Narsoplimab Exceeds Expectations Across High-Risk HSCT-TMA Subtype
Administered narsoplimab in patients with high-risk hematopoietic stem cell transplant– associated thrombotic microangiopathy resulted in a response rate of 61% among all patients treated with the monoclonal antibody
Alessandro Rambaldi, MD

Administered narsoplimab (OMS721) in patients with high-risk hematopoietic stem cell transplant– associated thrombotic microangiopathy (HSCT-TMA) resulted in a response rate of 61% among all patients treated with the monoclonal antibody (n=28; 95% CI, 40.6%-78.5%; P<.0001), according to results from a phase 2 trial (NCT02222545). In patients treated per protocol with at least 4 doses of narsoplimab (n=23), the response rate was 74% (n=17; 95% CI, 51.6%-89.8%; P<.0001).
The MASP-2 inhibitor demonstrated high response rates and a significant improvement in laboratory markers and organ function irrespective of subgroup in adult patients, according to findings presented during the 47th Annual Meeting of The European Society for Blood and Marrow Transplantation, which was held virtually in March.1
“Based on external advisory feedback, the estimated response rate for this patient population was 15%, and this was indeed the FDA-agreed efficacy threshold for the primary end point in this clinical trial,” said lead study author Alessandro Rambaldi, MD, a professor in the Department of Oncology and Hematology-Oncology at the University of Milan and head of the hematology and bone marrow transplant unit at ASST Papa Giovanni XXIII in Bergamo, Italy, during his presentation of the data.
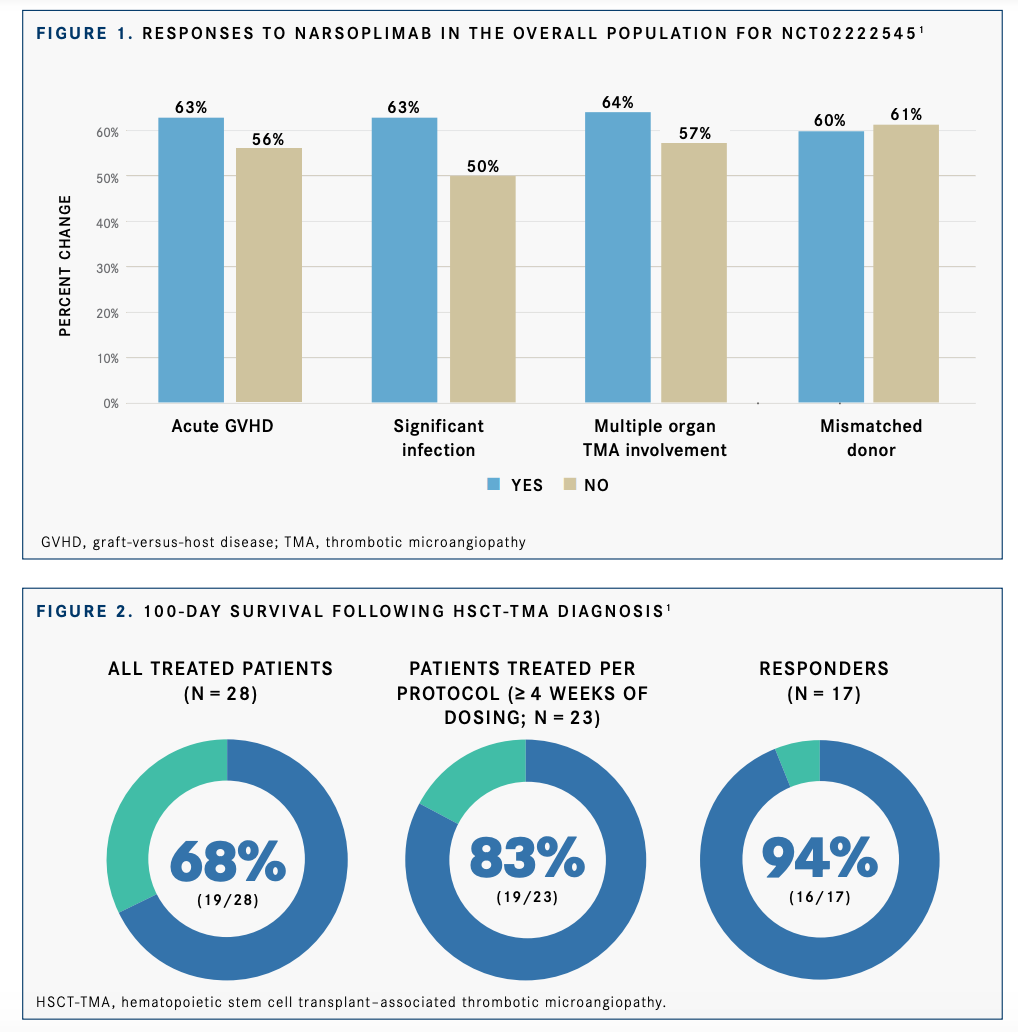
Moreover, responses were observed with narsoplimab in the overall population irrespective of subgroup, including age (<65, 58%; ≥65, 75%), sex (male, 65%; female, 50%), acute graft-versus-host disease (GVHD, 63%; no GVHD, 56%), significant infection (yes, 63%; no, 50%), multiple organ TMA involvement (yes, 64%; no, 57%), mismatched donor (yes, 60%; no, 61%), and transfusion within 2 weeks prior to first narsoplimab dose (yes, 56%, no, 100%) (FIGURE 11).
Additionally, patients responded regardless of baseline platelet count (≤20 × 109 /L, 60%;>20 × 109 /L, 61%), kidney dysfunction (yes, 57%; no, 71%), pulmonary dysfunction (yes, 40%; no, 65%), neurological dysfunction (yes, 63%; no, 58%), or gastrointestinal dysfunction (yes, 100%; no, 59%).
Endothelial injury syndromes such as HSCT-TMA, GVHD, veno-occlusive disease/sinusoidal obstruction syndrome, capillary leak syndrome, idiopathic pneumonia syndrome, and diffuse alveolar hemorrhage are common pathways for many early transplant complications caused by conditioning regimens, immunosuppressive agents, infections, and alloreactivity.
“TMA is a serious and life-threatening syndrome that is underrecognized and can occur in up to 40% of patients undergoing stem cell transplantation. TMA may coexist with other endothelial injury syndromes, such as GVHD, thus leading to an increase in morbidity and mortality after transplantation,” Rambaldi said.
Narsoplimab is an investigational, fully human immunoglobulin (Ig) G4 monoclonal antibody that inhibits MASP-2, an effector enzyme of the lectin pathway of complement. In HSCT-TMA, narsoplimab blocks the lectin pathway activation that results from endothelial injury. The agent also blocks MASP-2– mediated coagulation and activation of kallikrein. In turn, narsoplimab leaves the effector function of the adaptative immune response intact to fight infection.
On January 19, 2021, the FDA granted a priority review designation to a biologics license application for narsoplimab for the treatment of patients with HSCT-TMA.2 The FDA is expected to make a decision regarding the approval of narsoplimab by July 17, 2021, and does not plan to hold an advisory committee meeting to discuss the application.
The single-arm, open-label study was initiated as a phase 2 trial; however, after the FDA granted a breakthrough therapy designation to narsoplimab for patients with HSCT-TMA, the study was converted into a pivotal trial, Rambaldi explained.
The study protocol specified that patients receive 4 mg/kg or 370 mg of intravenous narsoplimab once weekly for at least 4 weeks.
Eligible patients had to be 18 years or older and have persistent HSCT-TMA defined as a platelet count less than 150,000/µL; evidence of microangiopathic hemolysis, such as the presence of schistocytes; serum lactate dehydrogenase (LDH) bove the upper limit of normal or haptoglobin below the lower limit of normal; and renal dysfunction for at least 2 weeks following modification or discontinuation of calcineurin inhibitors.
Patients with coexisting conditions, including GVHD, recent controlled infection, refractory underlying disease or relapse, and multiple organ dysfunction, were eligible for enrollment.
Patients who received eculizumab (Soliris) within 3 months prior to screening or had a positive direct Coombs test or serious uncontrolled infections at entry were excluded.
The coprimary end points of the study were response-based efficacy and safety and tolerability. Efficacy was defined as an improvement in TMA laboratory markers of platelet count and LDH and improvement in clinical status, which comprised any predefined criteria in blood, renal, pulmonary, gastrointestinal, or neurological markers. Secondary end points included 100-day survival, overall survival (OS), and change from baseline in laboratory markers.
The median age of patients was 48, and most patients were male (n = 20; 71.4%). The majority of patients had malignant underlying disease (n = 27; 96.4%)
Risk factors for poor outcomes included the presence of GVHD (n=19; 67.9%), significant infection (n=24; 85.7%), pulmonary dysfunction (n=5; 17.9%), neurological dysfunction (n=16; 57.1%), multiple organ involvement (n=14; 50.0%), and renal dysfunction (n=21; 75.0%). Moreover, 93% of patients had multiple risk factors for poor outcomes.
Additional data showed a 68% (n=19) 100-day survival rate following HSCT-TMA diagnosis among all patients treated with narsoplimab. In patients treated per protocol, the 100-day survival rate was 83% (n=19). Finally, among responders (n=17), the 100-day survival rate was 94% (n=16) (FIGURE 21 ).
The median OS for the overall patient population was 274 days (95% CI, 103-not estimable [NE]). In the per-protocol population, the median OS was 361 days (95% CI, 176-NE). In the responder population, the median OS was NE (95% CI, 273-NE).
Regarding safety, 96.4% (n=27) of patients in the overall population reported any adverse effect (AE). The most common AEs observed in at least 15% of patients treated with narsoplimab included pyrexia (n=10; 35.7%), diarrhea (n=9; 32.1%), vomiting (n=9; 32.1%), nausea (n=7; 25.0%), neutropenia (n=7; 25.0%), fatigue (n=6; 21.4%), hypokalemia (n=6; 21.4%), and back pain (n=5; 17.9%).
“The patient population had a high expectant death rate,” Rambaldi said. “In such [an ill] population with so many comorbidities, narsoplimab was well tolerated.”
Of note, 6 patients died during the core study period because of events commonly reported with HSCT, such as neutropenic sepsis, septic shock, progressive acute myeloid leukemia, TMA, and GVHD.
Narsoplimab is also under investigation in several phase 3 trials that are evaluating the agent’s use in other lectin pathway– associated diseases and endothelial injury syndromes, including IgA nephropathy (NCT03608033) and atypical hemolytic uremic syndrome (NCT03205995).
References:
1. Rambaldi A, Claes K, Goh YT, et al. Narsoplimab (OMS721), a MASP-2 inhibitor, for the treatment of adult hematopoietic stem cell transplant-associated thrombotic microangiopathy (HSCT-TMA): subgroup analyses. Abstract presented at: 47th Annual Meeting of the EBMT; March 14-17, 2021; virtual. Abstract OS4-2.
2. Biologics license application for narsoplimab in HSCT-TMA accepted for priority review by U.S. FDA. News release. Omeros Corporation. January 19, 2021. Accessed March 16, 2021. http://bit.ly/2NncWTb

Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More
















