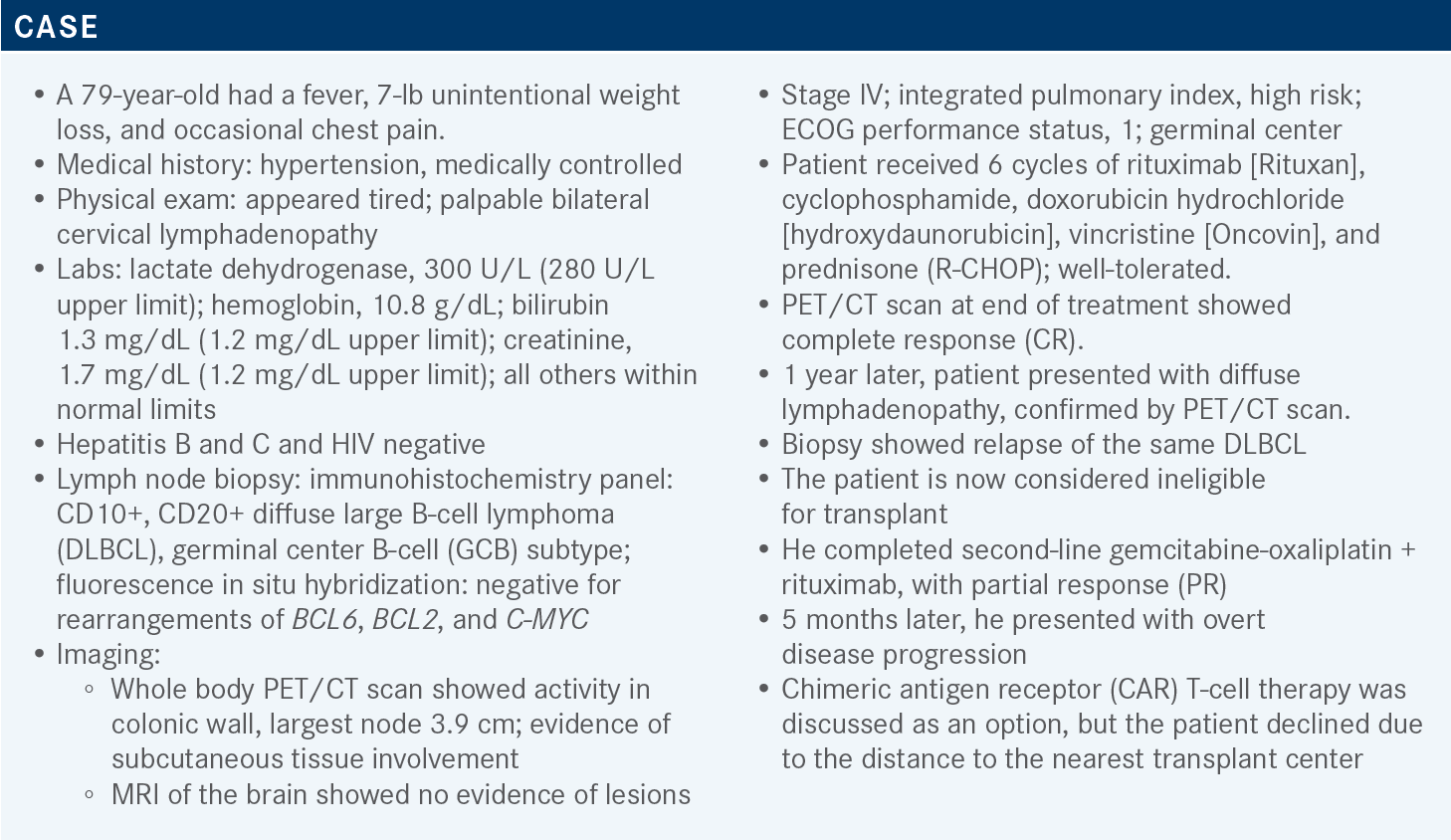
Yazbeck Considers the Use of New Approaches in Relapsed/Refractory DLBCL
During a Targeted Oncology case-based roundtable event, Victor Yazbeck, MD, MS, discussed the data from recent clinical trials of tafasitamab/lenalidomide, polatuzumab vedotin, and loncastuximab tesirine for patients with relapsed/refractory diffuse large B-cell lymphoma.
Victor Yazbeck, MD, MS
Associate Professor of Medicine
Director of Lymphoid Malignancies
Co-leader, Hematological Malignancies and Plasma Cell Neoplasm Disease Working Group
Massey Cancer Center
Virginia Commonwealth University
Richmond, VA

Targeted OncologyTM: What study data led to the approval of tafasitamab (Monjuvi) plus lenalidomide (Revlimid) in refractory or relapsed (R/R) DLBCL?
YAZBECK: Tafasitamab [MOR208] plus lenalidomide is approved based on the L-MIND study [NCT02399085], which looked at tafasitamab, an Fc-enhanced anti-CD19 monoclonal antibody. It has improved ADCC [antibody-dependent cellular cytotoxicity] and ADCP [antibody-dependent cellular phagocytosis], which are phagocytosis effects.
It acts by direct cell death and has encouraging single-agent activity, including in R/R DLBCL.1 Lenalidomide from the myeloma world is extensively studied. It’s an immunomodulator that affects T- and natural killer-cell activation or expansion [and] direct cell death and demonstrates activity as an antilymphoma agent. It is approved as a single-agent therapy for mantle cell lymphoma, and in combination with rituximab [R2] in follicular lymphoma and marginal zone lymphoma. In preclinical studies, both in vitro and in vivo, it showed a strong synergistic action, so that’s why they moved it to phase 1 and 2 clinical trials.
Based on the L-MIND study [findings, tafasitamab plus lenalidomide] was FDA approved in July 2020 for R/R DLBCL NOS [not otherwise specified], which includes those who had transformed from low-grade lymphoma who are not eligible for autologous stem cell transplant [ASCT].2 One can give this combination in second-line therapy. The other options of polatuzumab vedotin [Polivy] plus bendamustine [Treanda] and rituximab [pola-BR] and loncastuximab tesirine [Zynlonta] are for third-line therapy.
The L-MIND study included patients who had 1 to 3 prior lines of therapy, so they did not allow more than 3 prior lines of therapy. That’s important [in comparison with] the other studies. They had to be ineligible for ASCT and high-dose chemotherapy. The primary refractory patients were also excluded. So it’s a different patient population than [the ones] you see with the loncastuximab or pola-BR [studies].1
They gave, for the first 1 to 3 cycles, tafasitamab weekly at 12 mg/kg, then from cycle 4 to 12 it was given every 2 weeks. The lenalidomide starting dose was 25 mg, 3 weeks on, 1 week off. In cycle 1, the tafasitamab was loaded on day 4. After that, all those who achieved stable disease or better were put on tafasitamab maintenance every 2 weeks [until progression of disease].1
The primary end point of the study was overall response rate [ORR] and secondary were PFS [progression-free survival], duration of response [DOR], and overall survival [OS].1
For the patient characteristics, the median age was 72 [years], which is what you see in this patient population. The IPI [(International Prognostic Index) risk score] on the high end was 51%. The median prior lines of therapy was 2 and ranged from 1 to 4; [only 7% of patients had received more than] 3. Most of the patients had only 1 line of therapy. Keep that in mind. [Nineteen percent of] patients… were primary refractory…and 11% had prior ASCT.
The ORR was 57%, the complete response [CR] rate was 40%, and median DOR was close to 44 months. The median time to response was 2.1 months [range, 1.7-34.7].1,3
[At 33.9 months of follow-up], the median PFS was 11 months, and the median OS was 33.5 months after [42.7 months’ follow-up]; however, that’s for all patients. But those who achieved CR had more benefit from this combination for PFS and especially OS, [which were not reached].
Obviously it’s too early to say, but it would be nice to see a longer follow-up and see if that is maintained. Remember, this is what one would like to see in immunotherapy—a subset of patients who could potentially be cured.1,3
Were there any prognosticators as to who would achieve a CR? Had those patients received less prior treatment?
I’m not aware of such data. Remember, this is phase 2 alone but 50% of patients had only 1 prior line of treatment. I don’t know how many of the patients who achieved CR did so just after first-line therapy. Ideally, one wants to know who those [patients] are. Is there a specific biomarker that you can select them for? That’s the million-buck question, who are those patients, because they seem to do well with this combination.
What are the notable AEs from this treatment?
The most common AE was hematologic, specifically when you factor in lenalidomide. Neutropenia is the major thing at 27% grade 3 [and 21% grade 4], so [it's] close to 48% for both grades 3 and 4. Febrile neutropenia was around 12% [for grades 3 and 4].1,4 For nonhematologic AEs, the most common ones with more than 20% were fatigue, diarrhea, cough, fever, peripheral edema, UTIs [urinary tract infections], and decreased appetite. I think also for the rash, both tafasitamab and lenalidomide could give one that. It was 9% grade 3 and 27% for grades 1 and 2. Diarrhea was also common with this combination.1,4
The serious AEs were at 51% and those suspected to be treatment related were 19%. Discontinuation of [combination treatment] because of the AEs was 12%. Close to 46% of patients had to dose reduce the lenalidomide. Most patients, 77%, were able to maintain a lenalidomide dose of more than 20 mg per day over the duration of treatment.1,4
When they continued [tafasitamab monotherapy], I think there is no surprise [that the incidence and severity of treatment-emergent AEs], mainly neutropenia, decreased.1
Using real-world data, obviously tafasitamab plus lenalidomide was better than lenalidomide in OS and PFS, but these were not randomized data.5
What study data led to the approval of loncastuximab tesirine in R/R DLBCL?
Loncastuximab is an antibody-drug conjugate targeting CD19. It’s using the linker to deliver SG3199, a cytotoxic DNA minor groove interstrand crosslinking pyrrolobenzodiazepine dimer payload. So it’s delivering this targeted chemotherapy to the tumor. It was approved as a single agent in April 2021 for DLBCL after 2 lines of systemic therapy. This includes DLBCL NOS, DLBCL arising from low-grade lymphoma, and high-grade B-cell lymphoma including double-hit lymphoma, which is not seen in the other drugs.6
[Results from] the LOTIS-2 study [NCT03589469] led to its approval. It was done in patients with R/R DLBCL and had broader inclusion criteria. They allowed patients who [received] ASCT and were primary refractory, so high-risk patients. Also, those with double-hit lymphoma were allowed. Loncastuximab was given for the first 2 cycles every 3 weeks as a 30-minute infusion at a dose of 150 μg/kg. After that they [received] 75 μg/kg continued for up to 1 year of treatment.7
For the patient characteristics, the median age was 66 and they had high-risk features. The double- and triple-hit [rate] was 10%; the double and triple expressors, 14%; and transformed disease, 20%. The median number of prior lines of systemic therapy was 3, with [32%] of patients having more than 3 prior lines of therapy.
They had a lot of relapsed [and refractory] disease; 20% were refractory to first-line therapy and 58% were refractory to the last-line treatment. [Nine percent of] patients [had] prior CAR T-cell therapy. Post CAR T-cell therapy patients are hard to treat and there is an unmet need there. The ORR was 48%, with half [of patients having] CR and the other half PR. The median time to first response was 41 days. Of the 35 who achieved CR, 57% maintained this at the data cut-off point. Most patients achieved a response after 2 cycles, and this is when the scans were done. On average, patients got 4.5 loncastuximab cycles.
The high-risk groups, defined as transformed disease and double-hit lymphoma, seemed to respond or benefit. The ORR in the double-hit group was close to 33%, still high for this disease. For the transformed group, whether de novo [disease] or not, the ORR was close to 50%.
In the cell-of-origin subgroup, there was not much difference between the GCB-[like] and ABC [activated B-cell–like] groups. The primary mediastinal group, which is [in the World Health Organization classification], had a lower ORR [at 14.3%] compared with the high-grade B-cell lymphoma and DLBCL NOS [groups, which had 45.5% and 50.4%, respectively]. Based on this, the label [for loncastuximab] did not include primary mediastinal B-cell lymphoma, but also the subgroup had a low number of patients.7
Those who had prior ASCT still had a good response at 58% and those with prior CAR T-cell therapy still responded at over 45%, so whatever line of therapy they [had] in the past, they had the same ORR. It’s an effective regimen in highly pretreated populations [and including patients] post CAR T-cell therapy.
Now, these are phase 2 data so fewer patients [are included], but this is the only trial with post CAR T-cell therapy data. They also permitted both transplant-eligible and -ineligible patients. The median DOR, updated in March 2021, was 13.4 months, but for patients who achieved CR, it was not reached.
The median PFS was 5.1 months [95% CI, 2.9-8.3] and median OS was 9.5 months [95% CI, 6.9-11.3]. Obviously, you need more follow-up, but again it is always good to see the subset of patients who might derive long-term benefit. It is important to mention that 15 patients received CAR T-cell therapy after getting loncastuximab and their ORR was 46%. So [the rate is] lower than what you get with prior CAR T-cell therapy, which was around 60% to 80%, and 9 patients received an ASCT consolidation after responding to loncastuximab.
Whether one was younger than 65 [years] or above [age] 65, the AE profile was similar. That’s a good thing. The major AEs were an increase in gamma-glutamyl transferase and peripheral edema, which is usually not responsive to furosemide [Lasix] and is typically treated with spironolactone [Aldactone].
Patients are given dexamethasone the day prior, the day of therapy, and the day after, so for 3 days. If they forget to take it the day before, we give it on the day of therapy 2 hours or more prior to getting loncastuximab.7 Dose [modification can be done based on] the package insert following toxicity.8
What else can you tell us that is striking about these data?
[All the trials that led to the approval of pola-BR, tafasitamab plus lenalidomide, and loncastuximab] were phase 2, none of them were phase 3. There is no randomization between one or the other to say what is different between them, but from the eligibility criteria, pola-BR patients were transplant ineligible or had treatment failure with prior ASCT. The pola-BR study allowed more than 1 prior line of treatment and had a median of 2 lines.9
The L-MIND study had a median of 2 [prior lines] and it only allowed up to 3 prior therapy lines and [patients] were not eligible for ASCT. The LOTIS-2 study allowed more than 3 prior lines of therapy and the median was 3; patients had to have been CD19 positive if they [had received] CAR T-cell therapy in the past, and they allowed patients who were post autologous and allogeneic SCT.1,7
REFERENCES
1. Salles G, Duell J, González Barca E, et al. Tafasitamab plus lenalidomide in relapsed or refractory diffuse large B-cell lymphoma (L-MIND): a multicentre, prospective, single-arm, phase 2 study. Lancet Oncol. 2020;21(7):978-988. doi:10.1016/S1470-2045(20)30225-4
2. FDA grants accelerated approval to tafasitamab-cxix for diffuse large B-cell lymphoma. FDA. Updated August 3, 2020. Accessed March 21, 2022. https:// bit.ly/37O1pGB
3. Duell J, Maddocks KJ, González-Barca E, et al. Long-term outcomes from the phase II L-MIND study of tafasitamab (MOR208) plus lenalidomide in patients with relapsed or refractory diffuse large B-cell lymphoma. Haematologica. 2021;106(9):2417-2426. doi:10.3324/haematol.2020.275958
4. Monjuvi. Prescribing information. MorphoSys US Inc; 2020. Accessed March 30, 2022. https://bit.ly/2S38ZW7
5. Zinzani PL, Rodgers T, Marino D, et al. RE-MIND: Comparing tafasitamab + lenalidomide (L-MIND) with a real-world lenalidomide monotherapy cohort in relapsed or refractory diffuse large B-cell lymphoma. Clin Cancer Res. 2021;27(22):6124-6134. doi:10.1158/1078-0432.CCR-21-1471
6. Zammarchi F, Corbett S, Adams L, et al. ADCT-402, a PBD dimer-containing antibody drug conjugate targeting CD19-expressing malignancies. Blood. 2018;131(10):1094-1105. doi:10.1182/blood-2017-10-813493
7. Caimi PF, Ai W, Alderuccio JP, et al. Loncastuximab tesirine in relapsed or refractory diffuse large B-cell lymphoma (LOTIS-2): a multicentre, open-label, single-arm, phase 2 trial. Lancet Oncol. 2021;22(6):790-800. doi:10.1016/ S1470-2045(21)00139-X
8. Zynlonta. Prescribing information. ADC Therapeutics, SA; 2021. Accessed MArch 30, 2022. https://bit.ly/3qq9YOm
9. Sehn LH, Herrera AF, Flowers CR, et al. Polatuzumab vedotin in relapsed or refractory diffuse large B-cell lymphoma. J Clin Oncol. 2020;38(2):155-165. doi:10.1200/JCO.19.00172