Genomic Complexity in CLL Is Detected With Optical Genome Mapping
Optical genome mapping may help to detect genetic abnormalities in patients with CLL.
A study presented during the 2021 International Workshop on Chronic Lymphocytic Leukemia (CLL) showed the potential for effective detection of many genomic abnormalities in patients with CLL via optical genome mapping (OGM).
OGM detected 88% (n = 184) of previously known abnormalities and provided additional structural information in 45% (n = 19) of patients, most of which were associated with microarray copy number alternations (CNAs) or unknown cytogenetic elements reported by chromosome banding analysis (CBA).
Discordances in OGM were mainly found in patients with complex karyotypes (CKs) and occurred because of a CNA sensitivity of around 20% (n = 13; 45%), CNA masked regions (n = 2; 7%), CNA complex chromosomal microarray (CMA) profile (n = 3; 10%), a rearrangements sensitivity of around 5% (n = 2; 7%), rearrangements centromeric breakpoints (n = 7; 24%), and other (n = 2; 7%).
Curated results from OGM still detected a higher complexity compared with CBA and CMA; however, OGM demonstrated a good correlation with the other technologies (rp = .69; rp = .81, respectively). Patients with CK demonstrated significantly higher genomic complexity (P < .01).
Notably, OGM detected new balanced rearrangements, particularly among patients with CK, that should be further validated.
“Further studies are required to define genomic complexity criteria by OGM and implement this technique in the routine management of patients with CLL,” lead study author Anna Puiggros, a medical associate for the pathology service at Hospital del Mar and a member of the Translational Research Group in Hematological Neoplasms at the Institut Hospital del Mar d’Investigacions Mèdiques, in Barcelona, Spain, and coauthors wrote in the poster.
CK is defined as the presence of at least 3 chromosomal aberrations in the same clone by CBA. In CLL, the presence of CK predicts for poor prognosis.
CBA, CMA, and fluorescence in situ hybridization (FISH) are current standard methods for risk stratification and identifying CK in patients with CLL; however, each method is associated with intrinsic limitations.
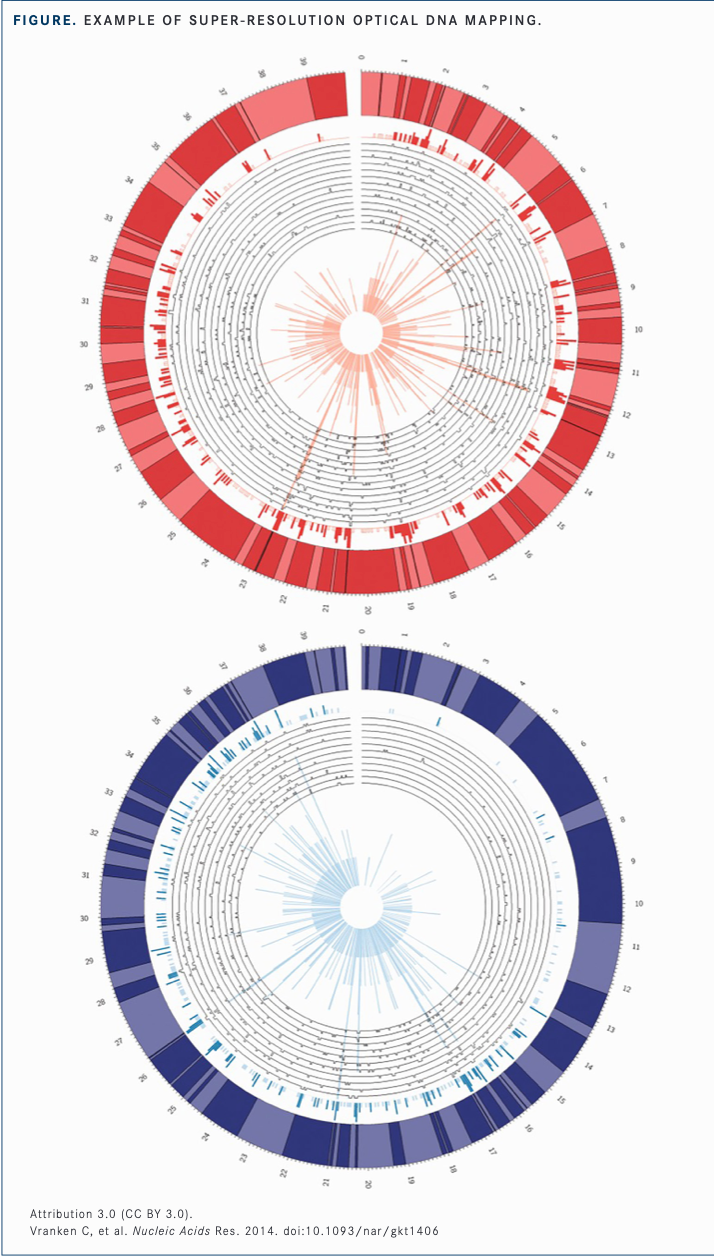
OGM is a novel method of risk stratification that relies on the imaging of long DNA molecules of greater than 250 kbp that has the potential to overcome some of the limitations associated with the aforementioned technologies. With OGM, long DNA molecules are labeled at specific sequences across the genome and imaged by a high-throughput, high-resolution machine. The resulting information features a map of the genomic location of every molecule that detects chromosomal abnormalities based on label patterns vs a reference genome and the number of molecules mapped in each region.
The goals of this study were “to compare the results obtained by OGM with previous CBA and CMA information [and] to analyze the usefulness of OGM in the assessment of genomic complexity in patients with CLL,” Puiggros and coauthors wrote.
In the study, investigators analyzed 42 patients with CLL, 18 of whom carried CK by CBA. Patients were a median age of 66 years, and the majority (67%) were male. Sixteen percent of patients had Binet stage B or C disease.
Genomic Complexity Comparisons
Overall, 27 patients had low-complexity by OGM (LC-OGM) defined as less than 10 abnormalities, and 15 patients had high-complexity by OGM (HC-OGM) defined as 10 or more abnormalities.
The median time from diagnosis to OGM was 4 months in the LC-OGM cohort (range, 0-51) vs 18 months in the HC-OGM cohort (range, 0-54; P = .623). The median number of abnormalities identified by OGM was 6 (range, 2-9) vs 28 (range, 10-77), respectively (P < .001). Patients had a median of 2 (range, 0-7) vs 10 (range, 1-29) CNAs identified by CBA (P = .001), respectively, and a median of 3 (range, 0-5) vs 17 (range, 5-48) translocations, respectively (P < .0 01).
Genomic complexity by conventional methods in the LC-OGM cohort vs the HC-OGM cohort revealed that 25.9% (n = 7) vs 73.3% (n = 11), respectively (P= .004), had CK by CBA, defined as at least 3 abnormalities; 3.7% (n = 1) vs 60% (n = 9), respectively (P< .001), had high CK by CBA defined as at least 5 abnormalities; 7.4% (n = 2) vs 53.3% (n = 8), respectively (P = .001), had high genomic complexity by CMA, defined as at least 5 abnormalities including all classical CLL CNA abnormalities (n = 40); 7.4% (n = 2) vs 80% (n = 12), respectively (P < .001), had high complexity by CBA and or CMA defined as at least 5 alterations; and 0% vs 53.3% (n = 8), respectively (P < .001), had chromothripsis.
In the LC-OGM cohort vs the HC-OGM cohort, FISH testing identified 13q deletions in 74.1% (n = 20) vs 66.7% (n = 10) of patients, respectively (P= .434); trisomy 12 in 22.2% (n = 6) vs 13.3% (n = 2) of patients, respectively (P= . 39 5) ; 11q deletions/ATM mutations in 29.6% (n = 8) vs 26.7% (n = 4) of patients, respectively (P= . 5 6 6) ; 17p deletions/TP53 mutations in 3.7% (n = 1) vs 40% (n = 6) of patients, respectively (P= .002); and TP53 abnormalities in 3.7% (n = 1) vs 46.7% (n = 7) of patients, respectively (P= . 0 0 5) .
Of evaluable patients with unmutated IGHV (n = 38), 51.9% (n = 14) of patients in the LC-OGM cohort compared with 60% (n = 9) of patients in the HC-OGM cohort had unmutatedIGHV (P= .495).
Finally, in the LC-OGM cohort, 51.9% (n = 14) of patients were treated, the median time to first treatment was 53 months (95% CI, 2.7-83.3), and the median follow-up time was 45 months (range, 0-95). In the HC-OGM cohort, 80% (n = 12) of patients were treated (P = .069), the median time to first treatment was 2 months (95% CI, 0.5-11. 5; P = .018), and the median follow-up time was 31 months (range, 0-82; P = .025).
Tumor DNA from peripheral blood was also analyzed by OGM; abnormalities identified by OGM were compared with available CBA, FISH, and CMA results. Additionally, clinical-biological characteristics and time-to-first treatment (TFT) were evaluated based on the complexity identified by OGM.
Further results showed that, as a continuous variable, the number of alterations defined by OGM demonstrated a concordance index for TFT (c-index = 0.623) that was similar to that observed with CBA (c-index = 0.602) and CMA (c-index = 0.657).
Additionally, patients with 10 or more alternations identified by OGM demonstrated a worse clinical evolution.
REFERENCE
1. Puiggros A, Ramos-Campoy S, de la Rosa M, et al. Optimal genome mapping: a new promising tool to assess genomic complexity in chronic lymphocytic leukemia (CLL). Presented at: 2021 International Workshop on Chronic Lym-phocytic Leukemia; September 17-20, 2021; virtual. Poster 1084272. https://bit.ly/3koE0Q0















