Personalized Acuity Tool Improves Resource Utilization
An acuity tool developed at the Mitchell Cancer Institute (MCI) at the University of South Alabama offers a comprehensive portrait of a patient’s condition that assists oncology nurse navigators in allocating their time and resources efficiently. It also provides managers with a way to determine caseload size in order to provide better patient care. The Association of Community Cancer Centers (ACCC) recognized the value of the analytical instrument at its recent conference with a 2017 Innovator Award.
Currently available tools use a limited number of factors to measure acuity, making it difficult to distinguish between patients who need very few resources versus those who need more attention. In contrast, the Oncology Navigation Acuity Tool incorporates 12 factors to measure the level of care required by each patient, said Reverend Diane Baldwin, RN, OCN, CBCN, the creator of the tool (TABLE1).
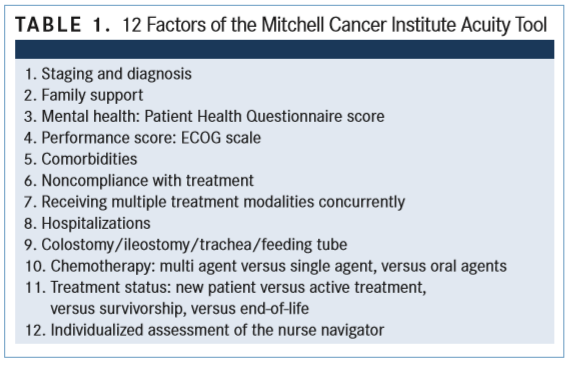
By using more factors to determine a patient’s acuity score, the MCI tool provides an accurate picture of an individual patient’s status. “Some of the factors include staging and diagnosis, depression score, performance score, comorbidities, family support, number of treatment modalities the patient is undergoing, and recent hospitalizations,” said Baldwin,
manager of quality assurance at MCI, which is located in Mobile, Alabama.
Baldwin, who also is a United Methodist minister, commented on her experience using the tool during the ACCC’s 34th National Oncology Conference, held October 18-20 in Nashville, Tennessee. During her presentation, Baldwin emphasized the importance of the tool’s 12th factor, which takes into account the nurse navigator’s personal experience with the patient and the unique relationship between nurse and patient. “Patients are more than a score,” she said. “There are times when the patient’s scores add up to a certain acuity number, but there [is additional information] that the nurse navigator knows about the patient that will affect that score.
“Acuity scores are important to guide us and help determine how we are using our limited resources,” Baldwin continued.
She described the case of a patient who had an acuity score of 0. However, the patient was suffering from depression because of the recent death of a spouse, on whom the patient had depended during her cancer journey. The oncologist advised the patient to “come back in 6 months,” but the nurse navigator determined that the patient needed referrals for grief counseling, a support group for widows, and increased phone contact.
Baldwin used the acuity tool for 247 patients over 6 months. In the acuity tool analysis, Baldwin determined the average number of each of these workload measures: monthly patients on caseload (144), monthly in-person visits (97), monthly phone calls (56), monthly referrals (13), clinical interventions (30), and stat interventions (4). Stat interventions are those that prevent the patient from going to the emergency department or being admitted to the hospital. She analyzed the caseload mix by acuity levels for the percentage of visits, the impact on phone calls, referrals, and stat interventions (TABLE 2).
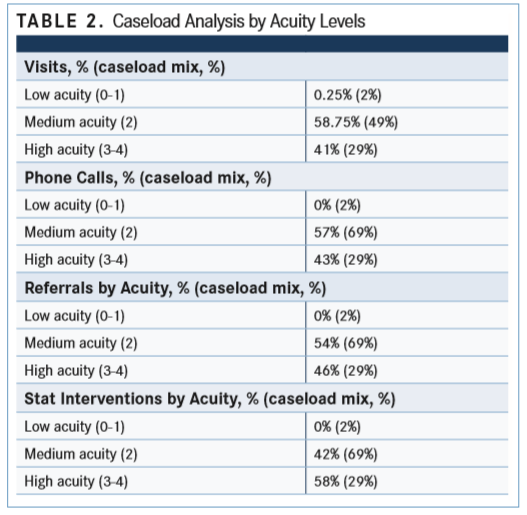
When comparing caseload mix with visits by acuity levels, she found that 29% of patients were considered high acuity and that these patients made up 41% of visits. “These high-acuity patients are using the most resources,” she said. When she looked at caseload mix versus stat interventions, she found 29% of the caseload was high acuity and 58% of these patients required stat interventions.
Baldwin says training in the use of the 1-page acuity tool is minimal and easy, as is its implementation. It can be customized to individual institutions and has accurately identified which patients need more services and resources.
“Using the tool, I know exactly how much my nurse navigators can take on, based on acuity and not so much on sheer numbers,” she said. “It has given us a clear picture of where we expect our utilization, referrals, time, and interventions to come from. This helps us plan our navigation team much better than before implementing the tool.

Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More