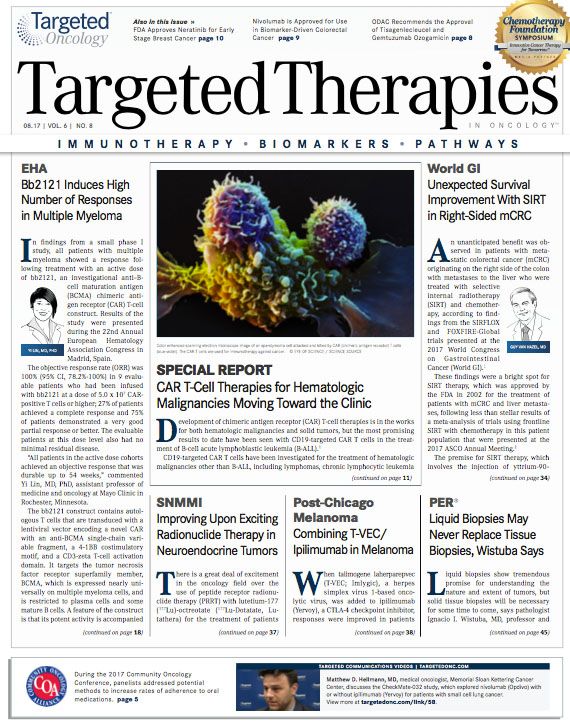
Liquid Biopsies May Never Replace Tissue Biopsies, Wistuba Says
Tissue samples will continue to be necessary in the practice of immunotherapy as more biomarkers for cancer become known, and solid biopsies remain the prime means of assessing the presence of cancer, says Ignacio I. Wistuba, MD.
Ignacio I. Wistuba, MD
Liquid biopsies show tremendous promise for understanding the nature and extent of tumors, but solid tissue biopsies will be necessary for some time to come, says pathologist Ignacio I. Wistuba, MD, professor and chair, Department of Translational Molecular Pathology, Division of Pathology/Lab Medicine, MD Anderson Cancer Center.
Although liquid biopsies have high sensitivity for detecting abnormalities in the bloodstream, they do not catch everything. Clinicians must still rely on tissue samples when the liquid biopsy is negative. When it comes to patients with metastases, the liquid biopsy is believed to capture the genomic information from multiple tumor sites, although this has not been proved beyond doubt, Wistuba said.
Tissue samples will continue to be necessary in the practice of immunotherapy as more biomarkers for cancer become known, and solid biopsies remain the prime means of assessing the presence of cancer, he said. Ideally, liquid biopsies could replace solid tissue samples in this context in the future because of the convenience that would represent.
He discussed this issue and other developments in pathology in an interview withTargeted Oncologyat the Inaugural International Congress on Oncology Pathology, hosted by the Physicians’ Education Resource® (PER®).
The FDA’s approval of the Philips IntelliSite Pathology Solution (PIPS), which allows for analysis of digitized surgical pathology slides, and the use of similar technology from other manufacturers, represents a huge step forward in convenience for pathology, Wistuba explained.
No longer will clinicians have to rely on libraries of glass slides kept in expensive storage facilities, as digitized images can be called up on a computer screen in an instant. Clinicians can review these images without having to peer through microscopes, and they can label them easily and clearly so other clinicians can review their work and understand how they reached their conclusions, Wistuba said.
TARGETED ONCOLOGY:How do you define large-scale genomic analysis?
Wistuba:Large-scale genomic analysis is the use of tumor cells to study the whole genomethe exons and introns of the genes. Studying the entire gene is very informative from the discovery perspective, but it’s time-consuming and expensive, and you’re not going to find anything additional that would be useful for a patient for practical purposes. The other option is whole exome sequencing, in which you study only the exons. That is still too expensive and too laborious, and it doesn’t help a patient more.
Some people may also include targeted sequencing of the RNA. That gets even more complicated. It’s part of the clinical practice in many places around the world, and you’re studying with the same next-generation technology, but people go from 50 to 400 genes, and you get practical information for treatment of the patients by doing that. The targeted approach is faster and less expensive because you are analyzing fewer regions of the genome. You can go deeper with the analysis and improve sensitivity. You can detect abnormalities that can be very low percentages in a tumor in the whole exome/whole genome sequencing.
TARGETED ONCOLOGY:What are the advantages of using panels to do genotyping in solid tumors?
Wistuba:Not only can we integrate specific abnormality mutations, amplications, translocations, and deletions that we know about, but we can also examine large regions of the DNA of genes of interest and identify additional ones that may help patients to get a targeted therapy. We can also find opportunities to get patients on clinical trials using those abnormalities as an inclusion criteria.
TARGETED ONCOLOGY:In your opinion, will liquid biopsies replace tumor samples for diagnostic purposes in any solid tumors?
Wistuba:No, I don’t think so, but I have a bias. For me, tissue is the source of discovery and information. When we talk about cell-free DNA or cell tumor DNA genotyping, the sensitivity is still about 80%, which means you’re missing 20% of abnormalities.
The counterargument is that when you have metastases and the tumor may be different, the liquid biopsy may represent the entire tumor for a person. However, nobody has shown that all these tumors are shedding DNA to the blood. In theory, that’s what happens, but nobody has shown that to be true.
In my opinion, with the use of immunotherapy to treat patients and the potential development of biomarkers to predict response to immunotherapy, we’re going to need tissue to do that analysis. Even if from a genomic perspective you could say that in 80% of the cases, a liquid biopsy is going to give us all the information we need, I would say we’re still going to miss 20%. Immunotherapy biomarker analysis may require tissue biopsies for a while. I think we can one day replace them with a liquid biopsy approach. I think that is better for a patient and is something we should do. But I don’t think tissue is going to go away soon.
TARGETED ONCOLOGY:How are PIPS and other digital slide technologies changing pathology?
Wistuba:I think the use of digital pathology to archive images is now part of the practice in many hospitals. We used to get histology glass slides, look at the microscope, make the diagnosis, and then send the slides to a warehouse. Now we are smarter than that. Instead of having an expensive warehouse with glass slides, we have digital images that we can go back and look at easily.
Secondly, we can use the images to make the diagnostics and make it convenient to look at the same area without having everybody in the room looking at the microscope or do consulting telepathology. I think that’s something we need to do, and this new FDA approval is allowing that. We need to train the next-generation pathologist to do that. However, this is not supposed to involve a diagnosis over a cell phone. People say they’re going to make diagnoses using cell phone images. No, you’re not going to do that. You have to do it properly.
The third benefit, as I see it, is to eventually use the images to quantify biomarkers. There is an FDA-approved image analysis system to quantify HER2 expression in breast cancer, but pathology does not use that. It uses the microscope. Pathologists still feel more confident doing it this way. I’ve done a lot of image analysis research in my laboratory that shows that imaging is more objective than a pathologist looking in a microscope.
TARGETED ONCOLOGY:How would this help a multidisciplinary approach?
Wistuba:
Gasparetto Explains Rationale for Quadruplet Front Line in Transplant-Ineligible Myeloma
February 22nd 2025In a Community Case Forum in partnership with the North Carolina Oncology Association, Cristina Gasparetto, MD, discussed the CEPHEUS, IMROZ, and BENEFIT trials of treatment for transplant-ineligible newly diagnosed multiple myeloma.
Read More
Key Trials From ASH 2024 Impact Treatment for Plasma Cell Disorders Going Forward
February 20th 2025Peers & Perspectives in Oncology editorial board member Marc J. Braunstein, MD, PhD, FACP, discussed the significant advancements in multiple myeloma treatment at the 2024 ASH Annual Meeting and Exposition.
Read More