Meeting Cochair Honors Immunotherapy Era in Lung Cancer
Julie R. Brahmer, MD, MSc, FASCO, cochair of the upcoming 19th Annual Winter Lung Cancer Conference, has seen the full development of immunotherapy era in lung cancer from the beginning.
Julie R. Brahmer, MD, MSc

Over the past decade, the impact of immunotherapy in the lung cancer space has only grown from early signals of the potential efficacy of immune checkpoint inhibitors in solid tumors.
Julie R. Brahmer, MD, MSc, FASCO, cochair of the upcoming 19th Annual Winter Lung Cancer Conference, has seen the full development of immunotherapy era in lung cancer from the beginning. Brahmer, director of the Thoracic Oncology Program at Kimmel Cancer Center at Johns Hopkins Bayview and professor of oncology at the Johns Hopkins Kimmel Cancer Center in Baltimore, Maryland, was on the ground floor 10 years ago as phase 1 studies of nivolumab (formerly MDX 1106; Opdivo) showed signals for antitumor activity and tolerability in patients with advanced solid tumors,1 and continued into phase 3 trials.
In an interview with Targeted Therapies in Oncology™, Brahmer said she has been a principal investigator in many phase 1 trials in her career in oncology drug development. However, this phase 1 study of nivolumab was one of the more exciting trials to see the results of and it was a goal of her career achieved to see the study extend into later phase studies and on to FDA approval.
She said that before this study, non–small cell lung cancer (NSCLC) had been considered potentially non-immunogenic, which was disproved with the immune checkpoint inhibitor studies, and treatment options for patients with NSCLC were minimal.
“It’s certainly exciting and gratifying to know that…I was a small part of the development of something that could have an effect on patients who otherwise had really minimal treatment options,” Brahmer commented.
Since then, immunotherapy options have boomed across various stages of lung cancers.
Most recently, atezolizumab (Tecentriq) was FDA approved as an adjuvant therapy for patients with stage II to IIIA NSCLC whose tumors have PD-L1 expression on at least 1% of tumor cells and following resection and platinum-based chemotherapy.2
This approval was based on results from the phase 3 IMpower010 trial (NCT02486718), which showed an improvement in disease-free survival (DFS) with atezolizumab compared with best available therapy in patients with early-stage resected PD-L1–positive NSCLC (median DFS, not reached vs 35.3 months, respectively; HR, 0.66; 95% CI, 0.50-0.88; P = .004).
“It’s great to be able to see immunotherapy impact patients in early-stage disease for non– small cell lung cancer,” Brahmer said. “I think we’re just seeing the power of immunotherapy that…the immune system does play a role in disease control. And hopefully, at least early on, we’re seeing increased chances of cure, or at least disease-free survival, in that early-stage disease as well.”
The role of neoadjuvant/adjuvant immunotherapy in NSCLC will be discussed in a presentation on Saturday, February 5, 2022 (see AGENDA), with a key focus on safety, as well as in a special keynote presentation from Everett E. Vokes, MD, the prior night.
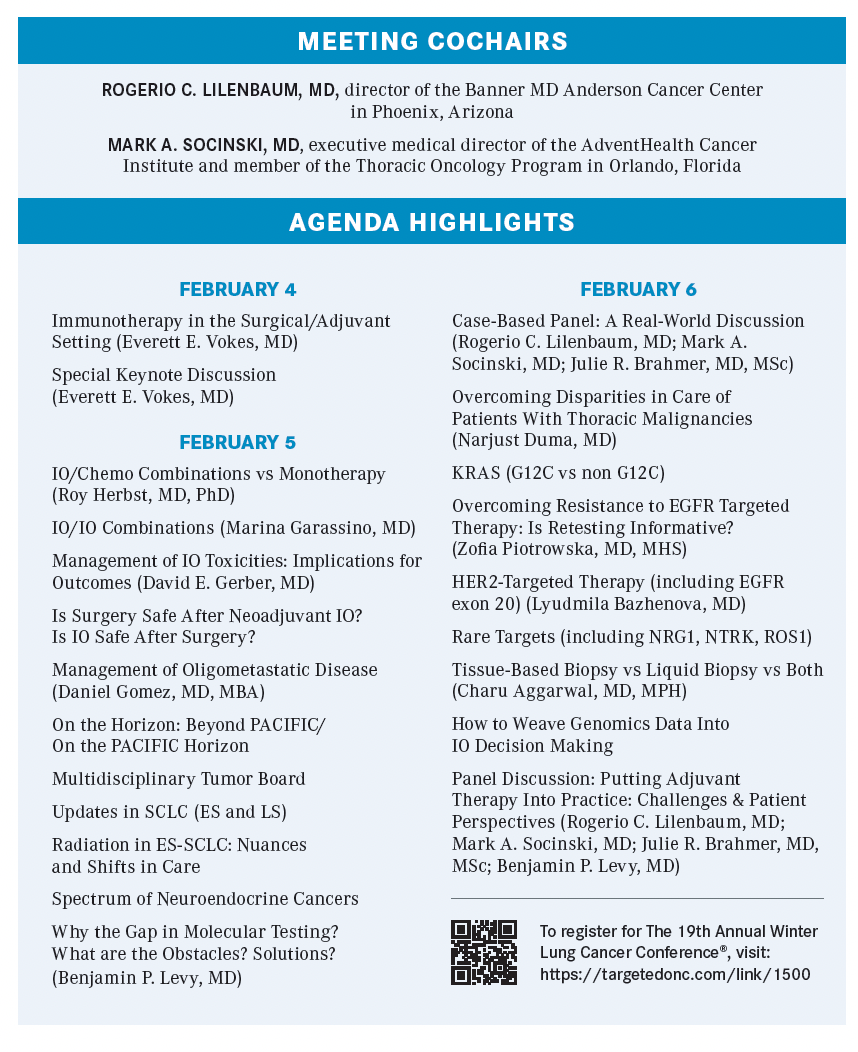
“It’s a multidisciplinary conference, so we will hear from surgeons, radiation oncologists, as well as medical oncologists about how immunotherapy plays a role in the treatment of lung cancer,” Brahmer said. “For the most part, oncologists are now getting comfortable treating patients with these inhibitors, but certainly, the toxicities [from immunotherapies], while typical for immune responses…there’s always nuances to these toxicities.”
Brahmer, who is a lead author of many guidelines providing recommendations for the management of immune-related adverse events, including most recently the updated guidelines from the Society for Immunotherapy of Cancer,3 stresses the importance of such guidelines as a basis for how to try to mitigate some of the varied immune-related toxicities seen with immune checkpoint inhibitors.
She explained that the meeting will focus on complex cases that are occasionally seen in the clinic “to give the providers who will be in attendance a framework in thinking about these toxicities.”
Targeted Therapy
Not to be outshone, the final day of the meeting will focus on advances in genomic testing as well as targeted therapies for NSCLC, including targets KRAS, EGFR, HER2, NRG1, and more.
“I’m excited to be able to offer [physicians and health care professionals dedicated] time in order to discuss some of these new treatment options and try to figure out how best to integrate them into our practice,” Brahmer said.
For example, while previously patients with EGFR exon 20 insertion mutations did not benefit from the standard EGFR inhibitors, patients now have 2 newly FDA-approved options specifi cally targeting EGFR exon 20 insertion mutations: amivantamab (Rybrevant) and mobocertinib (Exkivity).
Amivantamab was granted an accelerated approval on May 24 for patients with locally advanced or metastatic disease that has progressed on or after platinum-based chemotherapy.4 The approval was based on findings from a phase 1 trial (CHRYSALIS; NCT02609776) that showed that amivantamab monotherapy led to a response rate in 40% of patients with EGFR exon 20 insertion–mutant NSCLC and 74% had clinical benefit. The median progression-free survival was 8.3 months and the median overall survival was 22.8 months.5
Mobocertinib was granted accelerated approval on September 15 for a similar indication.6 In the phase 1/2 Study 101 trial (NCT02716116), the response rate was 28% in patients with EGFR exon 20 insertion–mutant NSCLC treated with mobocertinib and the median duration of response was 17.5 months.
On February 6, Lyudmila Bazhenova, MD, will provide an update on these and other HER2-targeted therapies in NSCLC.
REFERENCES:
1. Brahmer JR, Drake CG, Wollner I, et al. Phase I study of single-agent anti-programmed death-1 (MDX-1106) in refractory solid tumors: safety, clinical activity, pharmacodynamics, and immunologic correlates. J Clin Oncol. 2010;28(19):3167-3175. doi:10.1200/JCO.2009.26.7609
2. FDA approves atezolizumab as adjuvant treatment for non-small cell lung cancer. FDA. October 15, 2021. Accessed November 15, 2021. htt ps://bit.ly/3HuM5f9
3. Brahmer JR, Abu-Sbeih H, Ascierto PA, et al. Society for Immunotherapy of Cancer (SITC) clinical practice guideline on immune checkpoint inhibitor-related adverse events. J Immunother Cancer. 2021;9(6):e002435. doi:10.1136/jitc-2021-002435
4. FDA approves fi rst targeted therapy for subset of non-small cell lung cancer. FDA. May 21, 2021. Accessed November 17, 2021. htt ps://bit.ly/3fCjEyT
5. Sabari JK, Shu CA, Park K, et al. Amivantamab in post-platinum EGFR Exon 20 insertion mutant non–small cell lung cancer. Presented at: IASLC 2020 World Conference on Lung Cancer Singapore. January 28-31, 2021. Abstract OA04.04
6. FDA grants accelerated approval to mobocertinib for metastatic non-small cell lung cancer with EGFR exon 20 insertion mutations. FDA. September 16, 2021. Accessed November 17, 2021. https://bit.ly/3nnopkR
