ICIs and Targeted Treatments Expand Role in mUC
Thomas Flaig, MD, addressed new and emerging systemic therapies for bladder cancer during the National Comprehensive Cancer Network 2022 Annual Conference.
Thomas W. Flaig, MD
The treatment landscape in advanced bladder cancer has been rapidly evolving over the past several years with the broad use of immune checkpoint inhibitors and the integration of antibody-drug conjugates (ADCs) and targeted therapy making their way into current regimens.
In 2015, first-line chemotherapy for metastatic bladder cancer consisted of gemcitabine and cisplatin and alternative regimens such as carboplatin- or taxane-based regimens. There were no standard therapies for second-line chemotherapies at that time.
Fast forward to 2022 and first-line systemic therapy for locally advanced or metastatic disease in cisplatin-eligible patients remains the same. In patients who are cisplatin-ineligible, preferred regimens include gemcitabine and carboplatin, followed by avelumab (Bavencio) maintenance therapy, atezolizumab (Tecentriq) in patients whose tumors express PD-L1, pembrolizumab (Keytruda) for patients who are platinum-ineligible, and a number of alternative therapies for specific circumstances, including ifosfamide (Ifex), doxorubicin, and gemcitabine.1
Thomas Flaig, MD, addressed new and emerging systemic therapies for bladder cancer during the National Comprehensive Cancer Network (NCCN) 2022 Annual Conference.2
Comparing 2015 to 2022, Flaig noted that today, there's a much more complicated clinical picture that emerges with a new crop of approaches.
In addition, in the second-line setting in locally advanced or metastatic disease, Flaig noted that the preferred treatment is pembrolizumab for patients post platinum. The number of alternative preferred regimens has also grown. “It’s important to maximize the optimal benefit of therapy for our patients,” said Flaig, vice chancellor of research for the University of Colorado Denver and the University of Colorado Anschutz Medical Campus.
Immune Checkpoint Inhibitors
“This has been an extremely active area over the last few years,” Flaig said. “The key theme is the integration of immune checkpoint inhibitors and is highlighted by the approval of pembrolizumab, which was the leading wave of approvals,” Flaig said.3,4 Pembrolizumab was evaluated as second-line therapy in patients with advanced urothelial cancer (NCT02256436) and demonstrated longer overall survival (OS) by about 3 months.
In the post-surgery setting, Flaig spotlighted NCT02632409, a phase 3 randomized trial evaluating nivolumab (Opdivo) vs placebo in patients with high-risk muscle-invasive urothelial carcinoma after radical surgery.5 Findings revealed that disease-free survival was longer with adjuvant nivolumab than with placebo and among patients with a PD-L1 expression level of 1% or more.
Powles et al demonstrated that avelumab plus best supportive care significantly prolonged OS, compared with best supportive care alone, among patients with urothelial cancer.6 In the avelumab group, OS was determined to be 71.3% in 1 year vs 58.4% in the control group. Median OS was 21.4 months vs 14.3 months (HR, 0.69; 95% CI, 0.56-0.86; P = .001). The agent also prolonged OS in the PD-L1-positive population; OS at 1 year was 79.1% in the avelumab group and 60.4% in the control group (HR, 0.56; 95% CI, 0.40-0.79; P < .001).
The median progression-free survival (PFS) was 3.7 months in the avelumab group and 2.0 months in the control group in the overall population (HR, 0.62; 95% CI, 0.52-0.75) and 5.7 months and 2.1 months, respectively, in the PD-L1-positive population (HR, 0.56; 95% CI, 0.43-0.73).
“Immune checkpoint inhibitors have had a dramatic [effect] on the way we treat and think about patients with bladder cancer,” Flaig said.
Antibody-Drug Conjugates
Two ADCs are currently approved: enfortumab vedotin-ejfv (Padcev) and sacituzumab govitecan-hziy (Trodelvy).
Enfortumab vedotin-ejfv was granted approval in July 2021 based on results from EV-301 (NCT03474107) and evaluated the ADC vs investigator’s choice of single-agent chemotherapy, which could be docetaxel, paclitaxel, or vinflunine.7
Median OS was 12.9 months (95% CI, 10.6-15.2) for patients on the treatment arm (n = 301) vs 9.0 months for those receiving chemotherapy (n = 307) (95% CI, 8.1-10.7) (HR, 0.70; 95% CI, 0.56-0.89; P = .0014).8
In the trial, the median PFS was 5.6 months (95% CI, 5.3-5.8) compared with 3.7 months (95% CI, 3.5-3.9), respectively (HR 0.62; 95% CI, 0.51-0.75; P < .0001).
The ORR was 40.6% (95% CI, 34.9%-46.5%) vs 17.9% (95% CI, 13.7%-22.8%), respectively (P < .0001).8
An accelerated approval for sacituzumab govitecan-hziy was granted in April 2021, after efficacy and safety of the ADC were evaluated in the TROPHY-U-01 trial (NCT03547973).9 Patients with locally advanced or metastatic urothelial carcinoma were evaluated.
Investigators reported that the confirmed ORR was 27.7% (95% CI, 19.6%-36.9%) with 5.4% complete responses and 22.3% partial responses. The median duration of response was 7.2 months (95% CI, 4.7-8.6), according to the investigators.10
Targeted Therapy
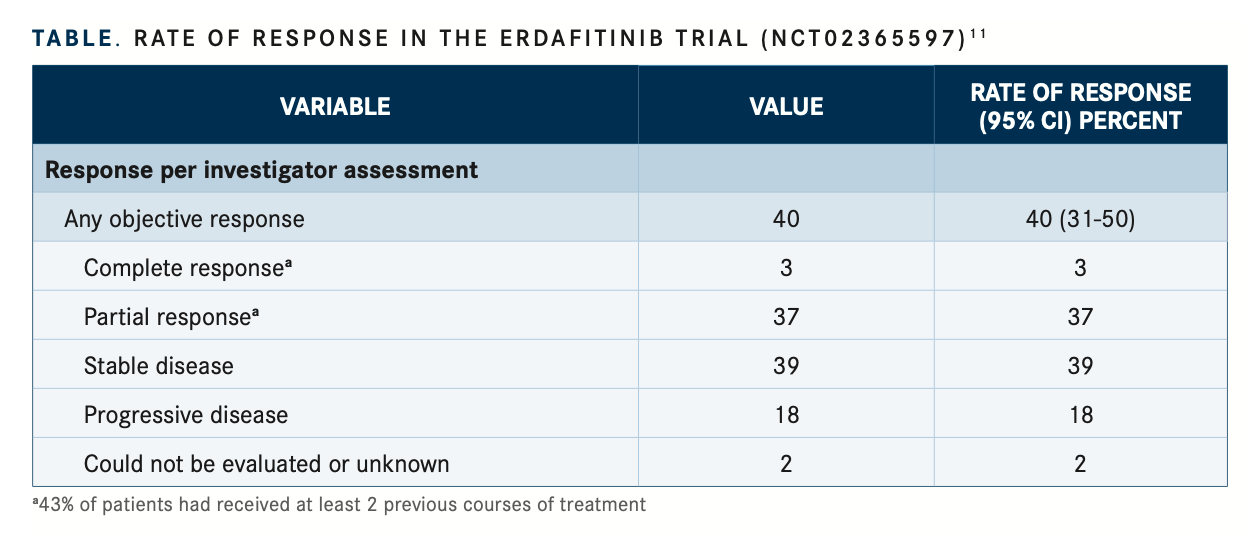
The tyrosine kinase inhibitor of FGFR1-4, erdafitinib (Balversa), was evaluated in an open-label phase 2 study (NCT02365597), patients who had locally advanced and unresectable or metastatic urothelial carcinoma with prespecified FGFR alterations were randomly assigned to receive erdafitinib in either an intermittent or a continuous regimen in the dose-selection phase of the study.11
Investigators reported the rate of confirmed response to erdafitinib therapy was 40%; it was determined that 3% of patients had a complete response and 37% had a partial response (TABLE11). Among the 22 patients who had undergone previous immunotherapy, the confirmed response rate was 59%. The median duration of progression-free survival was 5.5 months, and the median duration of OS was 13.8 months.11
“Currently, we have a much more complicated picture of how we think about our patients with metastatic bladder cancer,” Flaig said. “Our objective now [compared with 2015] is to try to align the optimal therapies with our patients.”
References
1. NCCN. Clinical Practice Guidelines in Oncology. Bladder cancer, version 1.022. Accessed April 13, 2022. https://bit.ly/3Efmwhh
2. Flaig TW.New treatment options for patients with bladder cancer. Presented at NCCN 2022 Annual Conference, March 31-April 2, 2022.Accessed April 12, 2022. https://bit.ly/3jzFdmh
3. Pembrolizumab (Keytruda): advanced or metastatic urothelial carcinoma. FDA. Updated May 19, 2017. Accessed April 13, 2022. https://bit.ly/3JM7UH8
4. Bellmunt J, de Wit R, Vaughn DJ, et al. Pembrolizumab as second-line therapy for advanced urothelial carcinoma. N Engl J Med. 2017;376(11):1015-1026. doi:10.1056/NEJMoa1613683
5. Bajorin DF, Witjes JA, Gschwend JE, et al. Adjuvant nivolumab versus placebo in muscle-invasive urothelial carcinoma. N Engl J Med. 2021;384(22):2102-2114. doi:10.1056/NEJMoa2034442
6. Powles T, Park SH, Voog E, et al. Avelumab maintenance therapy for advanced or metastatic urothelial carcinoma. N Engl J Med. 2020;383(13):1218-1230. doi:10.1056/NEJMoa2002788
7. FDA grants regular approval to enfortumab vedotin-ejfv for locally advanced or metastatic urothelial cancer.FDA. Updated July 9, 2021. Accessed April 13, 2022. https://bit.ly/3O9HiDj
8. Powles T, Rosenberg JE, Sonpavde GP, et al. Enfortumab vedotin in previously treated advanced urothelial carcinoma. N Engl J Med. 2021;384(12):1125-1135. doi:10.1056/NEJMoa2035807
9. FDA grants accelerated approval to sacituzumab govitecan for advanced urothelial cancer. FDA. Updated April 13, 2021. Accessed April 13, 2022. https://bit.ly/3KHdBHv
10.Tagawa ST, Balar AV, Petrylak DP, et al. TROPHY-U-01: A phase IIopen-label study of sacituzumabgovitecan in patients with metastatic urothelial carcinoma progressing after platinum-based chemotherapy and checkpoint inhibitors. J Clin Oncol. 2021;39(22):2474-2485. doi:10.1200/JCO.20.03489
11. Loriot Y, Necchi A, Park SH, et al. Erdafitinib in locally advanced or metastatic urothelial carcinoma. N Engl J Med. 2019;381(4):338-348. doi:10.1056/NEJMoa1817323

Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More