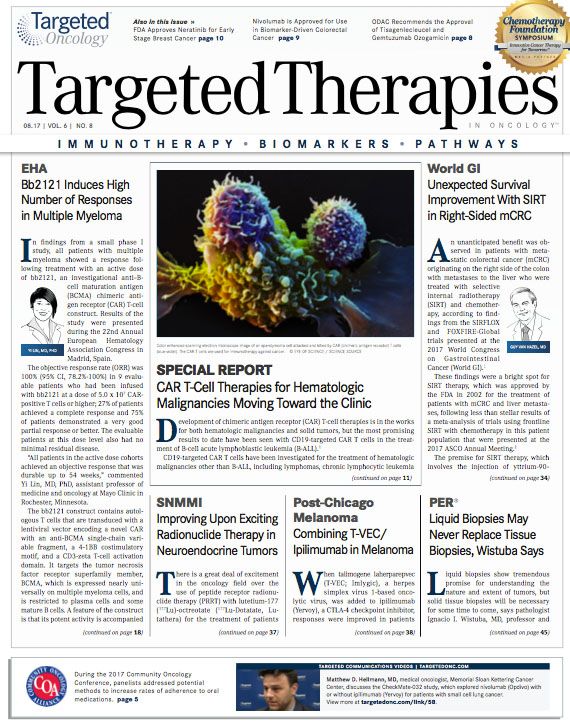
CAR T-Cell Therapies for Hematologic Malignancies Moving Toward the Clinic
Development of chimeric antigen receptor T-cell therapies is in the works for both hematologic malignancies and solid tumors, but the most promising results to date have been seen with CD19-targeted CAR T cells in the treatment of B-cell acute lymphoblastic leukemia.
1
CD19-targeted CAR T cells have been investigated for the treatment of hematologic malignancies other than B-ALL, including lymphomas, chronic lymphocytic leukemia (CLL), and multiple myeloma. CAR T cells directed at other targets that may be more appropriate for non−B-ALL hematologic malignancies, such as CD22 and CD30 for lymphomas, immunoglobulin-kappa for CLL, CD33 and others for acute myeloid leukemia, and B-cell maturation antigen (BCMA) for multiple myeloma, are also in development.1
CAR T-CELL THERAPY FOR RELAPSED/REFRACTORY PEDIATRIC B-ALL
CARs contain an extracellular domain, such as a single-chain antibody variable fragment that recognizes a specific target antigen, which is linked to an intracellular T-cell signaling domain that stimulates T-cell proliferation, lysis of the cells expressing the target antigen, and cytokine release syndrome (CRS). CAR T cells are currently generated from a patient’s own T cells, although they could be created using allogeneic donor cells.
Tisagenlecleucel (CTL019), a CAR T-cell therapeutic that targets CD19,2was developed at the University of Pennsylvania for the treat- ment of B-ALL; it is being commercialized by Novartis Oncology.3
Tisagenlecleucel received a breakthrough therapy designation from the FDA in March.3On July 12, the 10 members of the Oncologic Drugs Advisory Committee (ODAC) of the FDA unanimously voted to recommend approval of Novartis Pharmaceuticals’ biologics license application (BLA) for tisagenlecleucel for the treatment of patients aged 3 to 25 years with relapsed/refractory B-cell ALL.2,3This vote was based on a phase II study of a single intravenous infusion of tisagenlecleucel in 68 patients with relapsed or refractory acute B-cell ALL, of whom 63 were evaluable for efficacy. The overall remission rate (ORR) was 82.5%. Grade 3 and 4 CRS occurred in 47% of the safety population (n = 68). No deaths occurred.2Other serious adverse events (AEs) included hemophagocytic lymphohistiocytosis, neurologic events, and life-threatening infections.
Prakash Satwani, MD, called the use of tisagenlecleucel in treating children with relapsed or refractory ALL one of the great successes in modern medicine. “Here, for the first time, we are witnessing the introduction of completely novel genetically engineered T cells that can most likely cure otherwise refractory and fatal disease. We expect that in the near future, harnessing the power of the immune system will bring more curative options for patients with aggressive cancers,” said Satwani, associate professor of pediatrics, Division of Pediatric Hematology, Oncology, and Stem Cell Transplantation, NewYork-Presbyterian/Columbia University Medical Center, in New York, New York.
OTHER CAR T-CELL THERAPIES IN DEVELOPMENT
Kite Pharma has reported results of axicabtagene ciloleucel (KTE-C19), a CAR T-cell targeting CD19 in adults with high-burden relapsed/refractory ALL, with 73% of 11 patients in complete remission in the ZUMA-3 phase I/II trial.4The agent also demonstrated positive findings in the ZUMA-1 study of patients with refractory non-Hodgkin lymphomas, including diffuse large B-cell lymphoma, primary mediastinal lymphoma, and transformed follicular lymphoma.5The objective response rate was 82% in 101 patients, with 54% achieving a complete response. However, 1 patient on the ZUMA-1 trial died because of cerebral edema, the manufacturer disclosed. A BLA is pending with the FDA for axicabtagene ciloleucel for the treatment of patients with aggressive non-Hodgkin lymphoma.
Another CAR T-cell therapy for ALL targeting CD19 has fared far worse. A phase II trial of Juno Therapeutics’ JCAR015 in adult relapsed/refractory ALL was put on hold after 5 deaths from cerebral edema in the phase II ROCKET study. The study was placed on a hold by the FDA in July 2016 and again in November 2016 because of the severe toxicities associated with JCAR015, and development of this agent has since been discontinued by the manufacturer. The company is investigating other CAR T-cell therapies, including JCAR017, which is being studied in patient with relapsed/refractory diffuse large B-cell lymphoma. JCAR017 has already demonstrated an 80% ORR and a 60% complete response rate in this setting.6
Although CAR T cells targeting CD19 have been tested in patients with multiple myeloma, results were mixed, and other targets (ie, B-cell maturation antigen [BCMA]) have been shown to be more appropriate. Unlike B-ALL, which is sometimes curable with chemotherapy and steroids, particularly in children, multiple myeloma remains incurable. Several groups are testing BCMA CAR T cells in adults with multiple myeloma.7,8Toxicity has been considerable. Responses seem to be correlated with BCMA CAR T-cell expansion, and studies are ongoing to determine strategies to improve expansion and persistence.8
Another BCMA-targeting CAR, LCAR-B38M, has been administered to 35 patients with relapsed/refractory multiple myeloma in early results of a phase I study, with a reported 94% ORR, although further follow-up is needed. CRS, which occurred in most patients, was said to be generally mild and manageable in most cases.9
OBSTACLES TO CAR T-CELL THERAPY
Off-target activity, accurate determination of appropriate targets, production time from cell collection to infusion, and the serious toxicities associated with CAR T-cell therapies are obstacles to their development and widespread use.
The most common and well-characterized AE associated with CAR T-cell therapy is CRS, a systemic inflammatory response caused by cytokines released by the therapeutic T cells. Neurologic symptoms may also occur with or without CRS.10
The cytokines responsible for CRS may be produced by the infused CAR T cells or by other immune cells in response to those produced by the CAR T cells, and include interleukins (ILs), interferon, C-reactive protein, and tumor necrosis factor. In CRS, multiple organ systems are affected. CRS can lead to high fever, tachycardia, hypotension, pulmonary edema, acute renal impairment, cytopenias, infections, and other toxicities. Monitoring and supportive-care interventions can be used to manage CAR T-cell therapy−associated toxicities, including the use of the anti−IL-6 receptor monoclonal antibody tocilizumab and corticosteroids.10
B-cell malignancies are amenable to CAR T-cell therapies because targeting CD19 destroys B cells; the end result is permanent loss of normal B cells (B-cell aplasia). The resulting loss of antibody production can be treated with immunoglobulin infusions, which may be a life-long requirement. In other types of malignancies, seemingly appropriate targets might overlap with antigens on normal tissues that have irreplaceable functions. In acute myeloid malignancies, for example, targeting CD33 could lead to the elimination of normal myelopoiesis. Construction of CAR T cells with suicide genes could overcome this obstacle. If CAR T cells could be completely removed after therapy, a universal off-the-shelf agent might be constructed as a universal donor CAR T-cell product, reducing the wait time to therapy.11
It remains to be seen whether CAR T-cellbased therapy will be the best strategy for multiple myeloma. An early study of GSK2857916, an antibody−drug conjugate directed against BCMA, showed promising results in an early study of patients with relapsed/refractory multiple myeloma.12The agent was well tolerated, and no dose-limiting toxicities were found in part 1 of the phase I study. Although CAR T-cellbased therapies have the potential for long-term durable remission with a single treatment, the antibody−drug conjugate is off-the-shelf, so no manufacturing or wait time is needed, and many more patients could be treated with this modality.
Swaminathan P. Iyer, MD, professor of medicine, Institute for Academic Medicine, Houston Methodist Cancer Center, Weill Cornell Medical College, in Houston, Texas, said the deaths associated with CAR T-cell therapy that have been reported require that the safety data be examined carefully. He suggested that looking at the different types of chemotherapy administered before CAR T-cell therapy as well as at the particular CAR T-cell product may offer clues.
UNANSWERED QUESTIONS
There are many unanswered questions regarding CAR T-cell therapy, including whether there are unknown serious AEs that may develop in long-term survivors; whether combination therapy with chemotherapy, immunotherapy, or other agents may improve the efficacy in some settings; what treatment could follow failure of CAR T-cell therapy if effective off-the-shelf therapies could reduce time to infusion and could be developed; and what the true cost of these therapies will be.
It is not known if the gene therapy vectors used in CAR T-cell therapies are able to replicate independently or cause a secondary cancer via insertional mutagenesis, although to date these have not been reported.10The potential for the generation of replication-competent retrovirus and genotoxicity from insertional mutagenesis leading to secondary malignancies such as secondary leukemias, was not identified in the tisagenlecleucel registration study, in part because the follow-up was short.2
Combination trials adding to CAR T-cell therapy are already being explored in early stages in small numbers of patients, including of CAR T-cell therapies administered with the kinase inhibitor ibrutinib (Imbruvica) for CLL,13or the antiPD-1 monoclonal antibody pembrolizumab (Keytruda) in ALL,14in attempts to improve response and CAR T-cell resistance. Both combinations were found to be safe and warrant future study.13,14
Better selection of targets for CAR T cells may reduce “on target, off tumor” toxicities, (ie, attacking healthy cells or tissues that express the same antigens as the tumor cells). For example, in CLL, use of the immunoglobulin M Fc receptor may be a more selective target than the currently investigated CD19.15
Another CAR T-cell therapy that targets CD22 is being developed for children and young adults whose leukemia escapes CD19 CAR T-cell therapy. It is being explored in the phase I PLAT-04 study of young patients with relapsed/refractory CD22-positive ALL. An additional strategy of future studies will be to create CAR T cells that recognize both CD19 and CD22 simultaneously to determine whether that can help prevent relapse.16
Patients receiving CAR T-cell therapy will be monitored for at least a year, although they may require lifelong immunoglobulin administration, according to Satwani. He expects administration of tisagenlecleucel to be restricted to the implementation sites and speculated that they were selected because of their “strong ICU [intensive care unit] infrastructure,” given that many patients will require ICU care.
For tisagenlecleucel, both a prospective registry and a monitoring study have been proposed to assess long-term safety for up to 15 years post treatment.2The prospective registry study will evaluate short- and long-term AEs of interest, and monitor the incidence and outcome of any pregnancy, hematologic and secondary malignancies, B-cell aplasia, and replication-competent retroviruses and/or lentiviruses arising from the vector used to construct the CAR T cells.
The primary objective of the long-term follow-up is to assess the safety of long-term exposure to tisagenlecleucel, including new malignancies, new incidence or exacerbation of preexisting neurologic disorders, prior rheumatologic or autoimmune disorders, and new incidence of a hematologic disorder. Secondary objectives of the long-term follow-up study include monitoring the persistence of the CAR T cells in peripheral blood, determining the presence of replication-competent retroviruses in the peripheral blood, determining the long-term efficacy of tisagenlecleucel (including the rates of relapse and progression for patients who did not have relapse or progression at study entry), the incidence of death, and lymphocyte levels. For patients younger than 18 at the time of initial treatment with tisagenlecleucel, growth, development, and female reproductive status will also be monitored. It will be a considerable time before these results will be available, and they will go a long way to contributing to our understanding of this unique therapeutic approach.
Although Satwani estimated a 3- to 4-week manufacturing time for tisagenlecleucel, Iyer believes that the “door to door” time to collect patient T cells and engineer the product will be 4 to 6 weeks. Patients will require reasonable disease control during this process, and there will be patients who will require other treatment if their disease returns or worsens before their CAR T cells are ready for administration.
The cost of tisagenlecleucel may not be available until FDA approval. Estimates from Satwani and Iyer range from $300,000 to $700,000; the overall cost will be higher if chemotherapy prior to CAR T-cell therapy and emergency department, inpatient, or ICU care to manage AEs are taken into consideration.
LOOKING AHEAD
Having been approved by the ODAC, the licensing application for tisagenlecleucel will now be considered by the full FDA. Approval of the current indication of this agent could advance the development of additional indications and provide momentum for the development of additional CAR T-cell therapies. The use of these agents will require experience, and the results of additional studies of newer agents and combinations are awaited.
Iyer noted that the training of personnel and the infrastructure of the administration site are important, and not every oncologist will be able to administer this therapy. Groups like the Foundation for the Accreditation of Cellular Therapy have set up guidelines for administration of immune effector cells including CAR T cells.17
If tisagenlecleucel receives accelerated approval, additional studies will be required, as they will if tisagenlecleucel or other CAR T-cell therapies are to be used earlier in the course of disease and in older patients.
Iyer commented that childhood and adult ALLs are very different diseases, and for adults, “CAR T cells upfront are a thing of the future,” requiring randomized, controlled studies compared with transplantation before being confirmed for clinical practice. Although younger patients are able to tolerate more adverse effects, “slowly extending the ages to 40 years, and perhaps older, [is something] we expect to see,” he concluded. “Although we are very excited, both safety and ef cacy are important. We have to proceed cautiously with what we have.”
References:
- Jackson HJ, Ra q S, Bentjens RJ. Driving CAR T-cells forward. Nat Rev. Clin Onc. 2016;13:370-383. doi: 10.1038/nrclinonc.2016.36.
- FDA Brie ng Document. Oncologic Drugs Advisory Committee Meeting. BLA 125646: Tisagenlecleucel. July 12, 2017. www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMateri- als/Drugs/OncologicDrugsAdvisoryCommittee/UCM566166.pdf. Accessed July 27, 2017
- Novartis CAR-T cell therapy CTL019 unanimously (10-0) recommended for approval by FDA ad- visory committee to treat pediatric, young adult r/r B-cell ALL [media release]. Basel, Switzerland: Novartis International AG; July 12, 2017. www.novartis.com/news/media-releases/novartis-car-t- cell-therapy-ctl019-unanimously-10-0-recommended-approval-fda. Accessed July 27, 2017
- Shah BD, Wierda WG, Schiller GJ, et al. Updated results from ZUMA-3, a phase 1/2 study of KTE-C19 chimeric antigen receptor (CAR) T cell therapy, in adults with high-burden relapsed/refrac- tory acute lymphoblastic leukemia (R/R ALL).J Clin Oncol. 2017;35(suppl; abstr 3024).
- Locke FL, Neelapu SS, Bartlett NL, et al. Primary results from ZUMA-1: a pivotal trial of axicabta- gene ciloleucel (Axi-cel; KTE-C19) in patients with refractory aggressive non-Hodgkin lymphoma (NHL). Presented at: 2017 AACR Annual Meeting; April 1-5, 2017; Washington, DC. Abstract CT019.
- Juno Therapeutics reports fourth quarter and 2016 nancial results. March 1, 2017. ir.junothera- peutics.com/phoenix.zhtml?c=253828&p=irol-newsArticle&ID=2250772. Accessed July 27, 2017.
- Ali SA, Shi V, Maric I. T cells expressing an anti-B-cell maturation antigen chimeric antigen re- ceptor cause remissions of multiple myeloma.Blood.2016;128(13):1688-1700. doi: 10.1182/ blood-2016-04-711903.
- Cohen AD, Garfall AL, Stadtmauer EA, et al. B-cell maturation antigen (BCMA)-speci c chimeric antigen receptor T cells (CART-BCMA) for multiple myeloma (MM): initial safety and e cacy from a phase I study.Blood.2016;128(22):1147.
- Fan X, Zhao W, Liu J, et al. Durable remissions with BCMA speci c chimeric antigen recep- tor (CAR)-modi ed T cells in patients with refractory/relapsed multiple myeloma.J Clin Oncol.2017;35(suppl; abstr LBA3001).
- Brudno JN, Kochenderfer JN. Toxicities of chimeric antigen receptor T cells: recognition and management. Blood. 2016;127(26):3321-3330. doi: 10.1182/blood-2016-04-703751.
- Dunbar CE. Blood’s 70th anniversary: CARs on the blood highway.Blood.2016;128(1):1-3. doi: 10.1182/blood-2015-10-635334.
- Cohen AD, Popat R, Trudel S, et al. First in human study with GSK2857916, an antibody drug conjugated to microtubule-disrupting agent directed against B-cell maturation antigen (BCMA) in patients with relapsed/refractory multiple myeloma (MM): results from study BMA117159 part 1 dose escalation.Blood.2016;128(22):1148.
- Gill S, Frey NV, Hexner EO, et al. CD19 CAR-T cells combined with ibrutinib to induce complete remission in CLL.J Clin Oncol. 2017;35(suppl; abstr 7509).
- Maude SL, Hucks GE, Seif AE, et al. The e ect of pembrolizumab in combination with CD19-tar- geted chimeric antigen receptor (CAR) T cells in relapsed acute lymphoblastic leukemia (ALL).J Clin Oncol.2017;35(suppl; abstr 103).
- Faitschuk E, Hombach AA, Frenzel LP, et al. Chimeric antigen receptor T cells targeting Fc μ re- ceptor selectively eliminate CLL cells while sparing healthy B cells.Blood.2016;128(13):1711-1722. doi: 10.1182/blood-2016-01-692046.
- Seattle Children’s opens CD22 CAR T-cell immunotherapy trial for children and young adults whose leukemia escapes CD19 CAR T-cell therapy [press release]. Seattle, WA: Seattle Children’s; July 27, 2017. www.newswise.com/articles/seattle-children-s-opens-cd22-car-t-cell-immunother- apy-trial-for-children-and-young-adults-whose-leukemia-escapes-cd19-car-t-cell-therapy. Accessed July 28, 2017.
- FACT-JACIE International Standards for Hematopoietic Cellular Therapy Collection, Processing, and Administration. Fifth Edition. factwebsite.org/uploadedFiles/FACT_News/Immune%20E ec- tor%20Cell%20Standards%202.1.17.pdf. Accessed July 27, 2017.
Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More