Immunotherapy Offers Hopeful Outcomes in Nonmelanoma Skin Cancers
New and emerging treatment modalities for advanced nonmelanoma skin cancer provide hope for this patient subset.
The gold standard for localized nonmelanoma skin cancer (NMSC) treatment in the vast majority of patients is surgery and radiation therapy (RT), but treatment of advanced or metastatic NMSC may require systemic methods given the poor prognosis.1 New and emerging treatment modalities for advanced NMSC provide hope for this patient subset.
“I think the biggest thing that’s happened in the field and one of the reasons I’m enthusiastic about it is that there have been tremendous changes… very recently for both cutaneous squamous cell carcinoma and basal cell carcinoma,” said Michael K. Wong, MD, PhD, FRCPC, a professor in the Department of Melanoma Medical Oncology at The University of Texas MD Anderson Cancer Center, during an interview with Targeted Therapies in Oncology™.
Cutaneous Squamous Cell Carcinoma
Although cemiplimab (Libtayo) and pembrolizumab (Keytruda) have received FDA approval for use in cutaneous squamous cell carcinoma (CSCC), realworld data on tolerability and effi cacy are scarce, which has led to investigatory studies.2
The real-world clinical outcome and tolerability of cemiplimab-rwlc was evaluated in a retrospective cohort trial in the Netherlands.3 Objective clinical response was achieved in 50% of patients, with 13.6% having a complete response (CR; n = 66). The median progression-free survival (PFS) and overall survival (OS) rates were not reached after a median follow-up of 11.7 months. The most common adverse events (AEs) were fatigue and pruritis in 48.5% and 30.3% of patients, respectively. Real-world analysis of cemiplimab use demonstrated similar response rates to those of clinical trials and the drug was tolerable for patients with CSCC.3
Another trial that evaluated the real-world pattern of treatment in CSCC was performed in the United States using retrospective, observational data captured from health care claims from commercial health coverage or private Medicare supplemental coverage.4 Results demonstrated that between 2013 and 2019, 75.8% of patients received chemotherapy, 51.7% of patients received RT, and 35.7% of patients received targeted therapy as fi rstline treatment (n = 207). Cetuximab was the most common targeted therapy in the fi rst-line setting. However, the investigators concluded that results may not be refl ective of emerging real-world treatment patterns in the most recent years. They performed an analysis of the mortality using the National Death Index in 126 patients and found an OS of 76% at 6 months and 50% at 12 months post index date. Median survival without surgery or RT 180 days post index date was 11.2 months. Additionally, health care–related expenditures were mainly attributed to outpatient costs.4
Checkpoint inhibitors have been at the forefront of systemic therapy in advanced CSCC with the FDA approval of cemiplimab and pembrolizumab (Keytruda) in this patient population.
Wong said, “The 2 approved agents, cemiplimab and pembrolizumab, have propelled the field forward by showing significant objective response rate [ORR (achieved in approximately half of patients)] and a CR [rate around the 10% to 15% range. The results are] something very unusual considering that all we had before in the systemic space was combination cytotoxic chemotherapy or anti-EGFR drugs that are given as monotherapy or in combination with RT.”

The FDA’s granting an expanded label indication for pembrolizumab for the treatment of advanced CSCC was based on data from KEYNOTE-629 (NCT03284424), a multicenter, multicohort, nonrandomized, open-label trial. The ORR was 50% (n = 54). The AE profile was similar in CSCC compared with other malignancies.5 Cemiplimab and pembrolizumab have been incorporated into the standard of care as firstline treatment for advanced CSCC; however, the question of therapy sequencing remains unanswered. A study evaluated the sequential use of cemiplimab following progression on immunotherapy.6 Eleven patients were in cohort A, consisting of patients who received cemiplimab after immunotherapy, and 2 patients were in cohort B, consisting of those who received cemiplimab not immediately following immunotherapy. The ORR was 54% in cohort A and the cumulative 6-month disease control rate (DCR) was 77%. In cohort B, both patients had progressive disease (PD) as best response. Common AEs with cemiplimab included rash and hypomagnesemia. Investigators noted a high and durable response rate in cohort A, which requires validation in a larger patient population.6
On the sequencing of immunotherapy, Wong said, “The idea of sequencing with all current strategies [is an] extremely important question. There’s no answer to that yet. Certainly we’re learning from other cancers that are using immunotherapy, notably melanoma. All those questions that we’ve asked in melanoma, we’re now asking in squamous cell carcinoma and basal cell carcinoma as well.” Another potential emerging treatment option for patients with CSCC is nivolumab (Opdivo) in the first-line setting.7 A single arm phase 2 trial in treatment-naïve patients with advanced CSCC demonstrated an ORR at 24 weeks of 58.3% (n = 24). The median PFS was 12.7 months and estimated OS was 20.7 months. RT prior to nivolumab was associated with worse outcomes (P = .035). Overall, AEs were tolerable, and those related to nivolumab occurred in 87.3% of patients with the majority being grade 1 or 2. The investigators concluded that the findings from this trial further affirm checkpoint inhibitors as the standard of care in advanced CSCC.7
Basal Cell Carcinoma
Historically, patients with basal cell carcinoma (BCC) have had limited treatment options. “We’ve really had to resort to the toolbox that we had which was surgery, radiation. Perhaps the first breakthrough we had was in basal cell carcinoma where there was this recognition of a molecular pathway called a hedgehog pathway....” Wong said. “We recognize that there was a large proportion of these basal cell cancers which had aberrations in the hedgehog pathway resulting in the turning on of this pathway as a prerequisite for the cancer. By definition, inhibition of the same pathway would result in tumor regression…. For almost a decade now we’ve had the use of hedgehog inhibitors (HHIs) for basal cell carcinoma with more than half of the patients [responding to therapy], and if you add disease control rate, it’s even higher,” he continued.
A retrospective cohort study evaluated the characteristics and outcomes of patients who discontinued first-line treatment of HHIs in advanced BCC.8 A total of 73 patients discontinued first-line treatment with HHIs; 4 patients were included in the second-line initiators group and 15 were in the second-line noninitiators group. Fourteen patients discontinued fi rst-line HHI therapy because of toxicity and those patients were in the second-line noninitiators group. An additional 4 patients discontinued first-line HHIs because of disease progression and were in the second-line initiators group. One patient who discontinued first-line HHIs because of disease progression was in the second-line noninitiators group. The median time at which HHIs were discontinued was 9 months in the second-line initiators group and 7 months in the second-line noninitiators group. The time to fi rst-line HHI discontinuation was consistent with that of previous studies. The investigators found an unmet need for effective second-line treatment for patients after first-line HHI discontinuation in advanced BCC.8
Clinical trials have attempted to bridge the unmet gap of standard of care for second-line treatment of advanced BCC. In the past year, the FDA granted regular approval for cemiplimab for patients with locally advanced or metastatic BCC after treatment with HHIs or those who are unable to receive an HHI based on results from Study 1620 (NCT03132636), an open-label, multicenter, nonrandomized trial. In patients with locally advanced BCC, the ORR was 29% (n = 84). Additionally, in metastatic BCC, the ORR was 21% (n = 28).9
Wong said, “Now we have a new possibility in the use of anti–PD-1 immunotherapies, specifi cally cemiplimab. What has happened at ESMO [European Society for Medical Oncology] and ASCO [American Society of Clinical Oncology] are a slew of [results from] studies showing response rates in specifi c subsets or patients in community practice all in line with what we know is happening, which is [that cemiplimab] is an active therapy and gives us opportunities in the [HHI]-refractory space, which is something that we’ve not had before. Cemiplimab has filled an [unmet gap] in a significant way because one of the things is that patients achieve complete responses… and that’s a big deal.”
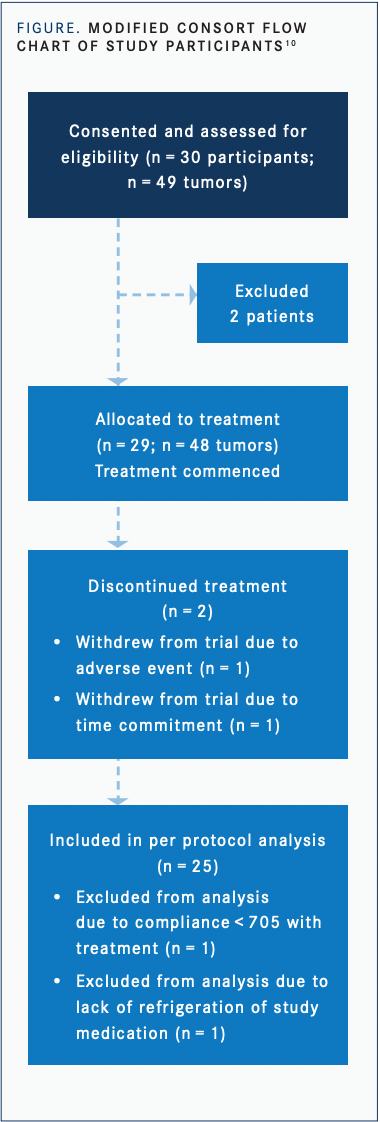
In addition to systemic targeted therapies in BCC, topical therapy with remetinostat, a histone deacetylase (HDAC) inhibitor, has also shown efficacy and safety for local treatment of BCC as an alternative to surgery.10 In the study, 27 patients with 45 tumors were included in the intentionto-treat analysis (FIGURE10).
According to Wong, “There’s been a tremendous amount of effort using immunomodulatory agents [in different drug delivery methods and]…we have tried to address this unmet gap in our therapeutic armamentarium. The use of topical HDAC inhibitors is along the same vein, but we don’t have good data yet to establish these as standards of care. Nevertheless, these are attempts to elucidate an immune response in an organ that has suffered prolonged and excessive UV radiation damage.”
Merkel Cell Carcinoma
One of the newer therapies approved for Merkel cell carcinoma (MCC), a rare and aggressive subset of skin cancer, is avelumab (Bavencio), an anti–PD-L1 immune checkpoint inhibitor. Results from the JAVELIN Merkel 200 trial (NCT02155647) led to the FDA approval of avelumab in MCC.11
Sandra D’Angelo, MD, a medical oncologist at Memorial Sloan Kettering Cancer Center, said, “The JAVELIN Merkel 200 study was conducted in 2 parts. The first part was a second-line postchemotherapy clinical trial [in which] a number of patients with MCC received avelumab at the time of progression on chemotherapy. [The results] formed the initial basis that led to the FDA approval of avelumab for MCC. In addition, the second part of the study was in a treatment-naïve cohort [who received] avelumab.”
Long-term data were presented at ASCO regarding patients who received at least 1 line of therapy prior to avelumab.11 The results demonstrated clinically meaningful OS of 12.6 months after 65.1 months of median follow-up in 88 patients. The OS rate at 48 months was 30% and at 60 months was 26%. The treatment discontinuation rate was 12.5%, with the most common reason for discontinuation being disease progression followed by AEs. Most patients, 71.6%, had died at the time of data cutoff, none as a result of avelumab-related AEs. Long-term results from this study solidify avelumab as the standard of care in patients with metastatic MCC after progression on at least 1 line of chemotherapy.11
“The 5-year follow-up data are the longest follow-up with checkpoint inhibitors we have in MCC. Overall, [this small population represented] meaningful and important data, which established checkpoint inhibitors as the standard of care in MCC,” noted D’Angelo.
Checkpoint inhibitors have found success in the treatment of metastatic MCC, but the question of their durability after therapy cessation was evaluated in a multicenter, international retrospective study in 40 patients.12 Avelumab was the primary checkpoint inhibitor in 90% of patients. The trial investigators found that patients had a median time on treatment of 13.5 months and median time on treatment after best response of 8 months. At the time of treatment discontinuation, a CR was achieved in 75% of patients, a partial response (PR) in 20%, and stable disease (SD) in 5%. However, after 12 months of follow-up after therapy discontinuation, 35% of patients had PD. Patients who achieved a CR had a decreased risk of relapse compared with non-CR patients (P = .044). However, PD occurred in 26% of patients who achieved a CR, in 57% who achieved a PR, and in 100% who achieved SD. A lower number of checkpoint inhibitor cycles received was associated with a risk of disease progression (P > .05); however, duration of treatment after best response was not associated with PD. The response rate to retreatment with checkpoint inhibitors was 75% in 8 of 14 patients who had PD.12
D’Angelo said, “This study asks a very important question of what the consequences are of stopping therapy. My takeaway from this study is that it’s a retrospective study so there are [limitations based on its design,] but these are the best data that exist in MCC and they’re valuable and very important data. Interestingly, the response rate to retreatment was 75%. If [therapy is stopped and the disease progresses], you can recapture a lot of those responses at the time of retreatment. These are small numbers and retrospective [data], so you have to be cautious with how you interpret and utilize that data. [In clinical practice], it’s all about having conversations with patients and fi guring out what’s important to them.”
Ongoing trials currently recruiting patients with MCC include the MERKLIN 1 (NCT04874831) and MERKLIN2 (NCT04393753) studies. MERKLIN 1 is a phase 2, open label, multicenter study evaluating the use of domatinostat, an oral class 1 HDAC inhibitor, in combination with avelumab in treatment-naïve patients with metastatic disease.13 MERKLIN2 is a phase 2, open label, multicenter, single-arm study evaluating the combination of domatinostat with avelumab in metastatic disease after progression on anti–PD-L1 antibody therapy. A total of 40 patients are expected to be enrolled in the MERKLIN2 trial.14 “These are important studies and ones that are currently enrolling, and I look forward to seeing these results,” D’Angelo said.
Other novel therapies being explored in MCC are transgenic T-cell receptor therapy and toll-like receptor agonists. Cavrotolimod, a spherical nucleic acid consisting of toll-like receptor 9 agonists, was recently designated as an orphan drug for the treatment of MCC based on preliminary results of a phase 1b trial.15 These results demonstrated potential activity with cavrotolimod in combination with pembrolizumab with no serious toxicity concerns. Cavrotolimod in combination with pembrolizumab will be evaluated in the phase 2 dose expansion phase in 2 patient cohorts, one with advanced or metastatic MCC and the other with advanced or metastatic CSCC.15
“Cavrotolimod requires intratumoral injection and the goal with all these approaches is to figure out ways to modify the immune microenvironment,” D’Angelo said. “I think the important question here is that we still don’t have good biomarkers of response to checkpoint blockade…. As a field, it’s really on us to…understand it better [which would] allow us to choose the right strategy but it seems that some sort of combinatorial strategy is where the field is headed,” she said.
Looking at the progress and future of targeted treatment in NMSC, Wong said, “The biggest unmet need now is in the PD-1–refractory space in skin cancer. The majority of patients do not achieve a longterm response and that’s unfortunate. The question is why? All these [novel treatment approaches] are percolating and it’s an incredibly exciting time. We will see the dominant hypothesis emerge and I’m not sure what it’s going to be. The recent drug approvals in melanoma tell us there are checkpoints yet to be discovered which may be effi cacious, so that whole area with second- and third-generation checkpoint inhibitors in the field is exciting now. What I tell patients is that there are opportunities and hope in [advanced and metastatic NMSC] where in the past this was an area that was one of the dark corners of oncology. For the first time we really see a glimmer of hope and what the hope is for not just response, but long-term, unmaintained, high-quality responses, which in layman’s terms translates to cure.”
References:
1. Villani A, Potestio L, Fabbrocini G, Scalvenzi M. New emerging treatment options for advanced basal cell carcinoma and squamous cell carcinoma. Adv Ther. 2022;39(3):1164-1178. doi:10.1007/s12325-022-02044-1
2. Migden MR, Chandra S, Rabinowits G, et al. CASE (CemiplimAb-rwlc Survivorship and Epidemiology) study in advanced cutaneous squamous cell carcinoma.Future Oncol. 2020;16(4):11-19. doi:10.2217/fon-2019-0762
3. Rohaan MW, Duizer ML, Devriese LA, Wilgenhof S, Van Herpen CM, Haanen JBA. Real-world data on clinical outcome and tolerability in patients with advanced cutaneous squamous cell carcinoma treated with cemiplimab in the Netherlands. Ann Oncol. 2021;32(suppl 5):S884-S885. doi:10.1016/j.annonc.2021.08.1447
4. Ruiz E, Chen CI, Zimmerman NM, Konidaris G, SongX.Real-world treatment patterns and outcomes of patients with metastatic cutaneous squamous cell carcinoma (mCSCC) in the US. Ann Oncol. 2021;32(suppl 5):S885. doi:10.1016/j.annonc.2021.08.1448
5. FDA approves expanded indication for Merck’s Keytruda (pembrolizumab) in locally advanced cutaneous squamous cell carcinoma (cSCC). News release. Merck. July 6, 2021. Accessed April 8, 2022. https://www.merck.com/news/fda-approves-expanded-indication-for-mercks-keytruda-pembrolizumab-in-locally-advanced-cutaneous-squamous-cell-carcinoma-cscc/
6. Marin-Acevedo JA, Withycombe B, Kim Y, et al. Efficacy of cetuximab after immunotherapy (IO) in advanced cutaneous squamous cell carcinoma (CSCC). J Clin Oncol. 2021;39(suppl15):9562. doi:10.1200/JCO.2021.39.15_suppl.9562
7. Munhoz RR, De Camargo VP, Marta GN, et al. CA209-9JC: aphase IIstudy of first-line nivolumab (NIVO) in patients (pts) with locally advanced or metastatic cutaneous squamous cell carcinoma. J Clin Oncol. 2020;38(suppl 15):10044.
8. Cowey CL, Chen CI, Aguilar KM, et al. Outcomes in patients (pts) with advanced basal cell carcinoma (aBCC) who discontinued hedgehog inhibitors (HHI) as first-line (1L) systemic treatment (Tx) in a U.S. community oncology setting: aretrospective observational study. J Clin Oncol. 2021;39(suppl15):e18742. doi:10.1200/JCO.2021.39.15_suppl.e18742
9. FDA approves cemiplimab-rwlc for locally advanced and metastatic basal cell carcinoma. FDA. February 9, 2021. Accessed April 8, 2022. Included in per protocol analysis (n=25)•Excluded from analysis due to compliance <705 with treatment (n=1)•Excluded from analysis due to lack of refrigeration of study medication(n=1) https://bit.ly/3JTtg5t
10. Kilgour JM, Shah A, Urman NM, et al. Phase II open-label, single-arm trial to investigate the efficacy and safety of topical remetinostat gel in patients with basal cell carcinoma.Clin Cancer Res. 2021;27(17):4717-4725. doi:10.1158/1078-0432.CCR-21-0560
11. Nghiem P, Bhatia S, Brohl AS, et al. Avelumab in patients with previously treated Merkel cell carcinoma (JAVELIN Merkel 200): updated overall survival data after more than five years of follow up. J Clin Oncol. 2021;39(suppl15):9517. doi:10.1200/JCO.2021.39.15_suppl.9517
12. Weppler AM, Da Meda L, Silva I. et al. Durability of response to immune checkpoint inhibitors (ICI) in metastatic Merkel cell carcinoma (mMCC) after treatment cessation. J Clin Oncol. 2021;39(suppl15):9543. doi:10.1200/JCO.2021.39.15_suppl.9543
13. Ascierto PA, van Akkooi ACJ, Nghiem P, Hermann F, Henneberg JP, Becker JC. A phase II, open label, multicenter study to investigate the efficacy and safety of domatinostat in combination with avelumab in patients with treatment-naive metastatic Merkel cell carcinoma:the MERKLIN 1 study. Ann Oncol. 2021;32(suppl 5):S901-S902. doi:10.1016/j.annonc.2021.08.1475
14. Van Akkooi ACJ, Ascierto PA, Nathan PD, et al. A phase II, open-label study to investigate the efficacy and safety of domatinostat in combination with avelumab in patients with advanced unresectable/metastatic Merkel cell carcinoma progressing on anti-PD-(L)1 antibody therapy: the MERKLIN 2 study. J Clin Oncol. 2021;39(suppl15):TPS9592. doi:10.1200/JCO.2021.39.15_suppl.TPS9592
15. Exicuregranted orphan drug designationby the U.S. Food and Drug Administration for cavrotolimod. News release. Exicure, Inc.March 3, 2021. Accessed March 29, 2022.https://bit.ly/3rKJHL9

Atlas Examines Tolerability of Hedgehog Pathway Inhibitors and Transition to IO in mBCC
October 16th 2024During a Case-Based Roundtable® event, Jennifer L. Atlas, MD, discussed treatment for a patient with basal cell carcinoma who reported challenging adverse events with hedgehog pathway inhibitor.
Read More
Tawbi Discusses the Role of Brain Metastases and PD-L1 Status in Melanoma
September 11th 2024During a Case-Based Roundtable® event, Hussein A. Tawbi, MD, PhD, and participants look at benefits of nivolumab combinations for brain metastases and PD-L1 positivity in the metastatic melanoma population in the second article of a 2-part series.
Read More