-1 or PD-L1 immunotherapy. Interestingly, it also was independent of whether they had an original diagnosis of triple-negative disease or an acquired TNBC later. The overall response rate [ORR] was 35% in the sacituzumab govitecan arm vs only 5% in the TPC arm. The efficacy analysis for the entire patient population included 61 patients who had brain metastases at baseline. The median PFS was 4.8 months in the sacituzumab govitecan arm vs 1.7 months in the TPC arm [HR, 0.43; 95% CI, 0.35-0.54; P < .001].
The common adverse events [AEs] with the drug were not unexpected based on the phase 1 and 2 studies. They included neutropenia, diarrhea, nausea, alopecia, fatigue, and anemia.
There was no greater than grade 3 neuropathy or [interstitial lung disease]. Just 1 patient developed grade 3 pneumonitis. Interestingly, 49% of patients were treated with concomitant growth factor support, so that was a high number. I think a lot of us have seen in practice that the neutropenia can be an issue. This was compared [with] only 23% of patients in the TPC arm being treated with growth factor. AEs leading to treatment discontinuation were infrequent in both groups at 5%.
Comparing the efficacy of sacituzumab govitecan with each of the individual TPC drugs on the ASCENT trial showed the efficacy benefit was retained regardless of which chemotherapy they were treated with.4 The ORR, again, was high with sacituzumab govitecan at 35% vs only 3% to 6% in all the comparator chemotherapy arms, so the outcomes were undoubtedly better. This was just a follow-up analysis after the initial trial data were presented.
Please discuss the biomarker analysis done on this trial.
A prespecified subgroup biomarker analysis was done to look at the question of whether the drug works for patients with BRCA germline mutations and regarding the degree of Trop-2 expression on the tumor. Most patients with TNBC will have Trop-2 expression, and 80% of patients in the ASCENT study had high or medium Trop-2 expression.
The survival outcomes and ORR were numerically higher in the sacituzumab govitecan arm compared with the TPC arm in patients with high or medium Trop-2 expression. The responses in those patients were analogous to what they were in the primary efficacy population.
Unfortunately, there was only a very small number of patients with low Trop-2 expression on the study, so they couldn’t derive definitive conclusions on whether the drug was beneficial in these patients, which is frustrating. It was not able to be identified as a negative predictive biomarker. The benefit of sacituzumab govitecan over TPC was similar regardless of germline BRCA1 or BRCA2 status, so it seemed to help either way. This was essentially a negative biomarker exploration because it didn’t identify a group that wouldn’t benefit.5 Good for the drug company, but good that it’s helping patients, too.
How did older patients do in ASCENT compared with younger patients?
In the outcomes by age, dose reductions were more frequent in patients older than 65 years compared with those younger than 65 years for both arms of the trial. The dose reductions were similar in both arms in all age groups and didn’t seem to impact efficacy.6
There was no treatment-related death in the study, and the rates of AEs were similar in patients older than 75 years, just as was observed in patients older than 65 years. This analysis basically concluded that even though patients were older, they still showed a survival benefit with sacituzumab govitecan over TPC, and they still seemed to have a relatively tolerable safety profile.6 So, we shouldn’t necessarily be afraid to use it in older patients.
In patients 65 years and older, the rates of febrile neutropenia were 8% in the sacituzumab govitecan arm vs 0% in the TPC arm. Diarrhea of all grades was 65% in the sacituzumab govitecan arm compared with 15% in the TPC arm, which is high, but only 10% of that was grade 3 or higher. There were high rates of GI [gastrointestinal] AEs in the sacituzumab govitecan arm, but there were not high rates of grade 3 and 4 GI AEs. Alopecia needs to be mentioned, as it was high at 37%.6 Sometimes we forget with the ADCs [that] it can still happen.
REFERENCES
1. NCCN. Clinical Practice Guidelines in Oncology. Breast cancer, version 4.2022. Accessed September 21, 2022. https://bit.ly/3kxcYWm
2. FDA grants regular approval to sacituzumab govitecan for triple-negative breast cancer. FDA. Updated April 08, 2021. Accessed September 21, 2022. https://bit. ly/3BAdDhi
3. Bardia A, Hurvitz SA, Tolaney SM, et al; ASCENT Clinical Trial Investigators. Sacituzumab govitecan in metastatic triple-negative breast cancer. N Engl J Med. 2021;384(16):1529-1541. doi:10.1056/NEJMoa2028485
4. O’Shaughnessy J, Punie K, Oliveira M, et al. Assessment of sacituzumab govitecan (SG) versus treatment of physician’s choice (TPC) cohort by agent in the phase 3 ASCENT study of patients (pts) with metastatic triple-negative breast cancer (mTNBC). J Clin Oncol. 2021;39(suppl 15):1077. doi:10.1200/JCO.2021.39.15_suppl.1077
5. Bardia A, Tolaney SM, Punie K, et al. Biomarker analyses in the phase III ASCENT study of sacituzumab govitecan versus chemotherapy in patients with metastatic triple-negative breast cancer. Ann Oncol. 2021;32(9):1148-1156. doi:10.1016/j. annonc.2021.06.002
6. Kalinsky K, Oliveira M, Traina TA, et al. Outcomes in patients (pts) aged ≥65 years in the phase 3 ASCENT study of sacituzumab govitecan (SG) in metastatic triple-negative breast cancer (mTNBC). J Clin Oncol. 2021;39(suppl 15):1011. doi:10.1200/ JCO.2021.39.15_suppl.1011