Barriers to BRCA Mutation Testing Identified in the Community
The majority of community oncology practitioners test less than half of patients with early or metastatic breast cancer for germline BRCA1/2 mutations, according to the results of a recent survey by the Association of Community Cancer Centers. Further findings from the survey suggest that this could be due to issues with identifying patients would should be offered BRCA testing, patient concerns, and a lack of access to testing and genetic counseling.

The majority of community oncology practitioners test less than half of patients with early or metastatic breast cancer for germline BRCA1/2 mutations, according to the results of a recent survey by theAssociation of Community Cancer Centers(ACCC).1Further findings from the survey suggest that this could be due to issues with identifying patients would should be offered BRCA testing, patient concerns, and a lack of access to testing and genetic counseling.
Current National Comprehensive Cancer Network (NCCN) guidelines strongly support BRCA mutation testing for all patients with HER2-negative breast cancer who are eligible for single-agent therapy.2This recommendation stems from the approval earlier this year of the first PARP inhibitor, olaparib (Lynparza), for the treatment of breast cancer. PARP inhibitors have been found to be highly effective against tumors with BRCA mutations compared with chemotherapy, the current standard of care. Olaparib was approved specifically for patients with HER2-negative metastatic breast cancer harboring a deleterious germline BRCA mutation.
In addition to olaparib, the PARP inhibitor talazoparib was recently granted a priority review by the FDA for the treatment of patients with germline BRCA mutationpositive, HER2-negative locally advanced or metastatic breast cancer, based on findings from the phase III EMBRACA trial (NCT01945775).
Tom Gallo, MS, MDA, president of the ACCC, commented in a statement on the importance of testing, like BRCA mutation testing, for improving patient care: “Effective processes for the timely integration of molecular biomarker and genetic testing are increasingly recognized as a component of quality breast cancer care.”
With growing evidence supporting the role of BRCA genetic testing, the ACCC seeks to increase testing in the appropriate patients to improve treatment decisions in the community setting.
In March, the association conducted a survey of 95 community oncology practitioners across the United States to see the current status of BRCA testing in the community.
The survey found that a mere 7% of responders frequently ordered BRCA testing for all of their patients with early stage breast cancer and for 14% of their patients with metastatic breast cancer in the community setting.
Among patients with early breast cancer, BRCA testing was routinely ordered for 74% of patients below the age of 50 at diagnosis, 85% with a family history of a BRCA mutation, 86% with a family history of breast or ovarian cancer, and 75% of patients who had triple-negative breast cancer (TNBC).
Testing was routinely ordered for 64% of patients with metastatic disease under 50 years at diagnosis, 77% with a family history of the mutation, 79% with a family history of breast or ovarian cancer, and 65% with TNBC. Additionally, testing was often ordered for 40% of patients with metastatic disease who had not yet been tested and had progressed on several lines of therapy.
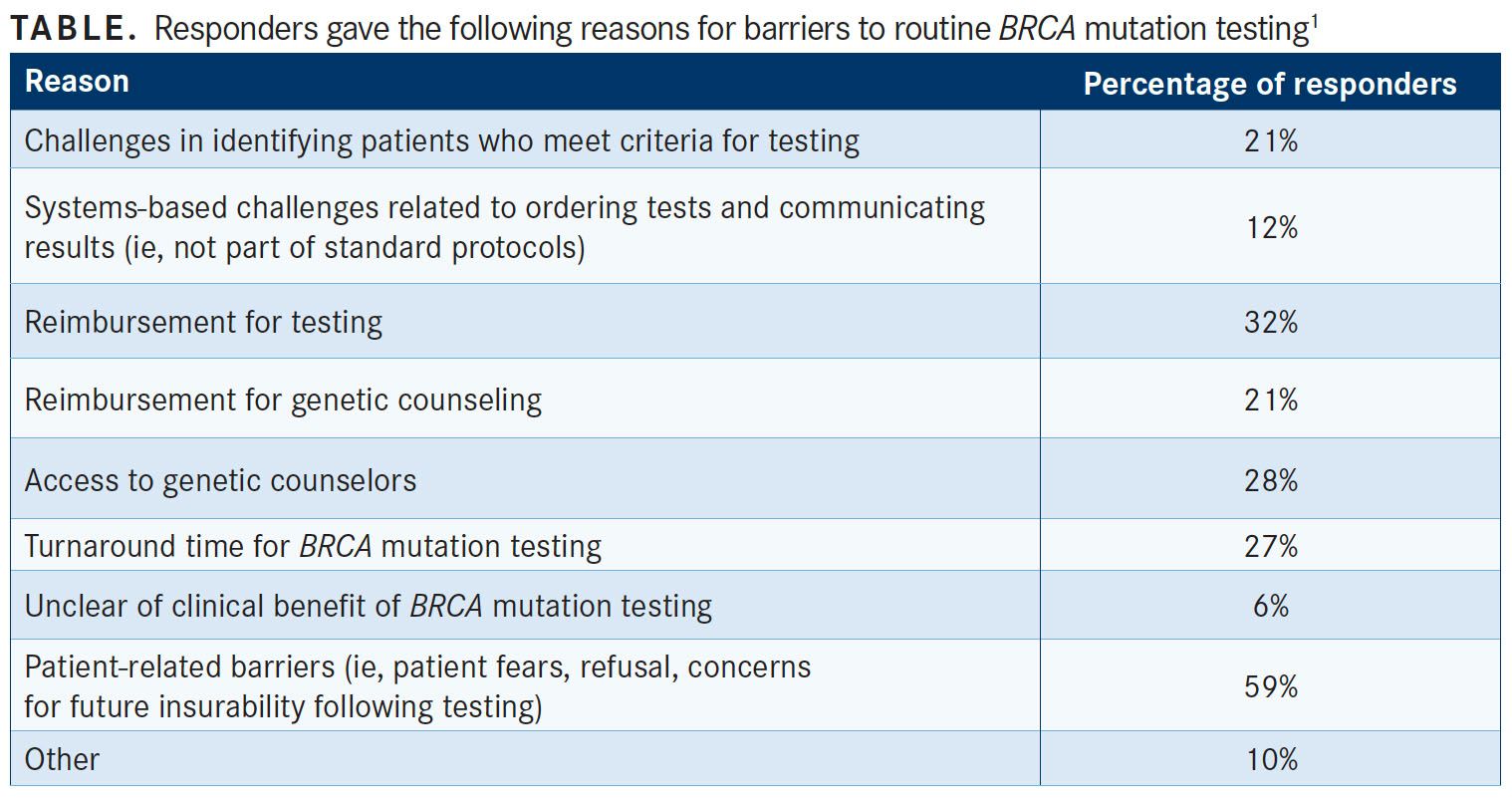
Barriers to routine BRCA mutation testing in the community setting were highlighted in the survey. The most common reasons were patient related (59%), including fear, refusal, and concerns for future insurance. Others were provider and institutional related, including payment for testing (32%), access to genetic counselors (28%), and turnaround time (27%). In addition, 21% of the responders reported struggling to identify patients that met BRCA testing criteria (TABLE).
Institutionally, one of the largest barriers identified was lack of access, either to resources, such as genetic counselors, or to provider education and experience. From the survey, 15% of the respondents reported having no access to, or routine use, of a genetic counselor. Most, however, did report utilizing a genetic counselor either onsite (69%) or through tele-counseling (16%).
Among those who documented having access to a genetic counselor, 75% reported waiting 2 weeks or less to get an appointment, with 25% waiting more than 2 weeks.
The turnaround time for germline BRCA test results was varied. Although 70% of respondents indicated they wait an average of less than 2 weeks to receive results, 31% typically wait more than 2 weeks. Turnaround time has been a common obstacle for the implementation of genetic testing in community patient care.
Despite these challenges, 95% of community practitioners who responded to the survey were at least somewhat familiar with the mechanism of action of PARP inhibitors in patients with metastatic breast cancer harboring BRCA1/2 mutations. Additionally, 67% noted that their practice prescribes PARP inhibitors to patients with metastatic breast cancer with BRCA mutations and about one-third had referred their patients to clinical trials of PARP inhibitors at other centers.
Most community oncologist practitioners (95%) reported utilizing the NCCN guidelines when administering germline BRCA mutation testing, although the survey generally recognized variation between practices in patient selection.
Other guidelines used by surveyed practitioners were those of the American Society of Clinical Oncology (31%) and the American Society of Breast Surgeons (17%). However, neither of these guidelines offers recommendations specific to BRCA testing. Three percent of the respondents admitted to following no specific guidelines.
In light of their recent survey, the ACCC has collaborated with Pfizer Independent Grants for Learning and Change to issue a request for proposals in support of quality improvement projects, with the goal of standardizing BRCA testing for patients with early or metastatic breast cancer. Pfizer plans to grant up to $1.5 million to fund at least 10 proposals.
References:
- Assessing the status of BRCA testing and the challenges faced by cancer care teams in the community. Association of Community Cancer Centers website. Posted May 14, 2018. accc-cancer.org/docs/projects/brca/brca-initiative_ survey-summary_05_14_18.pdf?sfvrsn=ad6a38ec_2. Accessed June 20, 2018.
- National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Breast Cancer. V1.2018. NCCN website. www.nccn.org/professionals/physician_gls/pdf/breast.pdf. Accessed June 20, 2018.
Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More
