Polatuzumab Combination Can Be Applicable if CAR T Is Not an Option in DLBCL
Eleven months after completion of therapy with the R-CHOP regimen, a 43-year-old woman with diffuse large B-cell lymphoma complained of fever, night sweats, and back pain.
Loretta J. Nastoupil, MD

During a Targeted OncologyTM Case-Based Roundtable event, Loretta J. Nastoupil, MD, associate professor, director, Lymphoma Outcomes Database, and section chief, New Drug Development Department of Lymphoma and Myeloma, Division of Cancer Medicine at The University of Texas MD Anderson Cancer Center, discussed the case of a 43-year-old woman with diffuse large B-cell lymphoma.
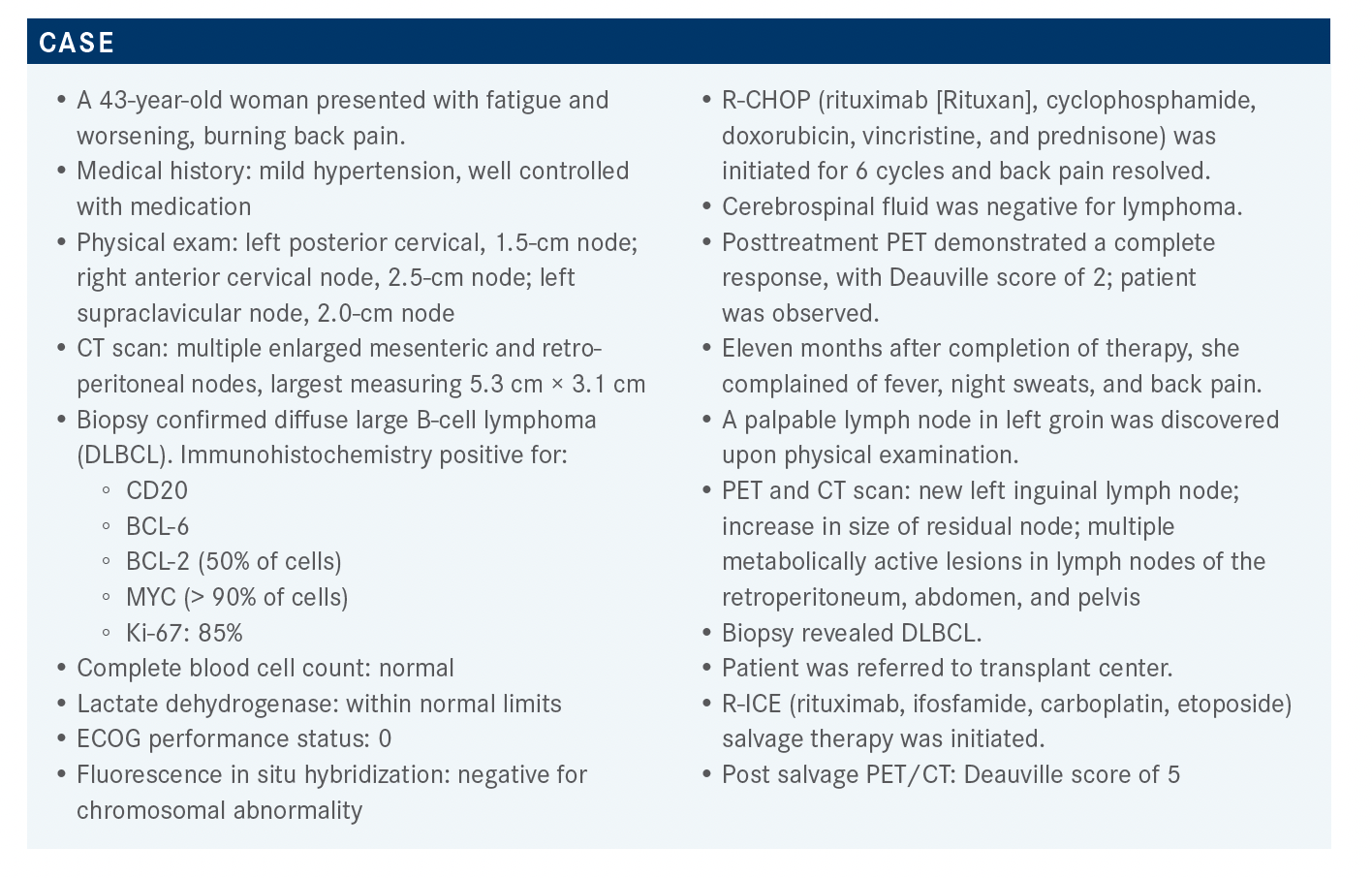
Targeted OncologyTM: What is the follow-up treatment for patients with DLBCL who relapse or are refractory to treatment?
NASTOUPIL: The National Comprehensive Cancer Network [NCCN] has guidelines on the follow-up treatment for patients who complete frontline or subsequent lines of therapy. They’re generally monitored every 3 to 6 months for 5 years and annually thereafter.1
Imaging [should be considered no more than] every 6 months for 2 years after completion of therapy and then only as clinically indicated. This is based off EFS [event-free survival] data from Mayo Clinic, which suggest that at least 90% of patients with [DLBCL] experience a relapse within the first 2 years following frontline therapy. Retrospective data suggest that a relapse can be detected in 99% of patients with DLBCL, based off the physical exam and history, hence the preemptive surveillance scans may be unnecessary.
If they relapse on second- or later-line treatment, options are listed in the NCCN guidelines. Three randomized trials looked at CAR [chimeric antigen receptor] T-cell therapy vs salvage therapy. We’ve had the top-line results from 2 of the 3 reported thus far, but they are positive studies suggesting that CAR T-cell therapy.
will be a potential second-line option for patients who were transplant-eligible and relapsed within 12 months of R [rituximab (Rituxan)]-chemotherapy. There are alternative second-line options for patients in whom allogeneic hematopoietic cell transplant [HCT] is deemed inappropriate. Best supportive care can be considered given the historically poor outcomes of patients with relapsed or refractory DLBCL.
For patients who have had R-CHOP as frontline therapy, some common second- or later-line regimens are R-ICE, R-DHAP [dexamethasone, cytarabine, cisplatin], R-GDP [gemcitabine, dexamethasone, cisplatin], R-GemOx [gemcitabine, oxaliplatin], and bendamustine [Treanda] plus rituximab plus polatuzumab vedotin [Polivy], a CD-79b antibody-drug conjugate now available. More recent agents include loncastuximab tesirine [Zynlonta], which is a CD19 antibody-drug conjugate, and tafasitamab [Monjuvi] plus lenalidomide [Revlimid]. Tafasitamab is a naked CD19 antibody. We also have selinexor [Xpovio], which is an oral nuclear export inhibitor. The role for third- or later-line R-chemotherapy is dwindling, given their poor outcomes prior to novel agents on the treatment landscape.
In the absence of details from the second-line studies, CAR T-cell therapy is currently approved for patients who have failed 2 prior systemic lines of therapy. These are patients either with primary refractory disease who are also refractory to salvage chemotherapy or who proceeded to high-dose therapy or allogeneic HCT and relapsed. Most patients are currently getting CAR T-cell therapy in the fourth- or later-line space, as opposed to the third-line space, but uptake in general has been quite low, with only about 18% of eligible patients in the United States getting it. I suspect that these patients are often sick and frail, and the time it takes to get to a referral or a treating center likely affects the decision to pursue this therapy.
What studies support the use of CAR T-cell therapy in patients with relapsed or refractory DLBCL?
The pivotal phase 2 studies that led to the FDA approval of 3 autologous anti-CD19 CAR T-cell immunotherapy in the third- or later-line space required patients to have had at least 2 prior lines of therapy that included a CD20 and an anthracycline. However, they were different in terms of the conduct of the trials and the patient population, so they shouldn’t be compared head-to-head. The ZUMA-1 study [NCT02348216], for example, took patients that were refractory and had failed to achieve chemotherapy-sensitive disease after frontline or second-line therapy or had progressed within 12 months of an autologous stem cell transplant [ASCT].2 The JULIET study [NCT02445248] and the TRANSCEND study [NCT02631044] allowed patients who had relapsed. There was a higher percentage of patients in the JULIET study who had failed a prior ASCT, suggesting that a larger portion of patients at some point had chemotherapy-sensitive disease.3 The TRANSCEND study was the most generous in terms of baseline characteristics and patients with a creatinine clearance as low as 31 mL/min, ECOG performance status as high as 2, and a left ventricular ejection fraction as low as 41% qualified. Apart from patients with primary mediastinal DLBCL, they also included patients with transformed DLBCL, de novo DLBCL, transformation from other inlet histology, such as Richter’s, and a history of central nervous system disease.4
Again, there were very significant differences in terms of the baseline characteristics across these studies and also differences in the turnaround time in terms of manufacturing from leukapheresis to successful cell infusion, and it’s impossible to compare the outcomes of these studies.
The toxicity profiles, however, can be fairly compared, though again they used different grading systems. The JULIET study for tisagenlecleucel [Kymriah] used a University of Pennsylvania grading system for cytokine release syndrome [CRS] different from the Lee criteria used in the other 2 studies.3 Later, they tried to adjust the CRS rates for the JULIET study and found they were lower. In my clinical experience, axicabtagene ciloleucel [axi-cel; Yescarta] is the most reliable in terms of manufacturing, with very high success rates of manufacturing and a median turnaround time of 16 to 17 days, including outside of the prospective study in the real world, but it’s also the most toxic. I think at least one-third of patients with axi-cel will have grade 3 or higher neurotoxicity, and at least 10% to 12% will have grade 3 or higher CRS.2
That’s important when you’re trying to determine who is an appropriate candidate is for CAR T-cell therapy. Lisocabtagene maraleucel [liso-cel; Breyanzi] can be given in outpatients with very low rates of grade 3 or higher CRS and neurotoxicity, which is generally reversible. It has a longer manufacturing time of about 24 days and slightly higher rates of manufacturing failure, though most of it is just off-spec products. We have an expanded access protocol available to enroll patients on.4
The current NCCN guidelines on CAR T-cell therapy show that they are indicated for patients who’ve had at least 2 or more prior lines of therapy. Most patients will have had 3 prior lines of therapy. It requires referral to a therapy center, perhaps because of a center’s ability to manage acute CRS or neurotoxicity but also for logistics purposes—having a cell processing lab that can perform leukapheresis, process, ship, and receive cells, then administer the product and manage the acute toxicity.1
I do share a lot of patients with community practices where I’m happy to keep patients who had leukapheresis for the first 30 days post cell infusion and then I often return patients back where they can be monitored for cytopenia, potential infection, and surveillance for lymphoma.
These pivotal phase 2 studies were tightly controlled trials likely with a huge amount of selection bias, and in the ZUMA-1 study, a small number of just 12 centers, but it did get up to many sites eventually. The JULIET study, in contrast, had about 200 participating sites, so it was very different in size. We tried to administer the commercial product across some centers that didn’t actually participate in the study and see what the practice patterns were.
What will you recommend for this patient now that CAR T-cell therapy is not an option?
Based on the NCCN guidelines, options include third-line chemotherapy [gemcitabine plus oxaliplatin] plus a CD20 antibody [rituximab]. Other options are polatuzumab vedotin [Polivy] plus bendamustine [Bendeka] plus rituximab [pola-BR], tafasitamab plus lenalidomide, loncastuximab, or selinexor.1
There are ongoing debates as to whether having prior exposure to CD19 in a patient being considered for CAR T-cell therapy at a later line would affect CD19 expression. Looking at the data, it’s challenging to answer that. In all the CAR T-cell therapy studies, CD19 expression was not associated with the outcomes. Even patients that had 0 or very low CD19 expression responded to the autologous CARs. The argument here is that the measuring of CD19 expression is inadequate. CD19 is ubiquitous in B cells and if they have never been targeted before, there’s no reason for patients to have antigen loss. There were some data on ALL [acute lymphocytic leukemia] that showed patients who had prior blinatumomab [Blincyto] and then went on to receive tisagenlecleucel had inferior outcomes.
That was what raised the question as to what the impact would be of having a prior suboptimal response to CD19-directed therapy on subsequent CD19-directed therapies. There have been reports, particularly in ALL, of antigen escape or antigen loss. DLBCL is an infrequent driver of resistance to CAR T-cell therapy, but now that we do have therapies like loncastuximab and tafasitamab plus lenalidomide, questions are being raised, like “Is it smart to introduce those treatments if you’re headed to CAR T-cell therapy later?” I think that’s a fruitless argument because if patients respond to the frontline therapy, you’re not worried about subsequent lines of therapy. Give the best or most appropriate treatment and then deal with the consequences later. Some minimal data suggest that patients who fail tafasitamab plus lenalidomide still maintain CD19 expression, and patients who have had prior loncastuximab have responded to CAR T-cell therapy and vice versa.
Does allogeneic HCT still have a role?
It probably does, particularly in young, fit patients who can respond to a subsequent line of therapy. The challenge is if we have therapy that could get patients into a stable response to give the graft time to perform and also have a patient who is a good candidate with an appropriate donor.
The data for allogeneic HCT have been limited, but likely some patients have durable responses to it, particularly in ALL. It has been pursued particularly in the post–CAR T-cell therapy period for patients who have had a partial response or even a complete response. In DLBCL, it has been reserved for patients who fail CAR T-cell or other therapies but may have a transient response.
Have you used pola-BR in your treatment of patients with DLBCL?
Polatuzumab targets CD79b, which is a great target, particularly for B-cell lymphomas because it’s part of the B-cell receptor complex. We don’t have any other therapies targeting it thus far. It’s an antibody-drug conjugate with the chemotherapy moiety MMAE [monomethyl auristatin E] like brentuximab vedotin used in Hodgkin lymphoma. It is a targeted delivery of chemotherapy to CD179b cells.5
The approval for polatuzumab was based off GO29365 [NCT02257567], a randomized phase 2 study of pola-BR in patients who had either follicular lymphoma [FL] or DLBCL and had at least 2 prior lines of therapy.6
Why did they use bendamustine as a backbone for polatuzumab in DLBCL?
This is partly because all these patients had 2 prior lines of therapy, so because of the MMAE component, peripheral neuropathy is one of the dose-limiting adverse events [AEs]. It’s challenging to combine polatuzumab, particularly with gemcitabine, which is a more common third-or later-line therapy in DLBCL. Also, there was activity with polatuzumab either as a single agent or in combination with rituximab, but it wasn’t durable or patients progressed too quickly during the initial phase 1 studies with DLBCL so that they felt the need for chemotherapy to slow the proliferation of the disease, and bendamustine could potentially achieve that. The study was comparing BR vs pola-BR in the 2 different cohorts of FL and DLBCL. Each cohort had 80 patients. The polatuzumab dose was 1.8 mg/kg on day 1, bendamustine was 90 mg/m2 on days 1 and 2, and standard dose rituximab [at 375 mg/m2] was used.6
The median age of the patients was 67 for the pola-BR group and 71 for the BR group. The duration of response [DOR] of their last treatment and whether they were refractory to last treatment were almost equal across the 2 groups. There was a slightly higher percentage of patients who had a prior SCT in the pola-BR than in the BR group and a slightly higher germinal center subgroup in the BR-only arm.6
The median DOR was 40% in the pola-BR group vs only 17.5% for the BR-only group. About 20% in both groups had a progression event and the overall response rate [ORR] was 45% for the pola-BR group. Prior to this study, any therapy that resulted in an ORR of 30% or higher was considered a potentially successful strategy.6 The median progression-free survival [PFS] was 9.5 months for pola-BR vs 3.7 months for BR [HR, 0.36; 95% CI, 0.21-0.63; P < .001]. The overall survival [OS] was 12.4 months for pola-BR vs 4.7 months for BR.6 Historically, prior to CAR T-cell therapy, the median OS for patients on third- or later-line therapy with DLBCL was 6 months or less, which is outlined by the 4.7 months in the BR arm.
So, this is a significant improvement in OS for patients who got pola-BR. For the AE profile of pola-BR vs BR, we don’t see substantial additive toxicity. The grade 3 febrile neutropenia, for instance, was about 10% with pola-BR vs 12.8% with BR only. Similarly, we don’t see higher rates of GI toxicity and fatigue. Peripheral neuropathy is the only AE that is significantly higher with pola-BR, but it’s mostly grade 1 or 2 at 44% vs 7% for BR alone.6 Cytopenias were common, which is not surprising, given the bendamustine. Because peripheral neuropathy is associated with polatuzumab, patients got only 6 cycles. I have given polatuzumab and rituximab only in patients I am trying to get to CAR T-cell therapy because of the theoretical and potentially real concerns that bendamustine is harmful to T cells, but I have not had much success.
Where do you see polatuzumab vedotin and CAR T-cell therapy fitting into the DLBCL treatment landscape?
We’ve got R-CHOP in the front line, and the POLARIX frontline study [NCT03274492] is looking at replacing vincristine with polatuzumab. We do not have the results of that study yet, and enthusiasm wanes the longer it takes to hear the results. We are looking into using polatuzumab in the patients who’ve failed CAR T-cell therapy. There is potentially some advantage to having chemotherapy when you’ve failed an immunotherapy approach. The only problem in that setting I’ve experienced is the cytopenia. About 20% to maybe 40% of post–CAR T-cell therapy patients will have persistent cytopenia. It is particularly challenging if they progress quickly.
REFERENCES:
1. NCCN. Clinical Practice Guidelines in Oncology. B-cell lymphomas, version 4.2021. Accessed September 17, 2021. https://bit.ly/3geoS5N
2. Neelapu SS, Locke FL, Bartlett NL, Miklos DB, Jacobson CA, Braunschweig I, et al. Axicabtagene ciloleucel CAR T-cell therapy in refractory large B-Cell lymphoma. N Engl J Med. 2017;377(26):2531-2544. doi:10.1056/NEJMoa1707447
3. Schuster SJ, Bishop MR, Tam CS, Waller EK, Borchmann P, McGuirk JP, et al. Tisagenlecleucel in adult relapsed or refractory diffuse large B-Cell lymphoma. N Engl J Med. 2019;380(1):45-56. doi:10.1056/NEJMoa1804980
4. Abramson JS, Palomba ML, Gordon LI, Lunning MA, Wang M, Arnason J, et al. Lisocabtagene maraleucel for patients with relapsed or refractory large B-cell lymphomas (TRANSCEND NHL 001): a multicentre seamless design study. Lancet. 2020;396(10254):839-852. doi:10.1016/S0140-6736(20)31366-0
5. Sawalha Y, Maddocks K. Profile of polatuzumab vedotin in the treatment of patients with relapsed/refractory non-Hodgkin lymphoma: a brief report on the emerging clinical data. Onco Targets Ther. 2020;13:5123-5133. doi:10.2147/OTT.S219449
6. Sehn LH, Herrera AF, Flowers CR, Kamdar MK, McMillan A, Hertzberg M, et al. Polatuzumab vedotin in relapsed or refractory diffuse large B-cell lymphoma. J Clin Oncol. 2020;38(2):155-165. doi:10.1200/JCO.19.00172
Gasparetto Explains Rationale for Quadruplet Front Line in Transplant-Ineligible Myeloma
February 22nd 2025In a Community Case Forum in partnership with the North Carolina Oncology Association, Cristina Gasparetto, MD, discussed the CEPHEUS, IMROZ, and BENEFIT trials of treatment for transplant-ineligible newly diagnosed multiple myeloma.
Read More